Updates on grading mesothelioma
Abstract
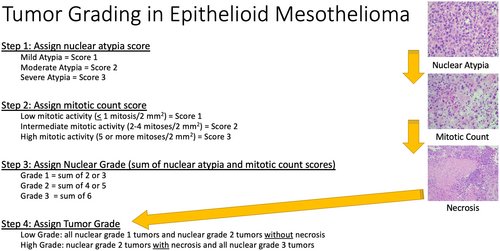
Mesothelioma is a rare disease with an historically poor prognosis. Over the past decade, a grading system has been developed that is a powerful prognostic tool in epithelioid mesothelioma. Grading of epithelioid mesothelioma is now required or strongly recommended by expert consensus, the College of American Pathologists, the World Health Organization, and the International Mesothelioma Interest Group. The original nuclear grading system for epithelioid mesothelioma, developed in the United States, split epithelioid mesotheliomas into three prognostic groups with marked differences in survival. Now, this three-tiered nuclear grading system has been combined with the presence or absence of necrosis to form the currently recommended two-tiered grading system of low- and high-grade epithelioid mesothelioma. This review will focus on the development of this grading system in mesothelioma, the grading system's shortcomings, and the application of the grading system to cytology specimens and other extra-pleural sites. Lastly, this review will briefly discuss alternative grading systems and future considerations.
Graphical Abstract
Introduction
Given that mesothelioma is a rare tumour with only approximately 3000 cases diagnosed annually in the United States,1, 2 establishing a pleural proliferation as mesothelial in lineage and then determining that it is malignant, either through direct invasion of underlying tissue or via biomarker evaluation (BAP1 and MTAP immunohistochemistry, or CDKN2A homozygous deletion by fluorescence in situ hybridization),3-8 one may find a sense of relief that the diagnosis has been rendered. After establishing the diagnosis, both expert subspecialty thoracic/pulmonary pathologists and general surgical pathologists know the importance of subtyping mesothelioma. Numerous studies, time and again, have shown the prognostic significance of classifying mesothelioma as either epithelioid, biphasic, or sarcomatoid.9, 10 While a Tumour, Node, Metastasis (TNM) staging system has been in use for some time,11 many pathologists end their report after stating the mesothelioma subtype. We have also observed in our own practice that this is especially true of small biopsy specimens. Even though not yet in widespread use, it is important to note that other significant and powerful prognostic features can be reported for both biopsy and resection specimens. Over the past decade, grading of epithelioid mesothelioma has emerged as a very robust prognostic tool. This review will cover the current literature and recommendations on grading mesothelioma. No original data are presented in this review. All data presented in this article were identified via searches of Pubmed.gov database.
Development of a nuclear grading system in epithelioid mesothelioma
In 2012, Kadota et al.,12 based at Memorial Sloan Kettering in New York, published their work highlighting their development of a grading system to be used in epithelioid mesothelioma. They studied a series of over 200 epithelioid mesotheliomas, looking at a number of potential prognostic features including nuclear atypia, nuclear-to-cytoplasmic ratio, chromatin pattern, intranuclear inclusions, prominent nucleoli, mitotic count, and atypical mitoses. They found through multivariate analysis that nuclear atypia and mitotic count were independent prognostic factors. From these two parameters they devised a three-tiered nuclear grade. This three-tiered grading system resulted from the sum of a nuclear atypia score and a mitotic count score. The three nuclear grades (1–3) were shown to stratify this cohort of patients into specific prognostic groupings. These prognostic groupings were quite striking in overall survival. This study showed the lowest nuclear grade, nuclear grade 1, had a survival of just over 2 years. While the highest grade, nuclear grade 3, showed a survival nearly identical to that of sarcomatoid mesothelioma (~5 months).
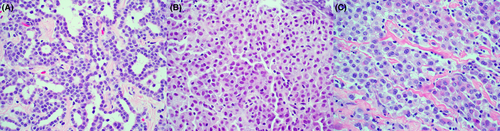
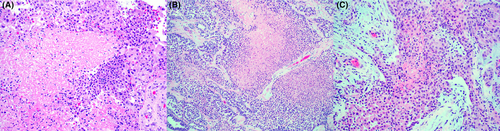
According to Kadota et al., the nuclear atypia is scored based on nuclear size and irregularity. Nuclear atypia score 1 (Figure 1) is only mild nuclear atypia characterized by uniform nuclei with similar size and shape. Nuclear atypia score 2 (Figure 2) is moderate atypia characterized by intermediate-sized nuclei with some irregularity in size and shape. Nuclear atypia score 3 (Figure 3) is severe atypia characterized by bizarre nuclear pleomorphism and marked variation in size and shape, often accompanied by prominent nucleoli. Nuclear atypia is considered significant if it consists of more than 5% of the entire tumour area.

Mitotic count scoring was originally performed in the Kadota study based on a count of 10 high-power fields (HPF). The original scoring system allowed for up to 1 mitotic figure per 10 HPF, scored as 1, for low mitotic activity; two to four mitotic figures per 10 HPF, scored as 2, for intermediate mitotic activity; and greater than or equal to five mitotic figures per 10 HPF, scored as 3, for high mitotic activity. Mitotic activity should be determined in areas devoid of, or with little necrosis, stromal fibrosis, or inflammation.
After atypia and mitotic count scores are assigned, the sum of these scores equates to the nuclear grade (Table 1). A sum of 2 or 3 is nuclear grade 1, a sum of 4 or 5 is nuclear grade 2, and a sum of 6 is nuclear grade 3. The differences in survival between the various nuclear grades were found to be statistically significant. Even though the original Kadota et al. article showed a disproportionate number of cases with low or intermediate nuclear grade (grade 1 n = 107, and grade 2 n = 91) compared to those with high nuclear grade (grade 3 n = 34), the study was adequately powered to show statistical significance amongst these groups. Lastly, Kadota et al.12 showed that the observations on nuclear grading held true regardless of the TNM stage of the tumour.
| Nuclear grading in epithelioid mesothelioma |
|---|
| Step 1: assign nuclear atypia score |
| Mild atypia = Score 1 |
| Moderate atypia = Score 2 |
| Severe atypia = Score 3 |
| Step 2: assign mitotic count score |
| Low mitotic activity (≤1 mitosis/2 mm2) = Score 1 |
| Intermediate mitotic activity (2–4 mitoses/2 mm2) = Score 2 |
| High mitotic activity (5 or more mitoses/2 mm2) = Score 3 |
| Step 3: assign nuclear grade (sum of nuclear atypia and mitotic count scores) |
| Grade 1 = sum of 2 or 3 |
| Grade 2 = sum of 4 or 5 |
| Grade 3 = sum of 6 |
The authors of the Kadota study advocated for the adoption of this three-tiered system for epithelioid mesothelioma, and noted that it appeared especially applicable to clinical diagnosis and research settings. They admitted that interobserver variability may be an issue, but felt that they controlled for this as best as possible by using criteria previously found to be easily recognizable and reproducible by pathologists.12-14 Nonetheless, the reproducibility of this nuclear grading system has yet to be tested.
Further validation of the three-tiered grading system and importance of necrosis
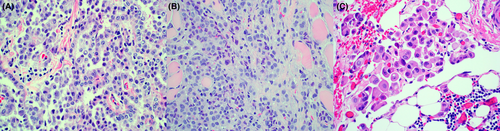
Following the Kadota et al. study, a study from France replicated the prognostic impact of the three-tiered nuclear grading system.15 Also, a multi-institutional effort was put forth to build on this previous work. Adding to the original cases from the Memorial Sloan Kettering Cohort, 17 different institutions contributed cases in an international effort lead by the University of Chicago. This study published by Rosen et al.,16 in 2018, further validated the three-tiered nuclear grading concept in epithelioid mesothelioma. Rosen et al. collected over 750 cases of epithelioid mesothelioma. They again replicated the findings of Kadota et al., showing a median survival of 27, 14, and 8 months in nuclear grades 1, 2, and 3, respectively. This study also established that tumours harbouring necrosis (Figure 4) showed differences in overall survival; 10 months for those tumours with necrosis, and 19 months for those tumours without necrosis. When examining individual nuclear grade categories (1–3), the addition of necrosis appeared to also predict survival, with the best overall survival seen in nuclear grade 1 tumours without necrosis. The median survival in nuclear grade 1 tumours with necrosis was similar to nuclear grade 2 tumours without necrosis. Nuclear grade 3 tumours fared slightly worse than nuclear grade 2 tumours with necrosis. The difference between nuclear grade 3 with and without necrosis did not reach statistical significance. This study was also the first to associate a morphologic pattern with prognostic significance, suggesting that tumours with a predominantly solid growth pattern are associated with worse overall survival, although this finding did not hold true as an independent prognostic factor in multivariate analysis. Additional discussion of morphology and nuclear grade will be presented later in the article.
Adoption of nuclear grading as standard practice in epithelioid mesothelioma
The 2017 update of the consensus statement on mesothelioma diagnosis from the International Mesothelioma Interest Group did not officially endorse the three-tiered nuclear grading system.3 In 2018, a multidisciplinary group of mesothelioma experts, including pathologists, surgeons, radiologists, oncologists, and others, met to discuss the histologic classification of mesothelioma. The findings from this meeting were subsequently published in the Journal of Thoracic Oncology.17 Reporting of nuclear grade was officially endorsed, albeit with a slight modification by expert consensus, as a result of this meeting and publication. The grading system was based on the work previously completed by Kadota et al.,12 but instead of reporting a three-tiered grading system, the experts concluded that a two-tiered system would be most appropriate.17 The decision to utilize a two-tiered system was based on the work by Rosen et al. incorporating the presence or absence of necrosis into the three-tiered nuclear grading system.16 The new two-tiered system splits epithelioid mesotheliomas into two categories, low and high grade (Table 2). Low-grade epithelioid mesothelioma consists of all nuclear grade 1 cases and nuclear grade 2 cases without necrosis. High-grade epithelioid mesothelioma consists of nuclear grade 2 cases with necrosis and all nuclear grade 3 cases. It should be noted that in an attempt to standardize reporting across institutions, counting mitoses in a 2 mm2 area is strongly encouraged; this is in contrast to counting 10 HPF, which was used in both the Kadota and Rosen articles. Grading was recommended on all specimens, including biopsies. Subsequent work has shown that grading can be applied to biopsy specimens.18, 19 This two-tiered grading system is now also recommended by the most recent WHO Classification of Thoracic Tumours book, and is a required element in the College of American Pathologists synoptic report.20-22 Grading of epithelioid mesothelioma is also recommended by the updated consensus diagnosis guidelines sponsored by the International Mesothelioma Interest Group (article under review).
| Tumour grading in epithelioid mesothelioma |
|---|
| Step 1: assign nuclear atypia score (1, 2, or 3) and mitotic count score (1, 2, or 3) |
| Step 2: assign three tier nuclear grade (1, 2, or 3) |
| Step 3: assign tumour grade |
| Low grade: all nuclear grade 1 tumours and nuclear grade 2 tumours without necrosis |
| High grade: nuclear grade 2 tumours with necrosis and all nuclear grade 3 tumours |
Nuclear grade in relation to morphologic features and molecular findings
It is now understood that certain morphologic features are associated with prognosis across all subtypes of mesothelioma. These features include morphologic patterns, stromal features, and cytologic features.17, 22 Consider some of the following as examples: (1) epithelioid mesothelioma with >50% solid architecture is associated with poor prognosis, (2) mesotheliomas with stroma composed of at least 50% myxoid features are associated with good prognosis, and (3) pleomorphic cytologic features are associated with worse prognosis.3, 16, 23-26 In epithelioid mesothelioma, the connection between most of these morphologic features and tumour grade is not well studied, except for pleomorphic epithelioid mesothelioma. Zhang et al.18 studied patterns of growth and pleomorphic features in epithelioid mesothelioma in the setting of application of the new two-tier grading system. This study showed that a composite score of growth pattern combined with a two-tier grade did not result in improved prognostication. Most importantly, the study did show that pleomorphic epithelioid mesothelioma had worse overall survival compared to nonpleomorphic mesotheliomas, and that pleomorphic epithelioid mesothelioma should be considered as a stand-alone prognostic group. The median overall survival for pleomorphic mesotheliomas was 5.4 months, compared to 19.3 months for low-grade and 8.9 months for high-grade epithelioid mesotheliomas.
It is well documented in the literature that specific genetic alterations appear to impact prognosis. There is a trend reported in most, but not all, articles showing improved survival in mesotheliomas that harbour a BAP1 mutation, as evidenced by loss of BAP1 expression by immunohistochemistry.6, 27-31 Unlike BAP1 mutation, CDKN2A homozygous deletion and/or MTAP immunohistochemical loss of expression have been associated with a worse overall survival.30, 32-34 We previously attempted to determine if an underlying genetic link exists between some of these morphologic prognostic features and tumour grade.35 We did find an association between BAP1 mutation and lower nuclear grade in pleural, but not peritoneal mesothelioma. We did not find any conclusive evidence in this somewhat limited dataset of an association between other morphologic features, nuclear grade, and underlying genetic mutation. This is an area of active and ongoing research.
Shortcomings of the epithelioid grading system
While grading of epithelioid mesothelioma is now widely recommended by expert consensus and the WHO,17, 20-22 there are some shortcomings with this grading system. First, the three-tiered grading system was robustly studied and validated for use, but the two-tiered grading system largely arose from expert consensus without robust testing prior to recommending its use in the clinical setting. While there was some support for the two-tiered grading system based on the study by Rosen et al.,16 the aim of the Rosen study was not to create a two-tiered grading system. We subsequently re-reviewed the original data from the Rosen study and did find a statistically significant difference when applying the two-tiered system to the original data set (unpublished data). Some subsequent studies have been published using the two-tiered grading system and continue to show that there is a prognostic value in this system and that the two-tiered grading system can be used in both biopsy and resection specimens.18, 19 Second, the grading system was developed and endorsed by experts in pulmonary and thoracic pathology with significant experience in the diagnosis and classification of mesothelioma. Now, these same experts state that all cases of epithelioid mesothelioma should be graded. Unfortunately, the reproducibility of these grading systems amongst general pathologists and amongst pathologists with expertise in other fields of surgical pathology has not been rigorously tested. We have studied and found that the reproducibility of this grading system amongst nonexpert pulmonary/thoracic/mesothelioma pathologists yields only moderate agreement and reproducibility.36 This would suggest additional training may be necessary in order to generate better agreement amongst all pathologists, both expert and nonexpert, who grade mesothelioma. Third, there are very little data in the published literature to inform the pathologist as to the value of applying this grading system at metastatic sites, but in one small study we found only moderate agreement comparing histopathologic parameters at metastatic sites compared to primary sites.37 We previously published differences between grade and other histopathologic parameters in biopsy and resection specimens in epithelioid mesothelioma.38 The data from this study was nearly identical to others that looked at histopathologic parameters between biopsy and resections,39-41 but these other studies did not specifically look at nuclear grade. We found that the three-tiered grading system and necrosis showed only moderate agreement (75% concordance [K = 0.59] and 81% concordance [K = 0.53], respectively) between biopsy and resection specimens. A possible driver of this moderate agreement was the fact that it was not uncommon for nuclear grade to be upgraded in the resection specimen by one grade (usually nuclear grade 1 to nuclear grade 2); it was quite rare that a resection specimen would show a lower nuclear grade than the biopsy specimen. Nuclear grade 3 in a biopsy was highly predictive of the same nuclear grade in the resection specimen (specificity of 98.9%). This study did not assess the two-tiered grading system between biopsy and resection, as it was initiated prior to that system being recommended for use in the clinical setting. With the reduction of categories from three to two, one may postulate that agreement may be slightly better between biopsy and resection specimens using the two-tiered system. The last major shortcoming of the currently used nuclear grading system is that, outside of the original work done by Kadota et al.,12 the nuclear grading system has not been scrutinized under multivariate analysis taking into consideration significant clinical features, most notably, the clinical stage. While the Rosen et al.16 study was larger than Kadota et al., Rosen did not incorporate TNM staging as part of the statistical analysis due to incomplete data.
Grading of cytology specimens
The diagnosis of mesothelioma in cytology specimens has long been a source of controversy in the field and a detailed discussion of this topic is beyond the scope of this review. The advent of the use of specific immunohistochemical markers allows for the determination of mesothelial lineage in effusion cytology specimens and also allows for characterization of these effusions as malignant if loss of expression of BAP1 and/or MTAP are observed.42-45 Aided by immunohistochemistry, cytologists now enter a new era of diagnosis of mesothelioma. While much attention has been paid to the use of ancillary studies in the diagnosis of mesothelioma in effusion specimens, the question arises as to how reliable nuclear grading and histological classification is in these specimens. A recent study concluded that assessment of certain morphologic features is possible in pleural effusion cytology specimens.46 Most notably, there was 100% concordance between cytology and surgical specimen nuclear atypia. There is also a high agreement in the detection of necrosis between the two specimen types. Regardless of the agreement observed in nuclear atypia and necrosis, the authors of this study rightfully state that nuclear grading in its current form cannot be performed on cytology specimens, as the current grading system requires a mitotic count in a 2 mm2 area. While one could theoretically count a 2 mm2 area in a cytology specimen, counting mitotic figures in this manner has never been studied, nor has it been validated for use.
Peritoneal mesothelioma
The vast majority of work on grading mesotheliomas has been performed in the setting of diffuse pleural mesothelioma. It should be noted that 10–20% of mesotheliomas arise from the peritoneum. The application of this grading system to peritoneal mesothelioma is currently not a part of any expert consensus or professional society guideline recommendation. Nevertheless, it is our personal practice to grade epithelioid mesothelioma arising from the peritoneum just as it is done in the thoracic cavity. There is some evidence in the literature that was previously published that supports this practice. In work by Chapel et al., the three-tiered nuclear grading system showed an ability to prognosticate between groups of epithelioid peritoneal mesothelioma patients, just as can be done with pleural mesothelioma.38 Interestingly, there was an absence of statistical significance when assessing necrosis as an independent prognostic factor in this peritoneal cohort. Some additional work prior to the Chapel study also showed that one could apply the original three-tiered grading system to peritoneal mesothelioma, but multivariate analysis was not performed in that study.47 While it is promising to see that grading of epithelioid mesothelioma performs similarly to what has been observed in the pleura, it should be noted that many pathologists feel that there are significant differences between pleural and peritoneal mesothelioma. These differences are most striking when examining the epidemiology and biology of peritoneal mesothelioma.48-50 Treatment also greatly varies between pleural and peritoneal mesothelioma, with the use of cytoreductive surgeries and intraperitoneal chemotherapy.51-53 Thus, it is unclear how closely one can compare these two disease processes at present. Others have looked at different grading systems in peritoneal mesotheliomas, but there is yet to be a formed consensus as to how and if peritoneal mesotheliomas should be graded.
Other proposed grading systems
Over the years, some authors have proposed alternative grading systems for mesothelioma. In contrast to the recommended grading system, which only applies to epithelioid morphology, these alternative grading systems have been applied to both epithelioid and nonepithelioid morphologies. These grading systems have yet to be widely studied or adopted outside of single institutions, nor have they been recommended by any consensus or guideline statements. These grading systems will be briefly discussed here as they are in the literature, and they do raise questions as to if pathologists can extend grading to nonepithelioid mesotheliomas. Pelosi et al.54 developed a grading system based on histologic subtype, necrosis, mitotic count, and Ki-67 index by immunohistochemistry. This study assigned points to each of these parameters and summed these points together. With an increase in points, there was an associated decrease in survival. More recently, work out of Australia has proposed a grading system to be used across all histologic subtypes of mesothelioma.55 This proposed Mesothelioma Weighted Grading Scheme (MWGS) was based upon point assignments in numerous categories including age, histologic subtype, necrosis, mitotic count, nuclear atypia, and BAP1 expression. The authors of this study did compare the MWGS with the WHO two-tiered system, but it is unclear how this comparison was completed, as the WHO two-tier system, by definition, cannot be applied to nonepithelioid morphologies. It is also interesting that the MWGS article found that the WHO two-tiered system was only predictive of median survival in mesotheliomas with BAP1 loss, a novel finding that is yet to be replicated. The Australian group subsequently developed and published a prognostic nomogram to be used across all subtypes of mesothelioma.56
It is our opinion, and the opinion of others active in the field, that there currently does not exist enough data to support grading of nonepithelioid mesothelioma, especially given the historically poor prognosis associated with nonepithelioid morphology. Historical median survival reported for sarcomatoid morphology ranges anywhere from 5 to 8 months. The studies looking at prognosis in nonepithelioid morphology by their respective proposed grading systems do not present clear-cut evidence that the reported grades outweigh the poor prognosis that accompanies nonepithelioid morphology.
Use of mesothelioma grade in the clinical setting
Given that epithelioid mesothelioma is the most prevalent subtype, it could be postulated that the striking differences in overall survival observed following grading may be quite useful to the treating oncologist and surgeon. Since the survival of nuclear grade 3 epithelioid mesothelioma mirrors that of sarcomatoid mesothelioma, one may wonder if treatment decisions should be made based on these findings. Considering the treatment differences between epithelioid and sarcomatoid mesothelioma, in which sarcomatoid morphology does not yield a survival benefit with surgery,57, 58 one can question if there is a survival benefit if surgery is offered to a grade 3 epithelioid mesothelioma. Over the last decade, there has been a lack of significant effort to incorporate grading into treatment decision-making, and it has remained mostly a prognostic tool. Nonetheless, given its strong overall performance as a prognostic indicator, for those patients who wish to know and understand the prognosis of their disease, this may be very useful information.
Conclusion
In recent years, the development of a grading system for epithelioid mesothelioma has emerged. Some key advantages of the current two-tier grading system include how the system was developed and its ease of use. The two-tier grading system was built from large studies employing multivariate analyses to extract from the slide, the most salient histologic features that affect prognosis. The grading system is relatively easy to deploy in the everyday practice of surgical pathology. The grading system utilizes only the pathologist's eyes and microscope. No additional special tools are required, and the pathologist is able to immediately relay important prognostic information to the clinical team. Nevertheless, some disadvantages remain. The grading system can only be applied to a subset of mesotheliomas (epithelioid cases only) and the true prognostic power of the grading system is unproven. Is the grading system more prognostic than clinical staging? Is the grading system reproducible? How the grading system can be applied by the clinical team to make treatment decisions has not been studied. All these questions should be addressed in future research.
It must be noted that the landscape of mesothelioma prognostication has changed with the advent of the use of immunotherapy in mesothelioma. According to the Checkmate 743 study, patients with nonepithelioid mesothelioma are seeing significant improvements in survival when treated with immunotherapy compared to standard chemotherapy.59, 60 How this shift in the understanding of mesothelioma behaviour in the setting of immunotherapy impacts grading of mesothelioma is currently unclear. To date, there are no studies that look at morphologic features or grading of mesotheliomas in the setting of immunotherapy treatment. Are there morphologic clues in these cases that may suggest response to treatment or nonresponse to treatment? If those studies are performed and certain morphologic features can be associated with response or nonresponse to therapy, then there may be some validity in grading and further characterizing mesotheliomas with nonepithelioid morphology. This is a fascinating and rapidly evolving area of study and there is sure to be additional data generated in the coming months and years on this topic.
In summary, at present it is recommended that all specimens that carry a diagnosis of epithelioid mesothelioma should be graded according to published guidelines using a two-tiered (low and high) grade system. There currently is no recommendation and a lack of strong evidence to perform grading in mesotheliomas with nonepithelioid morphology or in cytology specimens. While the concept of nuclear grading has been around for over a decade, its use has largely been limited to specialized mesothelioma centres and expert mesothelioma pathologists; only recently was grading simplified and recommended for widespread use. The coming years will show how widely accepted grading becomes and how grading may be incorporated into clinical practice.
Author contributions
Conception and design: All authors. Administrative support: None. Provision of study materials or patients: None. Collection and assembly of data: JJS. Data analysis and interpretation: All authors. Article writing: All authors. Final approval of article: All authors.
Open Research
Data availability statement
No original peer-reviewed data is presented in this review. All data presented in this manuscript was identified via searches of Pubmed.gov database.