Irbesartan Does Not Influence the Antiplatelet Effect of Aspirin in Spontaneously Hypertensive Rats
Because of the hemodynamic variation and endothelium impairment, hypertension is by far the most potent risk factor for stroke 1. Considerable trials have demonstrated that early intervention with the measures of platelet aggregation and blood pressure control can effectively decrease the incidence of stroke 2. Angiotensin receptor blockers (ARBs) and platelet aggregation inhibitor, such as aspirin, are the most commonly prescribed medications to prevent stroke in hypertensive patients. Recently, some data showed that ARBs could activate NF-κB pathway and increase proinflammatory gene expression associated with atherosclerosis and platelet aggregation through overstimulation of AT2 3. Long-term administration of ARBs also results in a several-fold increase in plasma AngIV, a N-terminal angiotensin degradation product, which could participate in thrombus formation through upregulating plasminogen activator inhibitor-1 expression 4. These findings suggest that ARBs could participate in the pathogenesis of stroke and could increase platelet aggregation. So in this study, we used irbesartan, one of the ARBs, to investigate whether ARBs affect the platelet aggregation in spontaneously hypertensive rats (SHR) administered aspirin.
Forty male SHR aged 14 weeks (250–300 g) were treated with aspirin (30 mg/kg/day), irbesartan (30 mg/kg/day), and their combination, and control animals with vehicle for 6 weeks. All animals received humane care and experimental procedures in compliance with institutional animal care guidelines. The platelet aggregation was determined by the light turbidimetric method. Blood for platelet aggregation studies was collected by abdominal aorta puncture from the SHR anesthetized with sodium pentobarbital (45 mg/kg i.p.). Whole blood was mixed with 3.8% trisodium citrate buffer (9:1 v/v) and then centrifuged at 114 g for 20 min at 4°C to obtain platelet-rich plasma (PRP). Platelet-poor plasma was prepared by centrifuging blood at 2682 g for 10 min and was used for adjusting the platelet concentration of PRP to 200,000–300,000 cells/mL and calibrating the aggregometer at maximal light transmittance. The maximum platelet aggregation of PRP was monitored at 37°C with platelet aggregation analysis system (IDXS-800i, Japan). Data were expressed as mean ± SD and analyzed using unpaired Student's t-test. Statistical significance was set at P < 0.05.
From the results (Figures 1 and 2), it can be found that the platelet aggregation induced with arachidonic acid (AA) and collagen in SHR fed with aspirin or combination of aspirin and irbesartan was significantly lower than in control group or irbesartan group (P < 0.001). There was no significant difference between aspirin group and combination of aspirin and irbesartan group. In the same way, there was also no significant difference between irbesartan group and control group.
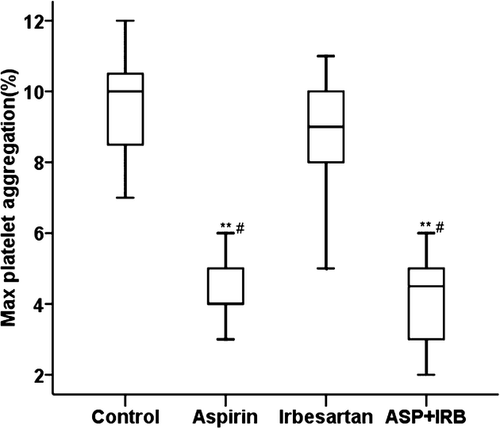
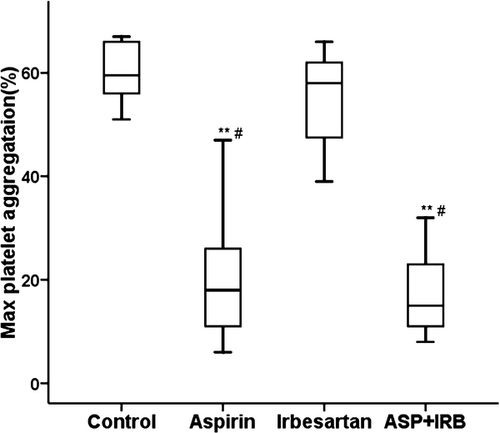
Large population studies have shown that aspirin reduces the incidence of both primary and secondary cerebrovascular disease by approximately 25% 5. However, aspirin fails to prevent stroke in a large proportion of people because of insufficiently suppressed platelet aggregation named “aspirin resistance”. Some studies suggested that the activation of COX-2 induced by inflammatory factors could attenuate the antiplatelet aggregation from aspirin and thus promote platelet aggregation. We investigated whether irbesartan could play a counter-regulatory role against aspirin in SHR. The results showed that aspirin can effectively decrease the platelet aggregation in those fed with irbesartan or not, and there was also no reverse effect on platelet aggregation from irbesartan.
Inflammatory mediator and oxidative stress are the major pathogenic molecular mechanisms underlying cerebral ischemic insults 6. Many studies have demonstrated that inflammation is one of the most important factors involved in the hypertension-induced stroke 7. In our previous study, we found that irbesartan can upregulate the inflammatory gene expression, such as MMP2, COX2, PECAM1, related to promoting platelet aggregation. In this study, we did not find the increase in platelet aggregation associated with irbesartan. Further, the results showed a downregulating trend when induced by AA or collagen.
In conclusion, our data showed that irbesartan did not affect the effects of aspirin on platelet aggregation in SHR. The concomitant use of irbesartan and aspirin might be safe for the prevention of thrombotic diseases.
Acknowledgments
This study was supported by the State Ministry of Science and Technology (2009BAI86B04).
Conflict of Interest
The authors declare no conflict of interest.




