Psychosocial and mental impact of alopecia areata: Analysis of the Danish Skin Cohort
Abstract
Importance
Alopecia areata (AA) carries a psychological burden for patients beyond hair loss. However, quality-of-life measurement tools such as EQ-5D used in clinical trials may not adequately capture the burden of AA, the perceived stigmatization or the psychosocial impact of AA.
Objective
To investigate the potential association between disease severity and the degree of social isolation, perceived stigmatization, anxiety and depression, alcohol consumption and work absenteeism using multiple PRO measures in patients with AA.
Design, Setting and Participants
Using the Danish Skin Cohort, the study included adult patients diagnosed with AA. The study included multiple PRO measures, including Skindex-16, EQ-5D-5L, Work Productivity and Activity Impairment (WPAI), Alcohol Use Disorders Identification Test-Consumption (AUDIT-C) and the Alopecia Areata Symptom Impact Scale (AASIS). The questionnaires were dispatched to the patients in January 2023. The severity of AA was determined based on scalp involvement using a modified Alopecia Areata Scale. Multiple multivariate linear regressions were conducted using Skindex-16, AASIS and WPAI, while multivariate logistic regressions were applied to HADS, AUDIT-C and EQ-5D-5L.
Results
A total of 376 patients were included, of which 177 (47%) had severe disease, 41 (11%) had moderate disease, 94 (25%) had mild disease, and 64 (17%) were in remission. The median age of patients was 55 (IQR, 47–66 years) and most were female (70%). Skindex-16 and AASIS were the only PRO measures able to distinguish between severity. For these scores, moderate and severe diseases, female sex, and involvement of eyebrows increased the score and negatively impacted patient quality of life.
Conclusion and Relevance
The results indicate the importance of using the proper tool for the intended measurement of quality of life and that factors such as the severity of AA, as well as female sex and involvement of the eyebrows, may potentially increase the psychosocial burden of AA.
INTRODUCTION
Alopecia areata (AA) is an autoimmune disease with an unpredictable prognosis characterized by transient nonscarring hair loss with preservation of hair follicles and with a broad range of hair involvment.1, 2 The prevalence of AA is estimated to be around 0.2%, and the incidence risk is between 0.57% and 3.8%.1, 3-7 There is no exact consensus on the definition of AA disease severity, and in most assessments, the psychosocial impact caused by AA or symptoms different from scalp hair loss, are not considered when defining AA severity.8-10
Although various skin conditions are associated with impaired mental health, AA carries a significant psychological burden for patients beyond hair loss and is associated with a negative impact on the health-related quality of life (HRQoL) and social functioning.7, 11-17 This includes being harassed, ostracized, stared at or being subject to perceived stigmatization.15, 16, 18 The effects appear to be greater (lower quality of life (QoL)) in patients at the age of 20–50 years, females and individuals subject to family stressor job change.11 Conflicting data exist regarding the impact of severity of AA and the psychological effects. In one study, patients with extensive AA have been reported to experience more adverse psychological effects than those with limited AA19 though other studies have found a non-linear relationship between extent of scalp hair loss in AA and health-related quality of life.20, 21
However, quality-of-life measurement tools used in clinical trials may not adequately capture the burden of AA, the perceived stigmatization or the psychosocial impact of AA. Applying accurate patient-reported outcomes (PRO) for HRQoL in a real-world setting is paramount to understand how the disease affects the lives of the patients.22 The objective of this study was thus to investigate the potential association between either disease severity or disease duration and the degree of social isolation, perceived stigmatization, anxiety and depression, alcohol consumption, and work absenteeism using multiple PROs in patients with AA based on data from the Danish Skin Cohort.23 Further objective was to explore characteristics of patients to investigate associations with psychological and mental components of AA.
MATERIALS AND METHODS
Data sources and study population
The present study used data from the Danish Skin Cohort, which is a prospective cohort established in 2018 to study the natural history and disease course of dermatologic diseases and has expanded to include AA, psoriasis, atopic dermatitis, hidradenitis suppurativa, chronic hand eczema and rosacea. Patients with AA were initially identified using the Danish National Patient Registry, which, from 1994 onwards, has used the tenth version of the International Classification of Diseases (ICD) system to register diagnoses. The Danish National Patient Registry is described in detail elsewhere.24 Patients categorized as suffering from AA were identified and invited if an ICD-10 code for AA (L63*) was registered, if the patient was over the age of 18 years, the diagnosis had been confirmed by a dermatologist, and as long as the patient did not suffer from psoriasis (L40*), atopic dermatitis (L20*) and hand eczema (L30.8H). Details were provided by Andersen et al.23 A total of 3198 patients were invited. To reduce the risk of participation bias, participants were only informed that the questionnaire was ‘regarding people in the Danish population’ before agreeing to participate. A questionnaire included HRQoL was dispatched in January 2023.
Severity and duration
Severity was determined based on the Alopecia Areata Scale, with mild AA defined as 1%–20% of scalp hair loss, moderate AA defined as 21%–49% scalp of hair loss and severe AA defined as ≥50% extent of scalp hair loss.25 Patients with prior AA and no scalp hair loss were considered in remission. For the analysis, only patients with clearly discernible disease severity were included. Patients were asked about the duration of their disease.
Patient-reported outcomes
The study utilized multiple PRO instruments to measure the degree of social isolation, perceived stigmatization, anxiety and depression, work absenteeism and alcohol consumption.
For the perceived impact of AA on social isolation and stigmatization, the study applied the emotion scale (items 5–11) from Skindex-16 and the anxiety/depression dimension from EQ-5D-5L. Although not developed for AA, Skindex-16 is a validated dermatology-specific instrument, which previously has been used in an adapted version for AA by changing ‘your skin condition’ to ‘your alopecia’ or ‘your scalp’,26, 27 while EQ-5D-5L has been validated and used across multiple diseases.28-30 In Skindex-16, answers are provided on seven levels ranging from ‘never bothered’ to ‘always bothered’ for the past 7 days. The number is then converted to a linear score of 0–100 (The Skindex Instruments to Measure the Effects of Skin Disease on Quality of Life). For EQ-5D-5L, answers are provided on a five-level scale from 1 (‘I am not anxious or depressed’) through 5 (‘I am extremely anxious or depressed’). While 1 represents no impairment and 2–5 denote impaired health.31 Data on depression and anxiety are further supported by the Hospital Anxiety and Depression Scale (HADS). HADS is a validated screening tool that measures each question on a scale from 0 to 3, yielding a maximum score of 21 for depression and anxiety, respectively. A score between 0 and 7 is normal, 8 and 10 is borderline normal and 11 and 21 is abnormal.32, 33
Work impairment was measured using the Work Productivity and Activity Impairment – General Health (WPAI) questionnaire, which measures absenteeism (work time missed), presenteeism (impairment at work), work productivity loss (overall work impairment measure) and activity impairment. A higher score indicates greater impairment.34 Alcohol consumption was measured using the Alcohol Use Disorders Identification Test-Consumption (AUDIT-C), for which a score of ≥4 for men and ≥3 for women is indicative of misuse.35
Specific to AA, we used the Alopecia Areata Symptom Impact Scale (AASIS), a validated tool for measuring the quality of life for patients with AA.13, 36 AASIS consists of 13 items. The first 7 items assess disease symptoms, while the following 6 measure interference with daily functioning. Each item is answered on a scale from 0 through 10, and scores are provided according to question, section (symptom and interference) and as a total score.
Statistical analysis
This cross-sectional study reported continuous variables as either means and standard deviations (SD) or medians and interquartile range (IQR), depending on the distribution. Categorical variables were presented as frequencies and percentages. The analyses investigated the effect of severity as defined by the extent of scalp hair loss on the included PRO endpoints. Multiple multivariate linear regressions were conducted using Skindex-16, AASIS and WPAI as continuous variables. The HADS, AUDIT-C and EQ-5D scores can be converted to a clinically relevant binary outcome and multivariate logistic regressions were applied. All analyses were adjusted for age, sex, involvement of eyebrows, involvement of eyelashes, age of AA onset and duration of current AA episode (<8 years or ≥8 years). The adjusting variables were all chosen a priori. Socioeconomic status was calculated in five quantiles (high, above average, average, below average and low). Results from adjusted analyses were also presented using forest plots. A level of p < 0.05 was considered statistically significant. All statistical analyses were performed in R statistical software version 4.0.2.
RESULTS
We included 477 patients who responded to the questionnaire, yielding a response rate of 15% (477 out of 3198). Of the included patients, we were able to discern disease severity for 79% (376 out of 477) of patients. By decreasing severity, 177 (47%) patients had severe disease, 41 (11%) patients had moderate disease, 94 (25%) patients had mild disease and 64 (17%) patients were in remission (Table 1). The median age of patients was 55 (IQR, 47–66 years), and most were female (70%). The median age of disease onset was 38 years (IQR, 25–51 years), and for 80% of patients, the disease had lasted ≥8 years (Table 1). For mild disease, the involvement of eyelashes and eyebrows was 43% and 45%, respectively. This number increased with disease severity, and for patients with severe disease, the numbers were 89% (eyelashes) and 94% (eyebrows) (Table 1). Active smoking was higher in patients in remission (25%) or with mild disease (22%) compared with patients with severe disease (7%) (Table 1).
| Severity | Total | Remission | Mild AA | Moderate AA | Severe AA |
|---|---|---|---|---|---|
| n | 376 | 64 | 94 | 41 | 177 |
| Age, median (IQR) [year] | 55 (47, 66) | 54 (47, 63) | 58 (48, 65) | 62 (53, 69) | 52 (46, 64) |
| Age at disease onset, median (IQR) [year] | 38 (25, 51) | 38 (29, 50) | 45 (32, 54) | 41 (22, 58) | 35 (20, 47) |
| AA for more than 8 years | 121 (80%) | 5 (83%) | 25 (61%) | 11 (92%) | 80 (86%) |
| Female sex, (n, (%)) | 264 (70%) | 46 (72%) | 70 (74%) | 26 (63%) | 122 (69%) |
| Involvement of eyelashes, n (%) | 244 (65%) | 19 (30%) | 40 (43%) | 28 (68%) | 157 (89%) |
| Involvement of eyebrows, n (%) | 258 (69%) | 24 (38%) | 42 (45%) | 26 (63%) | 166 (94%) |
| Socio-economic status, n (%) | |||||
| High | 82 (22%) | 14 (22%) | 20 (21%) | 6 (15%) | 42 (24%) |
| Above average | 85 (23%) | 13 (20%) | 22 (23%) | 11 (27%) | 39 (22%) |
| Average | 76 (20%) | 14 (22%) | 17 (18%) | 9 (22%) | 36 (20%) |
| Below average | 68 (18%) | 13 (20%) | 15 (16%) | 4 (9.8%) | 36 (20%) |
| Low | 65 (17%) | 10 (16%) | 20 (21%) | 11 (27%) | 24 (14%) |
| Smoking status, n (%) | |||||
| Current | 56 (15%) | 16 (25%) | 20 (22%) | 7 (17%) | 13 (7%) |
| Former | 149 (40%) | >25 | 32 (34%) | 19 (46%) | 73 (41%) |
| Never | >166 | 22 (35%) | >38 | 15 (37%) | 91 (51%) |
| Hair colour, n (%) | |||||
| Blonde | >97 | 14 (23%) | 15 (16%) | >13 | 55 (31%) |
| Brown | 138 (37%) | >25 | >39 | 9 (22%) | 59 (33%) |
| Dark brown or black | 62 (17%) | 11 (18%) | 19 (20%) | 9 (22%) | 23 (13%) |
| Light brown or red | 67 (18%) | 9 (15%) | 18 (19%) | 6 (15%) | 34 (19%) |
- Abbreviations: AA, alopecia areata; IQR, interquartile range.
PRO measures
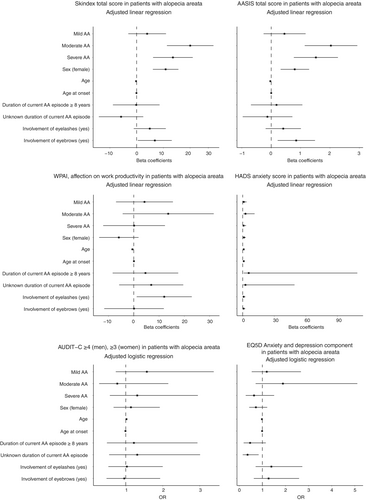
Measures of social isolation, perceived stigmatization, anxiety and depression included Skindex-16, EQ-5D-5L and HADS. The specific answers to the questionnaires are provided in Table S1. For Skindex-16, moderate AA and severe AA had largely comparable scores, while remission had the lowest scores in most cases (Table 2). For Skindex-16, the mean emotion score of moderate AA [53 (SD, 34)] and severe AA [55 (SD, 33)] was higher than the scores of mild AA [32 (SD, 26)] and remission [19 (SD, 30)] (Table 2). The Skindex-16 functioning and total score likewise reflected higher scores for moderate AA and severe AA and lower scores for mild AA and remission. In the multivariate analysis using the Skindex-16 total score, moderate AA (β-coefficient 20, 95% confidence interval (CI) 11–29), severe AA (β-coefficient 14, 95% CI 6.2–21), female sex (β-coefficient 11, 95% CI 6.1–16) and involvement of the eyebrows (β-coefficient 6.8, 95% CI 0.46–13) were associated with a higher score (Table 3A, Figure 1). When using EQ-5D-5L, a large proportion of patients, 30% to 47%, reported experiencing ‘slight to extreme anxiety or depression’ (Table 2). However, it should be noted that the high 47% is subject to uncertainty due to the small number of patients with moderate AA (Table 2). EQ-5D-5L was not able to capture any variations in the experience of anxiety and depression across disease severity (Table 3B, Figure 1). HADS neither showed any differences between severities with a median score of 5 (IQR, 2–7) for mild to severe AA and 4 (IQR, 1–6) for patients in remission (Table 3B, Figure 1).
| Questionnaires | Total | Remission | Mild AA | Moderate AA | Severe AA |
|---|---|---|---|---|---|
| n | 376 | 64 | 94 | 41 | 177 |
| Skindex-16, mean (SD) | |||||
| Skindex emotion score | 43 (34) | 19 (30) | 32 (26) | 53 (34) | 55 (33) |
| Skindex symptom score | 15 (20) | 9 (14) | 16 (19) | 20 (22) | 16 (22) |
| Skindex functioning score | 21 (27) | 10 (22) | 9 (17) | 27 (30) | 29 (29) |
| Skindex total score | 29 (24) | 14 (20) | 21 (17) | 36 (26) | 37 (25) |
| EQ-5D-5L (mental component), n (%) | |||||
| No anxiety or depression | 209 (64) | 35 (70) | 51 (61) | 17 (53) | 106 (67) |
| Slightly to extremely anxious or depressed | 116 (36) | 15 (30) | 33 (39) | 15 (47) | 53 (33) |
| AASIS, mean (SD) | |||||
| AASIS symptoms subscale score | 2.84 (2.35) | 1.27 (1.61) | 2.13 (2.01) | 3.46 (2.48) | 3.61 (2.33) |
| AASIS interference subscale score | 2.28 (2.70) | 0.81 (1.61) | 1.19 (1.78) | 2.95 (2.85) | 3.21 (2.94) |
| AASIS total score | 2.58 (2.37) | 1.06 (1.52) | 1.70 (1.78) | 3.23 (2.52) | 3.41 (2.45) |
| WPAI | |||||
| Currently employed (working for pay), n (%) | 220 (69%) | 36 (72%) | 55 (67%) | 17 (59%) | 112 (70%) |
| Hours missed from work due to AA, median (IQR) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) |
| Hours missed from work due to other reasons, median (IQR) | 0 (0, 7) | 0 (0, 0) | 0 (0, 0) | 0 (0, 14) | 0 (0, 8) |
| AA affection on productivity while working, median (IQR) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) |
| AA affection on activities other than work, median (IQR) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 1.0) |
| AA affection on productivity while working, n (%) | |||||
| Skin had no influence on work | 185 (84) | 33 (92) | 47 (85) | 14 (82) | 91 (81) |
| Skin influenced work | 35 (16) | 3 (8.3) | 8 (15) | 3 (18) | 21 (19) |
| AA affection on activities other than work, n (%) | |||||
| Skin had no influence on daily activities | 248 (77) | 42 (84) | 68 (82) | 24 (77) | 114 (72) |
| Skin influenced daily activities | 75 (23) | 8 (16) | 15 (18) | 7 (23) | 45 (28) |
| HADS, median (IQR) | |||||
| HADS anxiety total score | 5.0 (2.0, 7.0) | 3.5 (1.3, 6.0) | 5.0 (2.0, 7.0) | 5.0 (2.0, 7.2) | 5.0 (2.0, 7.0) |
| HADS depression total score | 2 (1, 5) | 2 (1, 4.75) | 2 (1, 6.00) | 2.50 (1, 5) | 2 (1, 5) |
| AUDIT-C | |||||
| AUDIT-C score, median (IQR) | 4 (2, 5) | 3 (2, 5) | 4 (3, 5) | 3 (2, 4) | 3 (2, 5) |
| Abnormal alcohol consumption, n (%) | 218 (67) | 35 (62) | 63 (72) | 16 (59) | 104 (68) |
| Normal alcohol consumption, n (%) | 105 (33) | 21 (38) | 24 (28) | 11 (41) | 49 (32) |
- Abbreviations: AA, alopecia areata; AUDIT-C, Alcohol Use Disorders Identification Test-Concise; AASIS, Alopecia Areata Symptom Impact Scale; EQ-5D-5L; HADS, Hospital Anxiety and Depression Scale; IQR, interquartile range; SD, standard deviation; WPAI, work productivity and activity impairment.
| Unadjusted | Adjusteda | |||||
|---|---|---|---|---|---|---|
| β-Coefficient | 95% CI | p-Value | β-Coefficient | 95% CI | p-Value | |
| Total Skindex-16 score | ||||||
| Remission (reference) | ||||||
| Mild AA | 6.8 | −0.43, 14 | 0.065 | 3.9 | −3.1, 14 | 0.3 |
| Moderate AA | 23 | 14, 31 | <0.001 | 20 | 11, 29 | <0.001 |
| Severe AA | 23 | 17, 30 | <0.001 | 14 | 6.2, 21 | <0.001 |
| Skindex emotion score | ||||||
| Remission (reference) | ||||||
| Mild AA | 12 | 2.2, 22 | 0.017 | 7.2 | −2.5, 17 | 0.14 |
| Moderate AA | 34 | 21, 46 | <0.001 | 30 | 18, 42 | <0.001 |
| Severe AA | 35 | 26, 44 | <0.001 | 21 | 11, 31 | <0.001 |
| AASIS total score | ||||||
| Remission (reference) | ||||||
| Mild AA | 0.64 | −0.07, 1.4 | 0.079 | 0.45 | −0.26, 1.2 | 0.2 |
| Moderate AA | 2.2 | 1.3, 3.1 | <0.001 | 2.0 | 1.1, 2.9 | <0.001 |
| Severe AA | 2.3 | 1.7, 3.0 | <0.001 | 1.5 | 0.77, 2.3 | <0.001 |
| WPAI, affection on work productivity | ||||||
| Remission (reference) | ||||||
| Mild AA | 2.7 | −8.4, 14 | 0.6 | 4.2 | −7.0, 16 | 0.5 |
| Moderate AA | 9.5 | −8.2, 27 | 0.3 | 14 | −4.4, 32 | 0.14 |
| Severe AA | 4.8 | −5.3, 15 | 0.3 | 0.13 | −12, 12 | >0.9 |
| WPAI, affection on non-work activities | ||||||
| Remission (reference) | ||||||
| Mild AA | −1.3 | −5.5, 2.9 | 0.6 | −0.78 | −5.2, 3.6 | 0.7 |
| Moderate AA | −1.2 | −6.5, 4.2 | 0.7 | −0.94 | −6.6, 4.7 | 0.7 |
| Severe AA | 2.1 | −1.7, 5.9 | 0.3 | 1.6 | −3.0, 6.2 | 0.5 |
- Abbreviations: AA, alopecia areata; AASIS, Alopecia Areata Symptom Impact Scale; CI, confidence interval; WPAI, work productivity and activity impairment.
- a Adjusted for age, sex, involvement (yes/no) of eyebrows, involvement (yes/no) of eyelashes, age of AA onset and duration of current AA episode. Severity is based on degree of scalp hair loss.
| Unadjusted | Adjusteda | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| EQ-5D-5L | ||||||
| Remission (reference) | ||||||
| Mild AA | 1.51 | 0.72, 3.24 | 0.3 | 1.19 | 0.54, 2.67 | 0.7 |
| Moderate AA | 2.06 | 0.82, 5.24 | 0.12 | 1.89 | 0.71, 5.11 | 0.2 |
| Severe AA | 1.17 | 0.59, 2.37 | 0.7 | 0.64 | 0.28, 1.51 | 0.3 |
| HADS anxiety score | ||||||
| Remission (reference) | ||||||
| Mild AA | 1.08 | 0.35, 3.70 | 0.9 | 1.02 | 0.31, 3.67 | >0.9 |
| Moderate AA | 2.08 | 0.57, 7.86 | 0.3 | 2.65 | 0.65, 11.3 | 0.2 |
| Severe AA | 0.87 | 0.31, 2.81 | 0.8 | 0.78 | 0.22, 3.17 | 0.7 |
| AUDIT-C score | ||||||
| Remission (reference) | ||||||
| Mild AA | 1.57 | 0.77, 3.23 | 0.2 | 1.57 | 0.73, 3.38 | 0.2 |
| Moderate AA | 0.87 | 0.34, 2.27 | 0.8 | 0.77 | 0.28, 2.15 | 0.6 |
| Severe AA | 1.27 | 0.67, 2.40 | 0.5 | 1.31 | 0.57, 2.95 | 0.5 |
- Abbreviations: AA, alopecia areata; AUDIT-C, Alcohol Use Disorders Identification Test; CI, confidence interval; EQ-5D-5L; HADS, Hospital Anxiety and Depression Scale;
- a Adjusted for age, sex, involvement (yes/no) of eyebrows, involvement (yes/no) of eyelashes, age of AA onset and duration of current AA episode. Severity is based on degree of scalp hair loss.
The study investigated WPAI and AUDIT-C separately. Neither PRO measures appeared to be influenced by disease severity (Table 2, Figure 1). For WPAI, most patients were employed, and few missed any workdays due to their disease. AUDIT-C showed that the majority of patients had positive screening for abnormal alcohol consumption (Table 2). Of the included patients, 15% opted not to provide an answer to the questions regarding alcohol consumption.
AASIS was the only score employed that was specific to AA. The score captured the differences between the severity of the disease, with the lowest total score in remission [mean, 1.06 (SD, 1.52)] and mild AA [mean, 1.70 (SD, 1.78)] and the highest score for moderate [mean, 3.23 (SD, 2.52)] and severe AA [mean, 3.41 (SD, 2.45)] (Table 2). Comparable to Skindex-16, the multivariate analysis indicated that moderate AA (β-coefficient 2.0, 95% CI 1.1–2.9), severe AA (β-coefficient 1.5, 95% CI 0.77–2.3), involvement of the eyebrows (β-coefficient 0.85, 95% CI 0.22–1.5) and female sex (β-coefficient 0.8, 95% CI 0.32–1.3), were associated with a higher AASIS score (Table 3A, Figure 1).
DISCUSSION
The following cross-sectional study reaching out to all Danish patients with dermatologist verified AA diagnosis included data from 376 patients from the Danish Skin Cohort. Multiple PRO measurements were utilized, including Skindex-16, AASIS, HADS scores, EQ-5D-5L, AUDIT-C and WPAI, though only Skindex-16- and AASIS scores increased with disease severity, female sex and involvement of the eyebrows, thus indicating a lower quality of life. HADS scores, EQ-5D-5L, AUDIT-C and WPAI, did not differ with disease severity. However, for many patients, EQ-5D-5L and AUDIT-C were elevated.
A study investigating the correlation between the severity of AA and PRO scores including Skindex-16 AA (AA specific version), EQ-5D-5L (EQ-VAS), HADS and WPAI also found a correlation between the severity as assessed by the physician and the PRO scores; higher severity yielded a greater negative impact on QoL.37 This was only the case for Skindex-16- and AASIS in this study. However, the criteria for assessing the severity of AA in the publication by Vañó-Galván et al. was not clearly defined, as more than 10% of patients with severe disease had mild or no scalp hair loss. Nevertheless, patients with AA demonstrate impairment in QoL comparable to other chronic dermatologic conditions such as psoriasis and atopic dermatitis.13, 15
DLQI is a commonly applied PRO measure across many dermatological diseases, but the PRO measure has not been designed to capture information on any specific disease and may not apply equally well in all clinical evaluations. DLQI has previously been investigated in the Danish Skin Cohort. A remarkably low score was found, and the authors concluded that DLQI is an inappropriate measure to thoroughly assess the quality of life related to AA, as it predominantly refers to cutaneous symptoms rather than symptoms associated with hair loss.23 DLQI was hence omitted in this manuscript.
Our data suggest a correlation between disease severity and impact in QoL using Skindex-16 and AASIS, while the other questionnaires did not. Intervals for QoL severity has not been established for Skindex-16. Applying intervals for interpretation of the Skindex-1638 using norms defined by Nijsten et al.39 (very little: 0–5.9, mild: 6–24.9, moderate: 5–49.9 and severe impairment:50+) and using mean values of the emotion score, patients in remission had mildly impaired QoL, mild AA had Skindex scores consistent with moderately impaired QoL and patients with moderate or severe AA had Skindex scores corresponding to severe impairments. This was true for scores related to social isolation and perceived stigmatization, while depression scores showed moderate impairment. These results align with a similar cross-sectional study in which patients with moderate or severe AA had Skindex-total scores in the moderate to severe range.21 AASIS also appeared to correlate with severity, but was the only score specifically developed to evaluate the QoL of patients with AA, with evidence supporting internal consistency and validity.36 In previous studies, AASIS has likewise been found to correlate with AA severity and clinical response to treatment, furthering the argument for the association presented on the impairment of QoL and disease severity.40-42 On the other hand, HADS scores, EQ-5D-5L, AUDIT-C and WPAI did not indicate an association with disease severity.
For AUDIT-C, a recent case–control analysis found AA to be significantly associated with alcohol-use disorder.43 Although, it may have been assumed that more severe disease would have a higher susceptibility for abnormal alcohol consumption, this association was not found in the present study. However, regardless of severity, there was a large proportion of individuals with a positive screening for abnormal alcohol consumption.
Interestingly, the two questionnaires suggesting a correlation with disease severity consistently found that female sex and involvement of the eyebrows negatively influenced QoL. Multiple studies have already reported the effect of age and sex on QoL impairment among patients with AA, showing, among others, that age < 50 years, female sex, amount of hair loss, family stress and job changes were each associated with diminished QoL.12 A recent systematic review reported that girls experience a greater psychological effect and more difficulty with social interactions caused by their AA than boys.44, 45 Eyebrow and eyelash involvement have been shown to potentially impact the QoL of patients, although the results were none-significant.21 On the contrary, in this study, eyelashes did not appear to influence any of the PRO scores, while eyebrows did. As eyebrow hair loss not only affects the patient's appearance, but may also affect how others perceive them and how they convey emotions, it may be an important aspect to consider.21 Clinician- and patient-rated eyelash and eyebrow hair assessment tools have been published and may be useful in a clinical setting.46
There are multiple limitations to the study that warrants mentioning. This is a descriptive study of self-reported data. As such, limitations include multiple types of bias, including recall, volunteer and non-response, for example, patients with clinical depression may not respond to the questionnaires. This include the potential of unmeasured confounding, for example, AA universalis was not adjusted for. Furthermore, none of the instruments discussed in this paper except AASIS were validated in AA, and although severity, as determined by scalp hair loss, was used to distinguish between patient groups, the instruments by yet be limited in capturing discrepancies in impact on QoL between these groups, for example, Skindex-16 does not include questions on hair. Hence, although severity may correlate with an instrument that instrument may not truly capture the impact on variables measured. Additionally, the generalizability of findings from this Danish adult AA population may differ from that of other countries due to the homogenous nature of the study population and could potentially be limited by the response rate. Lastly, as the cohort includes patients with a dermatologist-verified diagnosis, the result may reflect a population who, at least at some point during the cause of the disease, had a severity that required dermatological assessment and may not apply to all patients with AA.
In conclusion, the results highlight the importance of implied relevant questionnaires when measuring specific aspects of QoL, as all questionnaires may not fully capture the effects of disease severity. The study indicated that higher severity was associated with a higher impact on social isolation and perceived stigmatization and somewhat on feelings of depression when using Skindex-16 and AASIS. The population did not appear to show signs of clinical depression or anxiety based on the HADS screening tool, but approximately a third to half of patients did report at least some impairment based on the EQ-5D-5L. Furthermore, the result indicated that female sex and involvement of the eyebrows increased the impact on QoL as measured by PROs.
AUTHOR CONTRIBUTIONS
Conceptualization: All authors. Data curation: MC, AE and DTH. Formal analysis: MC, AE and DTH. Funding acquisition: AE and DTH. Investigation: All authors. Methodology: All authors. Project administration: AE and DTH. Resources: AE and DTH. Software: MC and DTH. Supervision: AE and DTH. Validation: All authors. Visualization: MC. Writing—original draft: MC and DTH. Writing—review and editing: All authors.
ACKNOWLEDGEMENTS
Not Applicable.
FUNDING INFORMATION
Pfizer provided financial support for the study.
CONFLICT OF INTEREST STATEMENT
Dr. Clemmesen has no conflicts of interest to declare. Dr. Thein has unrelated to this research received funding from Ebba Celinders Legat and Else og Mogens Wedell-Wedellsborgs Fond and holds stocks in the SP500 and Novo Nordisk. Dr. Egeberg has received research funding from Pfizer, Eli Lilly, Novartis, Bristol-Myers Squibb, Boehringer Ingelheim, AbbVie, Janssen Pharmaceuticals, the Danish National Psoriasis Foundation, the Simon Spies Foundation and the Kgl Hofbundtmager Aage Bang Foundation, and honoraria as consultant and/or speaker from AbbVie, Almirall, Leo Pharma, Zuellig Pharma Ltd., Galápagos NV, Sun Pharmaceuticals, Samsung Bioepis Co., Ltd., Pfizer, Eli Lilly and Company, Novartis, Galderma, Dermavant, UCB, Mylan, Bristol-Myers Squibb, Boehringer Ingelheim, Union Therapeutics and Janssen Pharmaceuticals, and is currently employed by LEO Pharma. Dr. Thomsen has been a speaker or has served on advisory boards for Sanofi-Genzyme, AbbVie, LEO Pharma, Pfizer, Eli Lilly and Company, Novartis, UCB Pharma, Almirall and Janssen Pharmaceuticals; has received research support from Sanofi-Genzyme, AbbVie, LEO Pharma, Novartis, UCB Pharma and Janssen Pharmaceuticals; and has been an investigator for Sanofi-Genzyme, Regeneron, AbbVie, LEO Pharma and Pfizer. PhD Gren and MSc Frostrup are employees of Pfizer Denmark and own Pfizer Inc. stock options.
ETHICS STATEMENT
This study involved human participants but was not approved in accordance with Danish law. A review of an ethics committee is not required in Denmark for studies not involving human tissue. Participants gave informed consent to participate in the study before taking part.
Open Research
DATA AVAILABILITY STATEMENT
Data are available upon reasonable request. There are no plans on sharing the raw data; however, data from the Danish Skin Cohort will be available for research collaborations upon obtaining the necessary legal approvals.