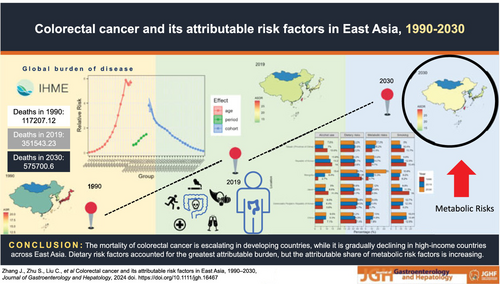
Colorectal cancer and its attributable risk factors in East Asia, 1990–2030
Jian Zhang
Department of Neurosurgery, Shengjing Hospital of China Medical University, Shenyang, China
Department of Neurosurgery, the Seventh Clinical College of China Medical University, Fushun, China
Jian Zhang, Shijie Zhu, and Chunlong Liu are co-first authors who contributed equally to this paper.
Search for more papers by this authorCorresponding Author
Shijie Zhu
Department of Occupational and Environmental Health, School of Public Health, Wuhan University, Wuhan, China
Jian Zhang, Shijie Zhu, and Chunlong Liu are co-first authors who contributed equally to this paper.
Correspondence
Shijie Zhu, Department of Occupational and Environmental Health, School of Public Health, Wuhan University, Wuhan 430071, China.
Email: [email protected]
Yang Hong, Department of Neurosurgery, Shengjing Hospital of China Medical University, Shenyang 110004, China.
Email: [email protected]
Search for more papers by this authorChunlong Liu
Department of Hepatobiliary and Pancreatic Surgery, Fuyang People's Hospital, Anhui Medical University, Fuyang, China
Jian Zhang, Shijie Zhu, and Chunlong Liu are co-first authors who contributed equally to this paper.
Search for more papers by this authorXiong Xiao
Department of Neurosurgery, Shengjing Hospital of China Medical University, Shenyang, China
Search for more papers by this authorHaojie Xie
Department of Neurosurgery, Shengjing Hospital of China Medical University, Shenyang, China
Search for more papers by this authorYonghui Zhang
Department of Neurosurgery, the Seventh Clinical College of China Medical University, Fushun, China
Search for more papers by this authorCorresponding Author
Yang Hong
Department of Neurosurgery, Shengjing Hospital of China Medical University, Shenyang, China
Correspondence
Shijie Zhu, Department of Occupational and Environmental Health, School of Public Health, Wuhan University, Wuhan 430071, China.
Email: [email protected]
Yang Hong, Department of Neurosurgery, Shengjing Hospital of China Medical University, Shenyang 110004, China.
Email: [email protected]
Search for more papers by this authorJian Zhang
Department of Neurosurgery, Shengjing Hospital of China Medical University, Shenyang, China
Department of Neurosurgery, the Seventh Clinical College of China Medical University, Fushun, China
Jian Zhang, Shijie Zhu, and Chunlong Liu are co-first authors who contributed equally to this paper.
Search for more papers by this authorCorresponding Author
Shijie Zhu
Department of Occupational and Environmental Health, School of Public Health, Wuhan University, Wuhan, China
Jian Zhang, Shijie Zhu, and Chunlong Liu are co-first authors who contributed equally to this paper.
Correspondence
Shijie Zhu, Department of Occupational and Environmental Health, School of Public Health, Wuhan University, Wuhan 430071, China.
Email: [email protected]
Yang Hong, Department of Neurosurgery, Shengjing Hospital of China Medical University, Shenyang 110004, China.
Email: [email protected]
Search for more papers by this authorChunlong Liu
Department of Hepatobiliary and Pancreatic Surgery, Fuyang People's Hospital, Anhui Medical University, Fuyang, China
Jian Zhang, Shijie Zhu, and Chunlong Liu are co-first authors who contributed equally to this paper.
Search for more papers by this authorXiong Xiao
Department of Neurosurgery, Shengjing Hospital of China Medical University, Shenyang, China
Search for more papers by this authorHaojie Xie
Department of Neurosurgery, Shengjing Hospital of China Medical University, Shenyang, China
Search for more papers by this authorYonghui Zhang
Department of Neurosurgery, the Seventh Clinical College of China Medical University, Fushun, China
Search for more papers by this authorCorresponding Author
Yang Hong
Department of Neurosurgery, Shengjing Hospital of China Medical University, Shenyang, China
Correspondence
Shijie Zhu, Department of Occupational and Environmental Health, School of Public Health, Wuhan University, Wuhan 430071, China.
Email: [email protected]
Yang Hong, Department of Neurosurgery, Shengjing Hospital of China Medical University, Shenyang 110004, China.
Email: [email protected]
Search for more papers by this authorAbstract
Background
The disease burden of colorectal cancer in East Asia has been at a high level. However, the epidemiological characteristics of the disease burden in this region have not been systematically studied.
Method
Data were obtained from the Global Burden of Disease 2019 program. Joinpoint analysis was used to identify long-term trends in mortality of colorectal cancer. Independent effects of age, period, and cohort were detected by the age–period–cohort model. The Bayesian age–period–cohort model was performed to predict the burden of colorectal cancer across East Asia by 2030.
Results
From 1990 to 2019, the average annual percentage change (AAPC) showed upward trends in mainland China (1.05 [95% confidence interval (CI)], 0.82, 1.28) as well as Taiwan Province of China (1.81 [95% CI], 1.51, 2.10) but downward in Japan (−0.60 [95% CI], −0.70, −0.49) (P < 0.05). Attributable risk factors for colorectal cancer in East Asia remained stable over 30 years, while the risk of metabolic factors is noteworthy in the future. In the next decade, the age-standardized death rate (ASDR) of colorectal cancer in China was predicted to surpass that of Japan and South Korea in expectation.
Conclusion
The mortality of colorectal cancer is escalating in developing countries, while it is gradually declining in high-income countries across East Asia. Nonetheless, the disease burden of colorectal cancer in high-income countries remains substantial level.
Graphical Abstract
Open Research
Data availability statement
The GBD in 2019 provides comprehensive data on the burden of diseases and risk factors across 204 countries and territories. Accessing this data is made possible through the GHDx query tool (http://ghdx.healthdata.org/gbd-results-tool), which is maintained by the Institute for Health Metrics and Evaluation.
Supporting Information
| Filename | Description |
|---|---|
| jgh16467-sup-0001-Supplementary Materials.pdfPDF document, 3.1 MB |
Table S1. The deaths and age-standardized death rate of colorectal cancer in East Asia, in 1990 and 2019, by countries and gender. Table S2. The age-specific death rate (longitudinal age curve) in East Asia, by countries and gender. Table S3. The period risk ratio in East Asia, by countries and gender. Table S4. The cohort risk ratio in East Asia, by countries and gender. Table S5. The projections of death number, age-standardized death rate and population attribution fraction (PAF) for colorectal cancer attributed to risk factors, 1990, 2019 and 2030. Table S6. The projections of death number, age-standardized death rate for colorectal cancer, 1990–2030. Figure S1. The age-specific death rate (longitudinal age curve) in East Asia, by countries and gender. (A. China-male; B. China-female; C. Japan-male; D. Japan-female; E. Democratic People's Republic of Korea-male; F. Democratic People's Republic of Korea-female; G. Republic of Korea-male; H. Republic of Korea-female; I. Mongolia-male; J. Mongolia-female; K. Taiwan (Province of China)-male; L. Taiwan (Province of China)-female). Figure S2. The period risk ratio in East Asia, by countries and gender. (A. China-male; B. China-female; C. Japan-male; D. Japan-female; E. Democratic People's Republic of Korea-male; F. Democratic People's Republic of Korea-female; G. Republic of Korea-male; H. Republic of Korea-female; I. Mongolia-male; J. Mongolia-female; K. Taiwan (Province of China)-male; L. Taiwan (Province of China)-female). Figure S3. The cohort risk ratio in East Asia, by countries and gender. (A. China-male; B. China-female; C. Japan-male; D. Japan-female; E. Democratic People's Republic of Korea-male; F. Democratic People's Republic of Korea-female; G. Republic of Korea-male; H. Republic of Korea-female; I. Mongolia-male; J. Mongolia-female; K. Taiwan (Province of China)-male; L. Taiwan (Province of China)-female). Figure S4A. Deaths and age-standardized mortality from colorectal cancer attributable to low-calcium diets in East Asia, 2020–2030. Figure S4B. Deaths and age-standardized mortality from colorectal cancer attributable to low-milk diets in East Asia, 2020–2030. Figure S4C. Deaths and age-standardized mortality from colorectal cancer attributable to low whole-grain diets in East Asia, 2020–2030. Figure S4D. Deaths and age-standardized mortality from colorectal cancer attributable to low physical activity in East Asia, 2020–2030. Figure S4E. Deaths and age-standardized mortality from colorectal cancer attributable to low-fiber diets in East Asia, 2020–2030. Figure S4F. Deaths and age-standardized mortality from colorectal cancer attributable to high body mass index in East Asia, 2020–2030. Figure S4G. Deaths and age-standardized mortality from colorectal cancer attributable to high red-meat diets in East Asia, 2020–2030. Figure S4H. Deaths and age-standardized mortality from colorectal cancer attributable to high processed-meat diets in East Asia, 2020–2030. Figure S4I. Deaths and age-standardized mortality from colorectal cancer attributable to high fasting plasma glucose in East Asia, 2020–2030. Figure S4J. Deaths and age-standardized mortality from colorectal cancer attributable to smoking in East Asia, 2020–2030. Figure S4K. Deaths and age-standardized mortality from colorectal cancer attributable to alcohol use in East Asia, 2020–2030. |
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
References
- 1 GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 2020; 396: 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9
- 2Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut 2017; 66: 683–691. https://doi.org/10.1136/gutjnl-2015-310912
- 3 GBD 2019 Colorectal Cancer Collaborators. Global, regional, and national burden of colorectal cancer and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Gastroenterol Hepatol 2022; 7: 627–647. https://doi.org/10.1016/S2468-1253(22)00044-9
- 4Labianca R, Nordlinger B, Beretta GD et al. Early colon cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2013; 24: vi64–vi72. https://doi.org/10.1093/annonc/mdt354
- 5Sung H, Ferlay J, Siegel RL et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71: 209–249. https://doi.org/10.3322/caac.21660
- 6Ferlay J, Soerjomataram I, Dikshit R et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015; 136: E359–E386. https://doi.org/10.1002/ijc.29210
- 7Doubeni CA, Major JM, Laiyemo AO et al. Contribution of behavioral risk factors and obesity to socioeconomic differences in colorectal cancer incidence. JNCI: J Natl Cancer Inst 2012; 104: 1353–1362. https://doi.org/10.1093/jnci/djs346
- 8Zhou J, Zheng R, Zhang S et al. Colorectal cancer burden and trends: comparison between China and major burden countries in the world. Chin J Cancer Res 2021; 33: 1–10. https://doi.org/10.21147/j.issn.1000-9604.2021.01.01
- 9Li N, Lu B, Luo C et al. Incidence, mortality, survival, risk factor and screening of colorectal cancer: a comparison among China, Europe, and northern America. Cancer Lett 2021; 522: 255–268. https://doi.org/10.1016/j.canlet.2021.09.034
- 10 GBD 2017 Colorectal Cancer Collaborators. The global, regional, and national burden of colorectal cancer and its attributable risk factors in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 2019; 4: 913–933. https://doi.org/10.1016/S2468-1253(19)30345-0
- 11Buccafusca G, Proserpio I, Tralongo AC, Rametta Giuliano S, Tralongo P. Early colorectal cancer: diagnosis, treatment and survivorship care. Crit Rev Oncol Hematol 2019; 136: 20–30. https://doi.org/10.1016/j.critrevonc.2019.01.023
- 12Akter S, Islam Z, Mizoue T et al. Smoking and colorectal cancer: a pooled analysis of 10 population-based cohort studies in Japan. Int J Cancer 2021; 148: 654–664. https://doi.org/10.1002/ijc.33248
- 13Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000; 19: 335–351. https://doi.org/10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z
10.1002/(SICI)1097-0258(20000215)19:3<335::AID-SIM336>3.0.CO;2-Z CAS PubMed Web of Science® Google Scholar
- 14Rosenberg PS, Check DP, Anderson WF. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev 2014; 23: 2296–2302. https://doi.org/10.1158/1055-9965.EPI-14-0300
- 15Liu Y, Zhang C, Wang Q et al. Temporal trends in the disease burden of colorectal cancer with its risk factors at the global and national level from 1990 to 2019, and projections until 2044. Clin Epidemiol 2023; 15: 55–71. https://doi.org/10.2147/CLEP.S388323
- 16 GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 2020; 396: 1223–1249. https://doi.org/10.1016/S0140-6736(20)30752-2
- 17 GBD 2020 Alcohol Collaborators. Population-level risks of alcohol consumption by amount, geography, age, sex, and year: a systematic analysis for the global burden of disease study 2020. Lancet 2022; 400: 185–235. https://doi.org/10.1016/S0140-6736(22)00847-9
- 18Burnett RT, Pope CA, Ezzati M et al. An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environ Health Perspect 2014; 122: 397–403. https://doi.org/10.1289/ehp.1307049
- 19Li X, Cao X, Guo M, Xie M, Liu X. Trends and risk factors of mortality and disability adjusted life years for chronic respiratory diseases from 1990 to 2017: systematic analysis for the global burden of disease study 2017. BMJ 2020; 368: m234. https://doi.org/10.1136/bmj.m234
- 20 GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. Lancet 2018; 392: 1736–1788. https://doi.org/10.1016/S0140-6736(18)32203-7
- 21Robertson C, Gandini S, Boyle P. Age-period-cohort models: a comparative study of available methodologies. J Clin Epidemiol 1999; 52: 569–583. https://doi.org/10.1016/s0895-4356(99)00033-5
- 22Zhu S, Zhang F, Zhao G et al. Trends in the global burden of oral cancer joint with attributable risk factors: results from the global burden of disease study 2019. Oral Oncol 2022; 134: 106189. https://doi.org/10.1016/j.oraloncology.2022.106189
- 23Yu J, Yang X, He W, Ye W. Burden of pancreatic cancer along with attributable risk factors in Europe between 1990 and 2019, and projections until 2039. Int J Cancer 2021; 149: 993–1001. https://doi.org/10.1002/ijc.33617
- 24Liu Z, Xu K, Jiang Y et al. Global trend of aetiology-based primary liver cancer incidence from 1990 to 2030: a modelling study. Int J Epidemiol 2021; 50: 128–142. https://doi.org/10.1093/ije/dyaa196
- 25Knoll M, Furkel J, Debus J, Abdollahi A, Karch A, Stock C. An R package for an integrated evaluation of statistical approaches to cancer incidence projection. BMC Med Res Methodol 2020; 20: 257. https://doi.org/10.1186/s12874-020-01133-5
- 26Janz T, Lu K, Povlow MR, Urso B. A review of colorectal cancer detection modalities, stool DNA, and fecal immunochemistry testing in adults over the age of 50. Cureus 2016; 8: e931. https://doi.org/10.7759/cureus.931
- 27Bérnard F, Barkun AN, Martel M, von Renteln D. Systematic review of colorectal cancer screening guidelines for average-risk adults: summarizing the current global recommendations. World J Gastroenterol 2018; 24. https://doi.org/10.3748/wjg.v24.i1.124
- 28Edwards BK, Ward E, Kohler BA et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 2010; 116: 544–573. https://doi.org/10.1002/cncr.24760
- 29Onyoh EF, Hsu WF, Chang LC, Lee YC, Wu MS, Chiu HM. The rise of colorectal cancer in Asia: epidemiology, screening, and management. Curr Gastroenterol Rep 2019; 21: 36. https://doi.org/10.1007/s11894-019-0703-8
- 30Schreuders EH, Ruco A, Rabeneck L et al. Colorectal cancer screening: a global overview of existing programmes. Gut 2015; 64: 1637–1649. https://doi.org/10.1136/gutjnl-2014-309086
- 31Levin B, Lieberman DA, McFarland B et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology 2008; 134: 1570–1595. https://doi.org/10.1053/j.gastro.2008.02.002
- 32Wong MCS, John GK, Hirai HW et al. Changes in the choice of colorectal cancer screening tests in primary care settings from 7,845 prospectively collected surveys. Cancer Causes Control 2012; 23: 1541–1548. https://doi.org/10.1007/s10552-012-0031-x
- 33Song M, Chan AT, Sun J. Influence of the gut microbiome, diet, and environment on risk of colorectal cancer. Gastroenterology 2020; 158: 322–340. https://doi.org/10.1053/j.gastro.2019.06.048
- 34Bardou M, Barkun AN, Martel M. Obesity and colorectal cancer. Gut 2013; 62: 933–947. https://doi.org/10.1136/gutjnl-2013-304701
- 35Kono S, Ahn YO. Vegetables, cereals and colon cancer mortality: long-term trend in Japan. Eur J Cancer Prev 2000; 9: 363–365. https://doi.org/10.1097/00008469-200010000-00011
- 36Kono S. Secular trend of colon cancer incidence and mortality in relation to fat and meat intake in Japan. Eur J Cancer Prev 2004; 13: 127–132. https://doi.org/10.1097/00008469-200404000-00006
- 37Béjar LM, Gili M, Infantes B, Marcott PF. Incidence of colorectal cancer and influence of dietary habits in fifteen European countries from 1971 to 2002. Gac Sanit 2012; 26: 69–73. https://doi.org/10.1016/j.gaceta.2011.04.016
- 38Chan DSM, Lau R, Aune D et al. Red and processed meat and colorectal cancer incidence: meta-analysis of prospective studies. PLoS ONE 2011; 6: e20456. https://doi.org/10.1371/journal.pone.0020456
- 39Newmark HL, Wargovich MJ, Bruce WR. Colon cancer and dietary fat, phosphate, and calcium: a hypothesis. J Natl Cancer Inst 1984; 72: 1323–1325.
- 40Lamprecht SA, Lipkin M. Cellular mechanisms of calcium and vitamin D in the inhibition of colorectal carcinogenesis. Ann N Y Acad Sci 2001; 952: 73–87. https://doi.org/10.1111/j.1749-6632.2001.tb02729.x
- 41Ralston RA, Truby H, Palermo CE, Walker KZ. Colorectal cancer and nonfermented milk, solid cheese, and fermented milk consumption: a systematic review and meta-analysis of prospective studies. Crit Rev Food Sci Nutr 2014; 54: 1167–1179. https://doi.org/10.1080/10408398.2011.629353
- 42Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev 2012; 70: 3–21. https://doi.org/10.1111/j.1753-4887.2011.00456.x
- 43Tárraga López PJ, Albero JS, Rodríguez-Montes JA. Primary and secondary prevention of colorectal cancer. Clin Med Insights Gastroenterol 2014; 7: 33–46. https://doi.org/10.4137/CGast.S14039
- 44Young JP, Win AK, Rosty C et al. Rising incidence of early-onset colorectal cancer in Australia over two decades: report and review. J Gastroenterol Hepatol 2015; 30: 6–13. https://doi.org/10.1111/jgh.12792
- 45Wolin KY, Yan Y, Colditz GA, Lee IM. Physical activity and colon cancer prevention: a meta-analysis. Br J Cancer 2009; 100: 611–616. https://doi.org/10.1038/sj.bjc.6604917
- 46Fedirko V, Tramacere I, Bagnardi V et al. Alcohol drinking and colorectal cancer risk: an overall and dose-response meta-analysis of published studies. Ann Oncol 2011; 22: 1958–1972. https://doi.org/10.1093/annonc/mdq653
- 47Vieira AR, Abar L, Chan DSM et al. Foods and beverages and colorectal cancer risk: a systematic review and meta-analysis of cohort studies, an update of the evidence of the WCRF-AICR continuous update project. Ann Oncol 2017; 28: 1788–1802. https://doi.org/10.1093/annonc/mdx171
- 48Millwood IY, Li L, Smith M et al. Alcohol consumption in 0.5 million people from 10 diverse regions of China: prevalence, patterns and socio-demographic and health-related correlates. Int J Epidemiol 2013; 42: 816–827. https://doi.org/10.1093/ije/dyt078
- 49Cochrane J, Chen H, Conigrave KM, Hao W. Alcohol use in China. Alcohol Alcohol 2003; 38: 537–542. https://doi.org/10.1093/alcalc/agg111
- 50Jiang H, Room R, Hao W. Alcohol and related health issues in China: action needed. Lancet Glob Health 2015; 3: e190–e191. https://doi.org/10.1016/S2214-109X(15)70017-3
- 51Yang JJ, Yu D, Wen W et al. Tobacco smoking and mortality in Asia: a pooled meta-analysis. JAMA Netw Open 2019; 2: e191474. https://doi.org/10.1001/jamanetworkopen.2019.1474
- 52Karastergiou K, Smith SR, Greenberg AS, Fried SK. Sex differences in human adipose tissues - the biology of pear shape. Biol Sex Differ 2012; 3: 13. https://doi.org/10.1186/2042-6410-3-13
- 53Mori N, Keski-Rahkonen P, Gicquiau A et al. Endogenous circulating sex hormone concentrations and colon cancer risk in postmenopausal women: a prospective study and meta-analysis. JNCI Cancer Spectr 2021; 5: pkab084. https://doi.org/10.1093/jncics/pkab084
- 54Fernandez E, La Vecchia C, Balducci A, Chatenoud L, Franceschi S, Negri E. Oral contraceptives and colorectal cancer risk: a meta-analysis. Br J Cancer 2001; 84: 722–727. https://doi.org/10.1054/bjoc.2000.1622
- 55Cho MY, Siegel DA, Demb J, Richardson LC, Gupta S. Increasing colorectal cancer incidence before and after age 50: implications for screening initiation and promotion of “on-time” screening. Dig Dis Sci 2022; 67: 4086–4091. https://doi.org/10.1007/s10620-021-07213-w
- 56Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013-2016. JAMA 2018; 319: 2410–2418. https://doi.org/10.1001/jama.2018.5158
- 57Modest DP, Pant S, Sartore-Bianchi A. Treatment sequencing in metastatic colorectal cancer. Eur J Cancer 2019; 109: 70–83. https://doi.org/10.1016/j.ejca.2018.12.019
- 58Gelmann A, Desnoyers R, Cagir B, Weinberg D, Boman BM, Waldman SA. Colorectal cancer staging and adjuvant chemotherapy. Expert Opin Pharmacother 2000; 1: 737–755. https://doi.org/10.1517/14656566.1.4.737