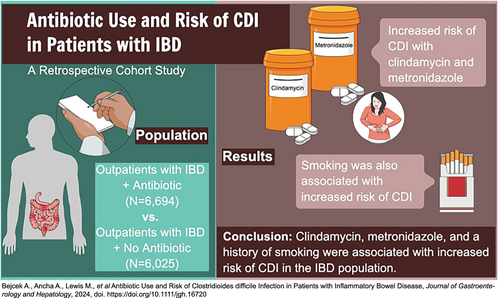
Antibiotic use and risk of Clostridioides difficile infection in patients with inflammatory bowel disease
Declaration of conflict of interest: The authors have no conflicts of interest to disclose.
Informed consent: Not applicable.
Financial support: Support was provided through internal funding from the Baylor Scott & White Research Institute.
Clinical trial registration: This study was not registered within a clinical trial.
Abstract
Background and Aim
Patients with inflammatory bowel disease (IBD) have an increased risk of Clostridioides difficile infection (CDI) compared with those without IBD, which is worsened with antibiotic usage. While prior studies have shown a correlation between CDI development and certain classes of antibiotics, the IBD population has not been well represented. This study evaluates the rates of CDI with outpatient antibiotic use in patients with IBD.
Methods
We conducted a retrospective cohort study composed of patients with IBD and compared the incidence of CDI in patients who received an outpatient prescription for antibiotics (6694 patients) against those without prescriptions (6025 patients) from 2014 to 2020 at our institution. We compared CDI rates based on nine antibiotic classes: penicillins, cephalosporins, sulfonamides, tetracyclines, macrolides, quinolones, clindamycin, metronidazole, and nitrofurantoin.
Results
The risk of CDI was low (0.7%) but significantly higher for those with antibiotic exposure (0.9% vs 0.5%, P = 0.005) and had a positive correlation with a smoking history. The increased risk of CDI in the IBD population was attributable to the clindamycin and metronidazole classes (odds ratio = 4.7, 95% confidence interval: 1.9–11.9, P = 0.001; odds ratio = 3.6, 95% confidence interval: 2.1–6.2, P < 0.0001, respectively).
Conclusions
The use of clindamycin or metronidazole prescribed in an outpatient setting was associated with a statistically significant increased risk of CDI in patients with IBD. Although the association between clindamycin and CDI is a well-established and common finding, the association between metronidazole and CDI is unique in this study.
Graphical Abstract
Open Research
Data availability statement
The data collected and used for this manuscript are readily available per request. Please contact the corresponding author for details.