Cerebral aneurysm: De novo genesis and rupture within 15 days
Abstract
We report the first case of de novo formation of a small 4- × 3-mm symptomatic aneurysm with subsequent subarachnoid haemorrhage (SAH) within 15 days. A pre-existing aneurysm was excluded by magnetic resonance angiography, as well as conventional angiography. In this case, there was no history of SAH, which is in contrast to other reported cases of de novo aneurysms that developed after previous aneurysm rupture.
Abbreviations
-
- MMP
-
- matrix metalloproteinase
-
- SAH
-
- subarachnoid haemorrhage
-
- WSS
-
- wall shear stress
INTRODUCTION
A de novo aneurysm is a newly formed lesion that develops from a vessel known to be normal from previous imaging studies. Little is known about the aetiology and the dynamic of de novo aneurysm formation. Graf and Hamby [1] reported the first de novo aneurysm and presumed that such aneurysms “develop on the basis of some congenital peculiarity in the vessel walls … influenced by variable, vaguely understood, post-natal circulatory changes”. In recent years, it has been shown that cerebral aneurysms are mainly acquired. Risk factors such as arterial hypertension and smoking induce endothelial damage promoting increased shear stress at vascular bifurcations, inflammation and tissue degeneration, with subsequent dilatative “remodelling” of the arterial wall [2]. We report the first case of a de novo formation of a 4-mm symptomatic aneurysm with subsequent subarachnoid haemorrhage (SAH) within 15 days.
CASE REPORT
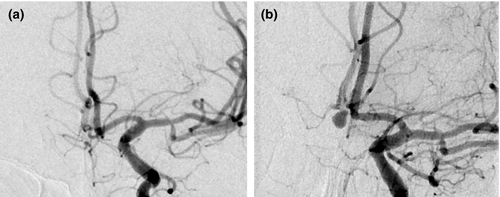
A 59-year-old female patient received angioplasty and stenting of a left high grade (80%; North American Symptomatic Carotid Endarterectomy Trial [NASCET]) asymptomatic carotid stenosis. She was discharged and readmitted 15 days thereafter with a SAH Hunt and Hess Grade V from a newly diagnosed 4- × 3-mm aneurysm of the anterior communicating artery (Figure 1). Retrospective analysis of the first angiography excluded a pre-existing aneurysm. Risk factors were hypertension and smoking.
DISCUSSION
To the best of our knowledge, this is the first case of de novo formation with aneurysm rupture within 15 days in a patient without a history of SAH. A pre-existing aneurysm was excluded by magnetic resonance angiography, as well as conventional angiography.
The patient had recorded hypertension, arteriosclerosis and a history of smoking. These factors may reduce the ability of the cerebral vasculature to adequately adapt to changes in haemodynamic stress. The angioplasty and stenting of the high grade carotid stenosis is probably a mechanical stress factor that increased wall shear stress (WSS).
Endothelial cells are highly sensitive to WSS. An abnormal WSS can result in vascular remodelling by endothelium-mediated proinflammatory responses and additional matrix metalloproteinase (MMP) activation, leading to extracellular matrix degradation. Therefore, cerebral vasculature is prone to the effects of haemodynamic forces due to a sparse tunica adventitia and a lower proportion of elastic fibres [3]. Animal experiments have shown that MMPs are involved in the early development of aneurysms. In particular, MMP-2 and MMP-9, produced by smooth muscle cells, were found to be upregulated in areas with loss of internal elastic lamina and media thinning [4]. These processes might have contributed to the fast aneurysm formation in our case.
Interestingly, the aneurysm was rather small. Prospective studies have shown that small unruptured aneurysms carry a lower risk of rupture [5]. Paradoxically, most ruptured aneurysms are likewise small in daily clinical routine [6]. Rapidly growing and rupturing de novo intracranial aneurysms might be one explanation for the apparent paradox. Intracranial aneurysms might be especially prone to rupture during the early remodelling phase [7]. Histological studies reveal that, due to acute stretching, the aneurysmal wall is thinned out with signs of inflammation and degradation [8]. Cases like this are probably much more frequent but rarely observed due to their nature.
ACKNOWLEDGEMENTS
This article published with the written authorization of the family.
CONFLICT OF INTEREST
The authors have no financial or other conflicts of interest to disclose.
AUTHOR CONTRIBUTIONS
Justine Münsterberg: Asklepios Klinik Altona, Hamburg, Germany: manuscript draft and revision. Joachim Röther: Asklepios Klinik Altona, Hamburg, Germany: manuscript draft and revision. Bernd Eckert: Asklepios Klinik Altona, Hamburg, Germany: manuscript revision. All co-authors have read and approved its submission in the present form.
Funding information
No funding was required for this paper.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.




