Predictors of Recovering Full Consciousness: Results From a Prospective Multisite Italian Study
Funding: The study was funded by the Italian Ministry of Health under the “Ricerca Corrente” RC2020-22 programs and the “5xMille” funds AF2018: “Data Science in Rehabilitation Medicine,” AF2019: Study and development of biomedical data science and machine learning methods to support the appropriateness and the decision-making process in rehabilitation medicine. The study was also funded by Regione Toscana (Bando Ricerca Salute 2018) under the TUNE-BEAM project.
[Correction added on 22 July 2025 after first online publication: An author’s name Chiara Tramonti has been changed to Caterina Tramonti.]
ABSTRACT
Background
Improving prognostication in patients with a prolonged disorder of consciousness (pDoC) is among the most challenging issues in neurorehabilitation. The aim of this Italian multisite prospective longitudinal study was to identify valuable predictors of the complete recovery of consciousness (emergence from Minimally Conscious State, eMCS) at 3 months (T1) from the admission in intensive rehabilitation units (IRUs) in pDoC (T0).
Methods
Patients with Unresponsive Wakefulness Syndrome (UWS) or MCS admitted within 3 months of injury to 4 Italian IRUs were included. Demographic, clinical, and neurophysiological data were collected at T0, and a clinical diagnosis of consciousness (UWS, MCS−, MCS+) was established at T0 and T1 using the Coma Recovery Scale-Revised (CRS-R).
Results
One hundred forty-three patients were initially included and 131 completed follow-ups at T1: (76 males; median age: 69 years [IQR = 23]; VS/UWS: 51, MCS−: 29, MCS+: 51; etiology: 33 traumatic, 14 anoxic, 24 ischemic, 55 hemorrhagic, 5 other; median time post-injury: 40 days [IQR = 23]). At T1, 77 patients were eMCS, and 10 improved their clinical diagnosis. Among the clinical and neurophysiological independent variables, a higher CRS-R visual sub-score and the presence of EEG reactivity to eye opening at T0 were the best independent predictors of eMCS. Out of 77 eMCS, 18 reached a moderate disability (Glasgow Outcome Scale Extended-GOSE > 4), while the others persisted with a severe disability (GOS-E ≤ 4).
Conclusions
A multimodal assessment can help identify patients who achieve functionally relevant improvements and thus better support clinicians when communicating with caregivers.
Trial Registration
ClinicalTrials.gov registration number: NCT04495192
1 Introduction
Disorders of consciousness (DoC) are commonly caused by severe acquired brain injuries (sABI) and often result in permanent disability, raising substantial clinical, ethical, and economic concerns. In Italy, the incidence of DoC has been estimated to range between 1.8 and 1.9 per 100,000 individuals, and the prevalence between 2.0 and 2.1 per 100,000, including only patients with Vegetative State/Unresponsive Wakefulness Syndrome (VS/UWS) [1]. Based on the presence of behavioral responses, the current diagnostic framework for DoC includes VS/UWS (i.e., awake but unaware patients) and Minimally Conscious State (MCS), further subdivided into MCS− (basic, non-reflexive responses, e.g., visual pursuit) and MCS+ (e.g., language comprehension, the ability to follow commands, and purposeful behavior) [2]. Diagnostic decision-making in DoC follows international criteria and is supported by standardized tools such as the Coma Recovery Scale-Revised (CRS-R) subscales [3], each of which can independently confer a specific clinical diagnosis in a univariate manner. When patients recover the ability to functionally communicate or use two different objects, they are considered to have emerged from MCS (eMCS [4, 5]). Conversely, when this state persists for longer than 28 days, it is termed prolonged DoC (pDoC), which can last for months or even a lifetime [6, 7].
Once clinically stable, sABI survivors are typically transferred from the Intensive Care Unit (ICU) to an Intensive Rehabilitation Unit (IRU). There, clinicians confront two closely intertwined challenges: accurately predicting patient outcomes to inform relatives and planning individualized care pathways that optimize the resources of the National Health System while addressing ethical and social considerations. In this context, predicting short-term recovery of consciousness is a key factor in defining personalized rehabilitation projects and pathways [8].
Numerous clinical and instrumental predictors of consciousness improvement have been investigated in patients with pDoC [6-9]. Compared to VS/UWS, MCS patients exhibit better short- and long-term functional outcomes [7, 9, 10]. The total CRS-R score at admission to a rehabilitation ward [11] and its progression during the first 4 weeks [12, 13] have been proposed as predictors of consciousness improvement at discharge after a mean hospital stay of 5 months. Recently, there has been growing interest in developing new CRS-R-derived indices, including the CRS-R index [14] and the Consciousness Domain Index (CDI) [15]. The latter also shows potential prognostic value [10, 16]. Both indices are derived from the six CRS-R sub-scores; the CRS-R index is generated via a mathematical transformation that expands its numerical range from 0 to 100, while the CDI uses cross-validated k-means binary clustering. However, the prognostic capability of these indices, in combination with neurophysiological and clinical descriptors, is yet to be examined.
As outlined above, the clinical diagnosis determined using the CRS-R at IRU admission is among the most relevant predictors of short-term outcomes. However, recent guidelines emphasize the importance of a multimodal assessment of consciousness, recommending that clinical evaluation be complemented by at least one instrumental measure [17, 18]. They also highlight the need to integrate neurophysiological and clinical predictors within a multivariate approach [19]. In terms of instrumental assessments, bilateral absence of the cortical component in somatosensory evoked potentials (SSEPs) is regarded as the most reliable indicator of a poor prognosis in anoxic comatose patients [20, 21]. The negative prognostic significance of absent SSEPs for short- and long-term recovery in pDoC has been widely confirmed, especially in post-anoxic etiology [22, 23]. Similarly, classical and advanced EEG features also have demonstrated prognostic value in identifying patients with a better likelihood of recovering or improving consciousness [24]. Notably, EEG recordings performed within the first week after IRU admission, and scored according to the American Clinical Neurophysiology Society (ACNS) terminology, can offer valuable prognostic insights [25, 26]. Among EEG features, background activity classified by the Synek scale [27] in the subacute phase has been associated with a better prognosis for responsiveness at 3 months post-injury, as measured by the Rancho Los Amigos Level of Cognitive Functioning scale [28]. Additionally, the presence of cortical reactivity to eye opening on the baseline EEG has been linked to a higher probability of short-term consciousness improvement (6 months from onset) [9].
In summary, previous studies on the prognosis for recovering consciousness in pDoC populations have frequently had methodological limitations, including retrospective designs, a focus on “improvement of consciousness” rather than “full recovery,” small sample sizes, and a lack of multidimensional approaches. Against this backdrop, the current multisite, prospective, longitudinal study was conducted across four Italian rehabilitation units to identify short-term predictors of full clinical recovery of consciousness (eMCS) through a bedside multimodal assessment (clinical and neurophysiological).
2 Methods
2.1 Study Design
This study was carried out in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology guidelines [29]. This analysis is one of the main endpoints of a multisite prospective observational longitudinal study (PRABI study [30]) that involved 4 IRUs (IRCCS Fondazione Don Carlo Gnocchi ONLUS, Firenze; Polo Specialistico Riabilitativo Fondazione Don Carlo Gnocchi ONLUS, Sant'Angelo Dei Lombardi; IRCCS Fondazione Don Carlo Gnocchi, Centro S. Maria Nascente, Milano; Fondazione Don Carlo Gnocchi, Polo Riabilitativo del Levante ligure, La Spezia) with expertise in the diagnosis and care of adults surviving sABI.
2.2 Aims
The primary aim of this study was to identify clinical and neurophysiological predictors of eMCS at 3 months from study enrollment and to evaluate the prognostic enhancement gained by combining demographic, clinical, and neurophysiological data. Clinical diagnoses at admission and discharge were established according to standardized clinical criteria for VS/UWS, MCS−, and MCS+ using the CRS-R [3]. Given uncertainties regarding the optimal method for extracting prognostic information from the CRS-R scale [10, 14, 15, 31], and the multicenter nature of the data, a secondary aim was to compare the predictive value of various validated methods for interpreting the CRS-R (clinical diagnosis of consciousness, total CRS-R score, CRS-R Index, CDI, and CRS-R sub-scores) when combined with neurophysiological data. In all analyses, the outcome was defined as the complete recovery of consciousness (eMCS) as measured by the CRS-R. Patients who improved but remained in a pDoC state (e.g., transitioning from UWS to MCS−/+) or whose clinical diagnosis remained unchanged or worsened were considered not improved in the statistical analysis.
2.3 Study Population
All patients with sABI admitted to the four Fondazione Don Carlo Gnocchi IRUs from June 10th, 2020, to January 1st, 2023, were screened for eligibility. Inclusion criteria were: (1) age > 18 years; (2) clinical diagnosis of VS/UWS or MCS at admission to the IRU according to CRS-R diagnosis; (3) anoxic, traumatic, vascular (i.e., hemorrhagic or ischemic) or other etiologies; (4) time post-injury ranging from 1 to 4 months. Exclusion criteria were (1) previous history of acquired brain injury or psychiatric (major depression with apathy, psychic akinesia, abulia) or neurodegenerative diseases (dementia of all etiologies); (2) coexisting neoplasms, severe organ dysfunction, or persistently unstable clinical conditions (e.g., hemodynamic instability, severe respiratory failure) that would preclude accurate consciousness assessment.
2.4 Clinical Assessment
At enrolment, each center collected patient demographic data (e.g., age, sex) and information about medical history (e.g., etiology, time post-injury). Within 1 week from study entry (T0), all patients were assessed by skilled investigators by means of repeated (at least 5 in a week) CRS-R evaluations in order to confirm the patients' clinical diagnosis and to determine the best CRS-R sub-scores [32, 33]. The CRS-R investigators were blinded to neurophysiological evaluations. The CRS-R administrations (best out of 5 consecutive evaluations) were performed following international guidelines to reduce misdiagnosis (e.g., use of a mirror, caregiver involvement when possible [34-36]) by experienced and trained personnel. The Disability Rating Scale was also administered at T0 [37]. Patients' follow-up was collected after 3 months from T0 (T1) by repeated CRS-R evaluations conducted by the same clinical staff.
2.5 Neurophysiological Assessment
Experienced neurophysiologists, blinded to the patients' clinical diagnoses, recorded neurophysiological data at T0, including resting-state EEG and SSEPs (for those without this information available from acute-phase medical records).
Standard EEG recordings (30 min in duration) were acquired in accordance with the international 10–20 System using a digital device (Gal NT, EBNeuro). A prewired EEG cap with 19 electrodes (Fp1, Fp2, F7, F8, F3, F4, C3, C4, T3, T4, P3, P4, T5, T6, O1, O2, Fz, Cz, Pz) was used, following previously established EEG recording parameters [25, 26] and a sampling rate of 128 Hz. Recordings with eyes closed included a 10-min resting-state segment and 10 min of clinically administered stimuli (acoustic stimuli calling the patient's name and nociceptive stimuli via nail bed pressure). EEG was performed in the morning at the bedside after routine nursing procedures and at least 10 h after the administration of central nervous system–active drugs (e.g., muscle relaxants, sedatives such as benzodiazepines, neuroleptics) to optimize vigilance. Long-term antiseizure treatment was continued as clinically indicated.
Recordings were filtered with a low-pass filter (cut-off frequency 30–70 Hz) and a high-pass filter (time constant 0.1–0.3 s), adjusted for interpretative needs (standard gain set to 7 V/mm, sensitivity gain 2–10 V/mm). EEG labeling was performed by consensus between two expert neurophysiologists, blinded to CRS-R evaluations, in accordance with the American Clinical Neurophysiology Society (ACNS) Critical Care EEG terminology [38]. Any disagreements were resolved through discussion, guided by Hirsch et al. [38]. The following EEG descriptors were assessed: background voltage and frequency, the presence or absence of an anterior–posterior gradient, cortical reactivity, and brain symmetry, all of which are known to be crucial for diagnosing and prognosticating pDoC [25, 26]. Frequency was coded as theta or alpha; while voltage was coded as normal or low-voltage (most or all activity < 20 V). Anteroposterior gradient (APG) was defined as presen, when a clear and persistent (at least 1 continuous minute) anterior to posterior gradient of voltages and frequencies was present (lower voltage, faster frequencies are seen in anterior derivations and the opposite in posterior ones), reverse (opposite of present) or absent; continuity as present or absent (presence of a pattern of attenuation/suppression alternating with higher voltage activity, with more than 10% of the record consisting of attenuation or suppression); cortical reactivity as present (change in voltage or frequency, including attenuation conditioned to a stimulus) or absent. Patients were labeled as asymmetric whenever (1) a consistent asymmetry in amplitude (on referential recording of 50%) or (2) a consistent asymmetry in frequency (of 0.5–1 Hz) was found for the majority (more than 50%) of the record. For further details on EEG descriptors, see Hirsch et al. [38].
SSEPs were recorded during electrical stimulation of the patients' median nerve, delivered by means of a bipolar surface electrode placed on the patients' right and left wrists. Stimulation intensity was set to 4/3 of individual motor threshold. Each pulse lasted 0.2 ms and was delivered with a 3 Hz rate (time base 50 ms; bandwidth 5 Hz–3 KHz). Recording stainless steel needle electrodes or silver cups were placed at Erb's point (referred to contralateral Erb's point), spinous process Cv7 (referred to anterior neck), C39 and C49 (referred to each other and to Fz). At least 2 averages of 300 responses were repeated and superimposed. The presence or absence of N20/P25 cortical components was evaluated.
2.6 Rehabilitation
The rehabilitation intervention is defined in an individualized care pathway based on the International Classification of Functioning, Disability, and Health-World Health Organization (ICF 2001, WHO) model of functioning [39]. For all involved centers, the rehabilitation intervention follows National Healthcare guidelines [40] and the Department of severe Acquired Brain Injuries of Fondazione Don Gnocchi guidelines. In short, the rehabilitation path and process of care were provided according to the national requirements. In particular, at least 3 h per day of tailored rehabilitation were provided, including physiotherapy for motor stimulation and speech therapy for cannula weaning. Auditory, visual, and sensory stimulations were administered with the dual purpose of performing the CRS-R assessment and stimulating the patient. Weekly team revisions of the individual rehabilitation pathway, emerging needs during the rehabilitation stay, and the type of aid the patients needed were determined based on a systematic screening at admission. Pharmacological neuromodulation was used in the absence of contraindications, and non-pharmacological neuromodulation was never used.
2.7 Statistical Analysis
Descriptive statistics were reported in terms of medians and interquartile ranges (IQR) for continuous variables and in terms of counts and percentages for categorical variables. Descriptive statistics were also reported for each diagnostic group (VS/UWS, MCS−, MCS+) and for each etiology (Traumatic and non-Traumatic). Clinical and neurophysiological predictors were compared across diagnostic groups using the Kruskal–Wallis test for numerical predictors and Chi-Square for categorical ones. Post hoc tests were conducted to assess pair-wise differences, with Dunn post hoc after Kruskal–Wallis and z-tests for multiple proportions after Chi-Square. All post hoc analyses were False Discovery Rate (FDR)-corrected with the Bonferroni correction. Predictors were also compared between TBI/nTBI patients via Mann–Whitney and Chi-Square analysis. With regard to inferential statistics, the dependent variable was set to presence/absence of a pDoC at T1. Univariate logistic regressions were performed between demographic, clinical (CRS-R sub-items) and EEG ACNS descriptors and the outcome. Then, different sets of independent variables were created to perform multivariate logistic regressions and evaluate the model performances in explaining the outcome variance. In particular, the following three datasets were used as independent variables: (1) CRS-R only; (2) ACNS labeling only; (3) CRS-R and ACNS labeling. Models were evaluated via Nagelkerke's R2 and the −2 Log Likelihood. All tests are performed on SPSS v. 28 and significance level α was set to 0.05 for all tests.
2.8 Standard Protocol Approvals and Patient Consents
The institutional review board of the coordinating center and of each center involved in the study reviewed and approved the same outline of the project, shared by all centers and translated in the respective languages. This study was then approved by the ethical standards committee of the coordinating center Florence: N. 16606OSS; Santa Maria Nascente: N. 21/2020/CeFdG/FC/SA; Sant'Angelo dei Lombardi: N. 1560 amendment N. 1888; La Spezia: N. 625/2020 and performed according to the ethical standards of the Declaration of Helsinki and its later amendments.
The surrogate decision-makers of the patients enrolled in the study provided their written informed consent after a semi-formalized interview in which the purposes, procedures, and time points of the longitudinal study were clearly explained. The original forms were collected and stored at each participant center.
3 Results
3.1 Admission Clinical and Neuro-Physiological Descriptors
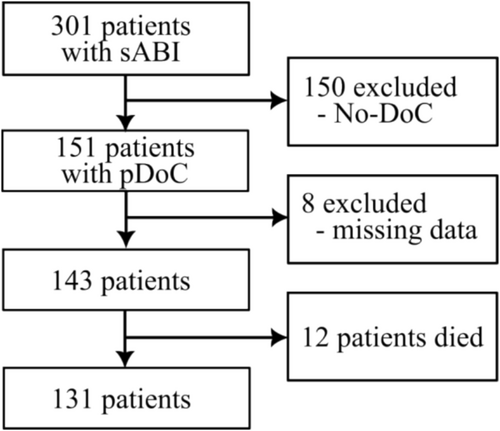
Out of 301 patients admitted in the 4 IRUs from 10.06.2020 to 01.01.2023, 151 pDoC patients fulfilled the inclusion criteria (Figure 1); 8 were discarded due to missing data and 12 died during their permanence in the IRU. One hundred thirty one patients were included and were distributed as follows: Clinical diagnosis of consciousness: 51 (38.93%) VS/UWS, 29 (22.13%) MCS−, and 51 (38.93%) MCS+; Sex: 76 (58.0%) males; etiology: 33 (25.19%) traumatic, 14 (10.68%) anoxic, 24 (18.32%) ischemic, 55 (41.98%) hemorrhagic, 5 (3.81%) mixed; median age: 69 years [IQR = 23] and median time post-onset (TPO) of 40 days [IQR = 23]. The overall sample was found to have a median DRS total score of 24 [IQR = 4].
Based on the clinical diagnosis at T0 (VS/UWS, MCS−, MCS+) and on the etiology (Traumatic/non-Traumatic), clinical and neurophysiological characteristics of the sample are described in Table 1. CRS-R sub-scales were found to be significantly different among consciousness groups (p < 0.05). Post hoc analysis showed significant differences between all diagnostic groups pairwise comparisons for what concerns the auditory sub-scale. Visual, motor, and arousal sub-scales were found significantly lower in VS/UWS patients compared to MCS− and MCS+ ones, with no significant differences between the MCS+ and MCS– conditions. Conversely, on the oro-motor and communication sub-scale, no differences were detected between VS/UWS and MCS− patients, with the values of MCS+ patients significantly higher than those of VS/UWS and MCS− ones (p < 0.05). When comparing demographic and clinical descriptors between etiologies, a younger age (p = 0.001) was found in TBI patients (median 56 [IQR = 38]) compared to nTBI (median 70 [IQR = 17]). Concerning neurophysiologic findings, most patients had an α background (N = 106; 80.9%) with a normal amplitude (N = 102; 77.9%). The presence of cortical reactivity and of an APG was respectively found in 93 (71.0%) and 74 (56.5%) pDoC patients (Table 1). Low-voltage EEG backgrounds were found to be significantly predominant in VS/UWS patients (21, 41.2%) compared to MCS− (3, 10.3%) and MCS+ (5, 9.8%). Similarly, in a subgroup of 93 pDoC (37 MCS+, 23 MCS−, 33 VS/UWS), VS/UWS patients reported a significantly smaller percentage of SSEP presence (15, 45.5%) compared to MCS− (23, 100%) and MCS+ (35, 94.6%) patients. Significant differences (FDR corrected, p < 0.05) in SSEP presence were only detected between MCS−/+ and UWS patients but not between MCS− and MCS+ (Table 1).
| Total (N = 131) | Clinical diagnosis | Etiology | ||||
|---|---|---|---|---|---|---|
| MCS+ (N = 51) | MCS− (N = 29) | UWS (N = 51) | TBI (N = 33) | nTBI (N = 98) | ||
| Age, yearsB | 69 [23] | 68 [21] | 71 [25] | 69 [26] | 56 [38] | 70 [17] |
| Sex, male | 76 (58.0) | 32 (62.7) | 12 (41.4) | 32 (62.7) | 22 (66.7) | 54 (55.1) |
| Etiology, TBI | 33 (25.2) | 18 (35.3) | 4 (13.8) | 11 (21.6) | — | — |
| TPO, days | 40 [23] | 47 [25] | 38 [19] | 40 [23] | 40 [19] | 40 [25] |
| DRS, points | 24 [4] | 22 [4]a | 22.5 [3]a | 24 [2]b | 24 [4] | 24 [4] |
| CRS-R auditoryA | 1 [2] | 3 [2]a | 2 [1]b | 1 [1]c | 2 [2] | 1 [2] |
| CRS-R visualA | 1 [2] | 3 [2]a | 2 [2]a | 1 [1]b | 1 [2] | 1 [2] |
| CRS-R motorA | 2 [3] | 4 [2]a | 3 [2]a | 1 [1]b | 2 [3] | 2 [3] |
| CRS-R oro-mot.A | 1 [0] | 2 [1]a | 1 [0]b | 1 [0]b | 1 [1] | 1 [0] |
| CRS-R comm.A | 0 [0] | 1 [1]a | 0 [0]b | 0 [0]b | 0 [1] | 0 [0] |
| CRS-R arousalA | 2 [1] | 2 [1]a | 2 [1]a | 1 [1]b | 2 [1] | 2 [1] |
| CRS-R totalA | 8 [8] | 14 [5]a | 9 [3]b | 5 [2]c | 8.5 [8] | 8 [9] |
| Frequency, αA | 106 (80.9) | 36 (70.6)a | 26 (89.7)a | 44 (86.3)a | 26 (78.8) | 80 (81.6) |
| APG, present | 74 (56.5) | 29 (56.9)a | 17 (58.6)a | 28 (54.9)a | 17 (51.5) | 57 (58.2) |
| Cortical react., presentA | 93 (71.0) | 37 (72.5)a,b | 26 (89.7)b | 30 (58.8)a | 21 (63.6) | 72 (73.5) |
| Voltage, lowA | 29 (22.1) | 5 (9.8)a | 3 (10.3)a | 21 (41.2)b | 7 (21.2) | 22 (22.4) |
| SSEP, presentA | 73 (78.5) | 35 (94.6)a | 23 (100)a | 15 (45.5)b | 19 (79.2) | 54 (78.3) |
- Note: Medians and interquartile ranges (in brackets) are reported for continuous variables while counts and percentages (in parenthesis) are reported for categorical variables. SSEP data refer to a subgroup of 93 pDoC patients with this assessment. a,b,cColumns not sharing the same subscript are significantly different in the post-hoc analysis after Bonferroni correction.
- Abbreviations: APG, anteroposterior gradient; CRS-R, Coma Recovery Scale-Revised; DRS, Disability Rating Scale; MCS, minimally conscious state; nTBI, non TBI; SSEP, somatosensory evoked potentials; TBI, traumatic brain injury; TPO, time post-onset; UWS, Unresponsive Wakefulness Syndrome.
- A Significant difference among diagnostic groups.
- B Significant difference between TBI/nTBI.
3.2 Clinical Evolution at T1
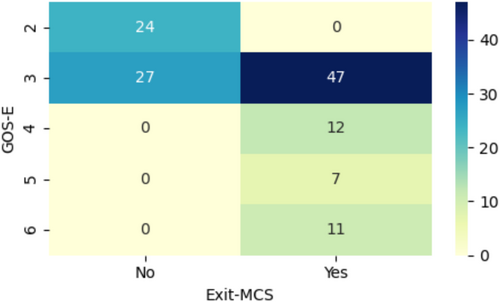
At T1, 77 (58.8%) patients had recovered full consciousness (eMCS). Among the remaining 54 patients who did not reach eMCS, 10 showed partial improvement (6 UWS to MCS−, 3 UWS to MCS+, 1 MCS− to MCS+) while 7 deteriorated (1 MCS− to UWS, 4 MCS+ to MCS−, and 2 MCS+ to UWS). The remaining 37 patients exhibited no change in clinical diagnosis of consciousness (4 MCS+, 6 MCS−, 27 UWS). Of the 77 patients who attained eMCS at T1 (Figure 2), 59 (76.6%) patients reached GOS-E ≤ 4 (GOS-E = 3: 47 patients, GOS-E = 4: 12 patients) and 18 (23.4%) patients reached GOS-E > 4 (GOS-E = 5: 7 patients, GOS-E = 6: 11 patients).
3.3 Predictors of Consciousness Recovery at T1
In univariate logistic regressions (Table 2), no demographic variables were significantly associated with eMCS at T1 (p > 0.05), apart from sex (females had a better outcome; p = 0.043, OR = 2.118, 95% CI: 1.024–4.385). All individual CRS-R sub-scores were significantly correlated with eMCS at p < 0.01, except the communication item (p = 0.027). Concerning EEG ACNS descriptors, the presence of cortical reactivity (OR = 4.244, CI: 1.905–9.455, p < 0.001) and of regular amplitude in the EEG background (OR = 3.003, CI: 1.280–7.042, p = 0.012) were found to be associated with the recovery of consciousness. SSEP presence was also found to be strongly associated with a favorable outcome (p = 0.003).
| OR | 95%CI | p | |
|---|---|---|---|
| Age, years | 1.006 | 0.985–1.028 | 0.566 |
| Sex, female | 2.118 | 1.024–4.385 | 0.043 |
| Etiology, TBI | 1.262 | 1.261–2.793 | 0.568 |
| TPO, days | 0.991 | 0.975–0.991 | 0.293 |
| DRS, points | 0.700 | 0.586–0.836 | < 0.001 |
| CRS-R auditory | 2.248 | 1.553–3.253 | < 0.001 |
| CRS-R visual | 2.286 | 1.633–3.202 | < 0.001 |
| CRS-R motor | 1.804 | 1.357–2.397 | < 0.001 |
| CRS-R oro-motor | 2.847 | 1.468–5.523 | 0.002 |
| CRS-R comm. | 2.860 | 1.126–7.263 | 0.027 |
| CRS-R arousal | 2.511 | 1.476–4.271 | 0.001 |
| CRS-R total score | 1.334 | 1.193–1.491 | < 0.001 |
| Clinical diagnosis, MCS | 8.267 | 3.719–18.377 | < 0.001 |
| CRS-R Index | 1.054 | 1.031–1.077 | < 0.001 |
| CDI | 7.729 | 3.464–17.246 | < 0.001 |
| Frequency, α | 1.629 | 0.647–4.104 | 0.301 |
| APG, present | 2.315 | 1.136–4.719 | 0.021 |
| Cortical reactivity, present | 4.244 | 1.905–9.455 | < 0.001 |
| Voltage, normal | 3.003 | 1.280–7.042 | 0.012 |
| SSEP, present | 5.076 | 1.730–12.925 | 0.003 |
- Note: Outcome is set to presence/absence of pDoC at T1. Absence of a pDoC is coded as 0, thus OR > 1 indicates that higher values of the related independent variable lead toward an eMCS state. Significant variables (p < 0.05) were indicated with bold text.
- Abbreviations: APG, anteroposterior gradient; CI, confidence interval; CRS-R, Coma Recovery Scale-Revised; DRS, Disability Rating Scale; OR, odds ratio; SSEP, somatosensory evoked potentials; TBI, traumatic brain injury; TPO, time post-onset.
Multivariate analyses including different sets of variables (i.e., clinical, neurophysiological, or both) were conducted in the full dataset (N = 131). Age, sex, TPO, and etiology were included in all analyses as covariates given their association with the consciousness outcome [9]. The multivariate regression including CRS-R sub-scores and demographic factors (Table 3A) resulted in only the visual CRS-R being independently correlated with the outcome (OR = 2.559, CI = 1.405–4.660, p = 0.002), also surviving FDR correction (pADJ = 0.02). When including only ACNS descriptors together with demographic variables (Table 3B), only the presence of cortical reactivity (p < 0.001) survived FDR correction. Conversely, the model including EEG and CRS-R descriptors showed that a higher CRS-R visual sub-score (OR = 2.146, CI: 1.124–4.096, p = 0.021), the presence of cortical reactivity (p = 0.020), and female sex (p = 0.040) were found to be independently correlated to exiting from a pDoC (Table 3C). The EEG model (B) was found to be one with the lowest correlation with the outcome (R2 = 0.291). On the other hand, the clinical model (A) and the clinical/EEG model (C) were found to have R2 = 0.439 (−2LL = 125.889) and R2 = 0.505 (−2LL = 115.964), respectively. All three multivariate models satisfied the Omnibus Tests of Model Coefficients (p < 0.05) showing significant improvements with respect to the baseline (p < 0.05). Using all the CRS-R subscales (Table 3C) simultaneously was found to be the most profitable way to express consciousness in terms of explained variance of the outcome compared to any other CRS-R derived index.
| OR | 95%CI | p | |
|---|---|---|---|
| A: R2 = 0.458, −2LL: 122.387 | |||
| CRS-R auditory | 0.902 | 0.470–1.729 | 0.756 |
| CRS-R visual | 2.464 | 1.354–4.483 | 0.003* |
| CRS-R motor | 1.025 | 0.684–1.537 | 0.904 |
| CRS-R oro-motor | 2.373 | 0.834–6.749 | 0.105 |
| CRS-R communication | 0.513 | 0.112–2.342 | 0.389 |
| CRS-R arousal | 1.052 | 0.486–2.279 | 0.898 |
| DRS, points | 0.820 | 0.656–1.026 | 0.083 |
| Age, years | 0.999 | 0.971–1.027 | 0.934 |
| Sex, female | 2.381 | 0.930–6.097 | 0.070 |
| Etiology, TBI | 1.248 | 0.387–4.016 | 0.711 |
| TPO, days | 0.986 | 0.965–1.007 | 0.188 |
| B: R2 = 0.291, −2LL: 145.686 | |||
| Frequency, α | 1.327 | 0.465–3.785 | 0.597 |
| APG, present | 1.027 | 0.422–2.501 | 0.953 |
| Cortical reactivity, present | 8.245 | 2.831–24.011 | < 0.001* |
| Voltage, normal | 1.782 | 0.660–4.830 | 0.254 |
| Age, years | 0.995 | 0.969–1.021 | 0.684 |
| Sex, female | 2.491 | 1.072–5.791 | 0.034 |
| Etiology, TBI | 1.205 | 0.460–3.154 | 0.704 |
| TPO, days | 0.991 | 0.973–1.009 | 0.307 |
| C: R2 = 0.520, −2LL: 113.055 | |||
| CRS-R auditory | 0.986 | 0.468–2.079 | 0.971 |
| CRS-R visual | 2.076 | 1.092–3.947 | 0.026 |
| CRS-R motor | 1.042 | 0.660–1.646 | 0.860 |
| CRS-R oro-motor | 2.359 | 0.805–6.916 | 0.118 |
| CRS-R communication | 0.516 | 0.111–2.406 | 0.400 |
| CRS-R arousal | 0.899 | 0.390–2.068 | 0.802 |
| DRS, points | 0.828 | 0.656–1.045 | 0.111 |
| Frequency, α | 1.330 | 0.373–4.748 | 0.660 |
| APG, present | 1.488 | 0.483–4.580 | 0.488 |
| Cortical reactivity, present | 4.678 | 1.257–17.412 | 0.021 |
| Voltage, normal | 1.024 | 0.311–3.378 | 0.968 |
| Age, years | 0.990 | 0.959–1.022 | 0.535 |
| Sex, female | 2.863 | 1.008–7.692 | 0.048 |
| Etiology, TBI | 1.081 | 0.925–3.610 | 0.967 |
| TPO, days | 0.982 | 0.964–1.009 | 0.246 |
- Note: Outcome is set to presence/absence of pDoC at T1. Absence of a pDoC is coded as 0, thus OR > 1 indicates that higher values of the related independent variable lead toward an eMCS state. Significant variables (p < 0.05) were indicated with bold text. An asterisk near the p-value indicates that significance is retained after Bonferroni correction.
- Abbreviations: APG, anteroposterior gradient; CI, confidence interval; CRS-R, Coma Recovery Scale-Revised; DRS, Disability Rating Scale; OR, odds ratio; SSEP, somatosensory evoked potentials; TBI, traumatic brain injury; TPO, time post-onset.
Lastly, the analysis in Table 3B,C was performed on a selected subgroup of patients (N = 93) who had the SSEP assessment. Results were reported in Table S2. In particular, reactivity and presence of SSEP were all associated with a favorable outcome despite not surviving the Bonferroni adjustment.
4 Discussion
In the present prospective study, 58.8% of patients admitted with a pDoC to the IRUs recovered full consciousness at T1 and 8.1% improved their clinical diagnosis without emerging from MCS. The visual sub-item of the CRS-R and the detection of EEG reactivity to eye opening at T0 were identified as the most significant markers of short-term recovery of full consciousness. The proportion of patients recovering full consciousness is not clearly stated in the previous literature, mostly due to the heterogeneity in outcome selection (i.e., improvement of clinical diagnosis) [19] and/or withdrawal of life supports. Nevertheless, it is noteworthy that a substantial proportion of pDoC patients reached an eMCS during the first few months after the acute event [12], which supports the importance of early intensive rehabilitation in pDoC patients [41, 42]. The present multisite study, by using a multimodal consciousness assessment, identified the visual subscale of the CRS-R and EEG cortical reactivity to eye opening as the most relevant predictors of an early complete recovery of consciousness.
Previous studies have highlighted the relevance of the CRS-R score at T0 for predicting a short-term improvement in consciousness [12]. However, most of the studies investigating the predictive value of the clinical assessment relied only on the CRS-R total score [9, 25], thereby preventing an accurate identification of the most significant behavioral correlate of recovery. Among the clinical responses within the CRS-R scale [3] and individually included in the present study, the visual response at T0 was found to be most frequently associated with a recovery of consciousness at T1. Early detection of visual signs of consciousness in individuals transitioning from VS/UWS to MCS has been documented previously: some studies conducted in both rehabilitation centers and long-term care facilities showed that the diagnosis of consciousness was made thanks to visual signs alone in 55% to 83% of the samples [43, 44]. Visual fixation and pursuit were also the most frequently observed markers of consciousness to emerge (57% and 52% of cases, respectively) in a chronic MCS sample [45] and in a chronic VS/UWS sample admitted to rehabilitation programs [46]. However, this is the first study that disentangles the independent predictive nature of these visual signs from other demographic and neurophysiological factors.
Then, to identify the most relevant clinical marker of recovery, analyses were performed including in turn the total CRS-R score, the CRS-R index, the CDI, and the clinical diagnosis. We observed that none of these CRS-R-derived markers provided a better estimate than the individual sub-items when considered together. This finding aligns with a recent study that investigated the prognostic value of various CRS-R-based metrics using a machine learning analysis and concluded that the sub-items were superior [31].
Regarding the call for multimodality in pDoC diagnosis and prognosis [17, 18, 47], including EEG in the analysis demonstrated the superiority of cortical reactivity to eye opening in predicting eMCS at T1 compared to all other neurophysiological descriptors. This outcome is consistent with a recent review showing that, among different neurophysiological responses, only oscillatory EEG responses to passive stimulation appear to be reliably related to both prognostic criteria (i.e., minimal clinical improvement and the recovery of full consciousness) [19]. That review also found that cortical reactivity was the only predictor with significant predictive value for both the transition from UWS/VS to MCS and the recovery of consciousness. SSEPs are recognized as outcome predictors for acute coma [48, 49] and for the transition from UWS to MCS but not specifically for the recovery of consciousness. Furthermore, SSEP absence seems to have a notably higher negative predictive power compared to the positive predictive power of SSEP presence [50-52], despite retaining high predictive accuracy for outcomes after cardiac arrest [53].
Another important finding of this study involves the functional status achieved by eMCS patients. While considering complete recovery of consciousness as the outcome, it is important to emphasize that a substantial proportion of patients remained severely disabled at T1. Indeed, as shown in the results, although about a quarter (23.4%) of eMCS patients attained moderate disability (GOS-E > 4) at T1, the majority (76.6%) continued to exhibit extremely severe disability (GOS-E < 4). These results highlight the complexity of distinguishing, especially when communicating with caregivers, between the probability of regaining consciousness and the potential for achieving other functional outcomes that might be even more relevant to patients and families [19, 54]. Indeed, regardless of consciousness recovery (which also implies the recovery of communication), the reduction in disability burden and the restoration of individual autonomy are arguably the most pertinent factors for supporting family members and clinicians in formulating post-IRU care management.
Several limitations of this work should be acknowledged. First, we did not include any neuroimaging instruments in assessing consciousness and thus could not detect covert consciousness or its evolution [55]. On the other hand, EEG techniques are inexpensive, can be performed at the bedside, and are widely available in rehabilitation settings [56, 57]. Additionally, the analysis of Event-Related Potentials (ERPs) was not part of this study. ERPs such as P300 and Mismatch Negativity (MMN), although beneficial for assessing cognitive processes, require advanced technical and medical expertise for acquisition and interpretation, along with specialized equipment that is not universally accessible. In contrast, resting-state EEG is routinely utilized across centers, including those without dedicated neurophysiology expertise, thus facilitating standardized and practical data collection. This practical consideration aligns with the need to balance scientific rigor and logistical constraints in large-scale multicenter studies. Moreover, although P300 and MMN have demonstrated fair positive predictive value for consciousness recovery, their diagnostic utility is limited by low sensitivity, potentially resulting in false negatives in patients with DoC [58]. Resting-state EEG, by contrast, has shown promise for detecting functional and structural disruptions in brain networks linked to consciousness and is increasingly recognized as a robust tool for prognostic assessments [59]. Grouping “patients who did not improve or worsened” together could introduce a minor bias related to clinical determinants, such as secondary events or increased medical complexity, that affect consciousness outcomes. However, given the low incidence of such cases (5.34%) and our primary focus on full recovery, further subgrouping was deemed unnecessary. Lastly, EEG recordings were conducted in the morning—after routine nursing procedures and at least 8 h following sedative administration—to optimize vigilance, with expert neurophysiologists evaluating the recordings for sleep-related EEG patterns.
In conclusion, this study reaffirms the importance of multimodal assessment of consciousness in prognostication while emphasizing the prognostic role of the CRS-R subscales. Using the recovery of full consciousness as the outcome, this work provides clinically and functionally relevant insights to guide clinicians in planning rehabilitation pathways and communicating with patients' relatives.
Author Contributions
Bahia Hakiki: conceptualization, investigation. Piergiuseppe Liuzzi: conceptualization, investigation, methodology, software, formal analysis. Anna Maria Romoli: data curation, investigation. Francesca Draghi: data curation. Daniela Maccanti: data curation. Agnese De Nisco: data curation. Rachele Burali: data curation. Tanita Toci: data curation. Antonello Grippo: writing – review and editing, investigation, methodology. Maenia Scarpino: writing – review and editing. Andrea Mannini: funding acquisition, project administration, writing – review and editing, methodology. Alfonso Magliacano: writing – original draft, data curation. Anna Estraneo: writing – review and editing, methodology, supervision, investigation. Angela Comanducci: data curation, writing – review and editing. Jorge Navarro: supervision, investigation, writing – review and editing. Caterina Tramonti: data curation, writing – review and editing. Valentina Carli: data curation, writing – review and editing. Pietro Balbi: writing – review and editing, supervision. Claudio Macchi: writing – review and editing. Francesca Cecchi: writing – review and editing, project administration, supervision.
Acknowledgements
The authors would like to thank Prof. Sandro Sorbi for his support and Dr. Chiara Fanciullacci for assisting with administrative/ethical issues. Open access funding provided by BIBLIOSAN.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
Data are available from the corresponding authors upon reasonable request.




