Neurological level at birth predicts survival to the mid-40s and urological deaths in open spina bifida: a complete prospective cohort study
Abstract
Aim
To conduct a 50-year complete, community-based, prospective cohort study to investigate long-term survival, causes of death, and influence of level of the lesion in treated open spina bifida.
Method
The cohort comprised 117 consecutive cases whose backs were closed non-selectively at birth between 1963 and 1971 in Cambridge, UK. In 2013 we surveyed the survivors (n=39, 18 males, 21 females; mean age 46y, range 43–49y) by postal questionnaire and telephone interview. We compared outcomes in those born with a neurological deficit in terms of sensory and motor levels of L1 and above versus L2 and below.
Results
Two-thirds of the cohort (78/117) had died. Causes of death were cardiorespiratory (n=26), neurological (n=24), urological (n=22), or other (n=6). Only the urological deaths were related to level of the lesion: there were none in those with a sensory level of L2 or below (p<0.001). Birth findings also predicted survival: of the 57 infants with a neurological level of L1 or above, only 12% (n=7) survived compared with 55% (30/55) of the remainder (p<0.001).
Interpretation
The increased mortality in those born with an extensive neurological deficit was mainly due to urological deaths. Neurological level, particularly the sensory level, is the best predictor of long-term outcome and should be assessed routinely at birth.
What this paper adds
- In open spina bifida, sensory level predicts urological life expectancy.
- Death due to urological causes only occurred in those with a sensory level of T6–L1.
- Neurological level predicts outcome better than cutaneous or radiological level.
- Sensory level should be assessed in all infants with open spina bifida.
This article is commented on by Worley on pages 594–595 of this issue.
The worldwide estimated incidence of open spina bifida varies between 1 and 16 per 10 000 births.1, 2 A recent population-based study estimated there were 25 000 children and adolescents aged between 0 years and 19 years living with spina bifida in the USA.3 Reliable data on long-term survival and the influence of the level of the lesion at birth are crucial for doctors, patients, parents, care planners, and health insurers.3, 4 While it is has long been accepted that higher lesions are associated with greater disability and mortality,5 there is continuing controversy over whether cutaneous (external), radiological (bony), motor, or sensory level is the most useful predictor of outcome.1, 3, 6-11
In 1963 a prospective study of open spina bifida was set up in Cambridge, UK, to investigate the effect on outcome of early non-selective closure of the back and insertion of a cerebrospinal fluid shunt for hydrocephalus when required.12 In 2013 we reviewed the complete cohort to investigate survival up to 50 years, causes of death, and relation with level of the lesion at birth.
Method
Participants
As previously described,10 the cohort comprised 117 consecutive infants (50 males, 67 females) with open spina bifida who were treated unselectively at Addenbrooke's Hospital, Cambridge, UK between 1963 and 1971. After a detailed neurological examination, including assessment of sensory, motor, cutaneous, and radiological levels, their backs were closed within 48 hours of birth.12 At operation the open lesion was found to be a simple meningocele with no neural tissue in the sac in four infants. If required, a cerebrospinal fluid shunt was inserted. This was done in 89% (82/92) of those who reached the age of 1 year.10, 13 The cohort has been regularly reviewed with no loss to follow-up.10, 14-16
Data collection
In 2012 to 2013 we conducted a confidential postal questionnaire survey of the survivors backed by telephone interview with the patient or carer. (These data will be reported separately). Details of recent deaths were obtained from the Health and Social Care Information Centre (flagged cohort reference MR564) backed by information from medical records and autopsy reports.10
Ethical review
The NRES Committee East of England-Cambridge East reviewed the study (Reference 07//Q0104/11).
Statistical analysis
In line with other studies5, 7, 8 we divided the cohort into those born with a motor level or sensory level of L1 and above (i.e. no quadriceps activity or no sensation below the inguinal ligament) versus L2 and below. At this cut-off there was 79% (92/117) agreement between motor and sensory levels. Where sensory and motor levels were different, we followed recent recommendations to prioritize sensory level as it tends to be more reliably assessed and remains stable over time.11
We examined the relation between neurological deficit in infancy (L1 or above vs L2 and below) with survival using Kaplan–Meier curves and the log-rank test, and with cause of death using Fisher's exact test. We also described the level of the lesion in terms of cutaneous, radiological, motor, and sensory level in those with urological-related deaths.
Results
Overall survival
Ascertainment of survival was 100%. Of the original cohort of 117 cases, only 39 (33%) were still alive in July 2013. The mean age of the survivors was 46 years (range 43–49y); 18 (46%) were male and 21 (54%) were female. Thirty eight cases (97%) were followed up by postal or telephone questionnaire to patient or carer. Of the 78 deaths, 40 (51%) had occurred before the age of 5 years. The median survival time was 28.5 years.
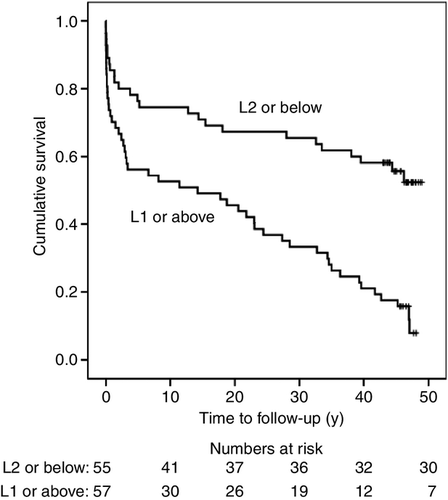
Figure 1 gives Kaplan–Meier survival curves for those born with a neurological deficit in terms of sensory level of L1 and above versus L2 and below. Five cases born with asymmetrical sensory levels were excluded. Only 12% (7/57) of those born with a sensory level of L1 and above survived to the mean age of 46 compared with 55% (30/55) of the remainder (log rank p<0.001).
Causes of death related to neurological deficit in infancy
The causes of the 78 deaths were: cardiorespiratory (n=26); neurological (n=24; acute hydrocephalus [n=10], central nervous system infection [n=10], epilepsy [n=4]); urological (n=22); other causes (n=6; inhaled vomit [n=2], sudden infant death [n=1], thrombocytopenic purpura [n=1], carcinoma of the cervix [n=1], malignant melanoma [n=1]).
Table 1 gives causes of death in those with high, low, and asymmetrical sensory and motor levels. Causes of death were similar in those with high and low neurological levels except for urological deaths. Excluding those with asymmetrical levels, there were no urological deaths in those born with a sensory level of L2 and below (p<0.001), and only one urological death in those with motor level of L2 and below (p=0.001). Of the 22 urological deaths, 10 (45%) had had evidence of outflow obstruction. Twelve deaths were due to renal failure, six to urinary sepsis, two to bladder cancer, and two were post-operative (after ureterostomy [n=1] and renal transplant [n=1]).
| Cause of death related to sensory levela | Sensory level L1 or above n (%) | Sensory level L2 or below n (%) | Asymmetrical sensory level n | Total |
|---|---|---|---|---|
| Neurological | 12 (21) | 10 (18) | 2 | 24 |
| Cardiorespiratory | 12 (21) | 14 (25) | 0 | 26 |
| Other | 5 (9) | 1 (2) | 0 | 6 |
| Urological | 21 (37) | 0 (0) | 1 | 22 |
| Alive at mean age 46 | 7 (12) | 30 (55) | 2 | 39 |
| Total | 57 | 55 | 5 | 117 |
| Cause of death related to motor levelb | No quadriceps activity (L1 or above) | Quadriceps activity both legs (L2 or below) | Asymmetrical: quadriceps activity in only one leg | |
|---|---|---|---|---|
| n (%) | n (%) | n | Total | |
| Neurological | 11 (18) | 11 (23) | 2 | 24 |
| Cardiorespiratory | 13 (22) | 13 (28) | 0 | 26 |
| Other | 4 (7) | 1 (2) | 1 | 6 |
| Urological | 20 (33) | 1 (2) | 1 | 22 |
| Alive at mean age 46 | 12 (20) | 21 (45) | 6 | 39 |
| Total | 60 | 47 | 10 | 117 |
- Bold value indicates there were no urological deaths in those with a sensory level of L1 and above.
- aSensory level is defined as the first dermatome of normal sensation above the area of anaesthesia, shown by a cry or grimace in response to pinprick.12 Those born with a sensory level of L1 and above have sensation only at and above the inguinal ligament. Fisher's exact test for cause of death in sensory level L1 or above versus L2 or below p<0.001 (excludes those with asymmetrical sensory level). bChildren with a motor level of L1 and above have no quadriceps activity and are likely to be immobile/wheelchair-bound with hydrocephalus, low IQ and incontinence of urine and faeces.5, 7, 19 Fisher's exact test for cause of death in motor level L1 or above versus L2 or below p<0.001 (excludes those with asymmetrical motor level).
Survival, urological-related deaths, and other deaths by sensory level
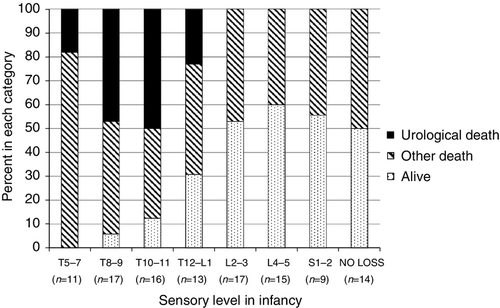
Figure 2 shows that the main reason survival was worse in those with a high sensory level was because of urological-related deaths.
Urological deaths and level of the lesion (cutaneous, radiological, motor, or sensory) in infancy
Table 2 shows that nearly all those dying of urological-related deaths had neurological levels above L1, but there was diversity in cutaneous and radiological levels.
| Case number | Cutaneous (external) levela | Radiological level (dysraphic vertebraeb) | Motor level | Sensory level |
|---|---|---|---|---|
| 1 | TL | T7–sacrum | Above L1 | T6 |
| 2 | TL | No data | Above L1 | T6 |
| 3 | TLS | T1–sacrum | Above L1 | T8 |
| 4 | TL | T6–8, T10–sacrum | Above L1 | T8 |
| 5 | TL | T1–sacrum | Above L1 | T8 |
| 6 | TLS | T12–sacrum | Above L1 | T9 |
| 7 | L | T11–sacrum | Above L1 | T9 |
| 8 | TL | T5–6, T11–sacrum | Above L1 | T9 |
| 9 | TL | T10–sacrum | Above L1 | T9 |
| 10 | LS | T4–12, L2–5 | Above L1 | T9 |
| 11 | TL | T10–sacrum | Above L1 | T9 |
| 12 | TLS | T10–L5 | Above L1 | T10 |
| 13 | L | T2–5 | Above L1, L4c | T10 |
| 14 | LS | L1–sacrum | Above L1 | T10 |
| 15 | L | L1–3 | Above L1 | T10 |
| 16 | TLS | T11–sacrum | Above L1 | T10 |
| 17 | L | T12–sacrum | L3 | T10 |
| 18 | LS | L1–sacrum | Above L1 | T11 |
| 19 | L | T2–7, L1–sacrum | Above L1 | L1 |
| 20 | TL | L2–sacrum | Above L1 | L1 |
| 21 | LS | L2–sacrum | Above L1 | L1 |
| 22 | L | T9–sacrum | Above L1 | T10, L4c |
- aCutaneous levels: TL, thoracolumbar; TLS, thoracolumbosacral, LS lumbosacral; L, lumbar. bDysraphic vertebra defined as interpedicular distance at least 2mm greater than normal.12 cAsymmetrical motor or sensory level. Case 13 died aged 3mo. Case 17 was subsequently found to have no quadriceps activity (i.e. motor level L1 or above) when reassessed at age 10y.
Discussion
Principal findings
Survival up to 50 years was related to neurological deficit in infancy, with few survivors among those most severely affected. The increased mortality in those born with a high neurological level (L1 or above) was mainly caused by urological deaths. Sensory and motor levels were more closely related to outcome than cutaneous or radiological levels.
Strengths and weaknesses
This is the first study to compare long-term outcomes in cases of open spina bifida born with a neurological level of L1 and above versus L2 and below. It is also unique in relating this cut-off with urological life expectancy. Other strengths are no loss to follow-up, this was an unselected cohort with meticulous assessment at birth and a wide range of disability, and the record length of follow-up by the same independent observer.12, 17 Risk of bias in measuring predictors and outcome should be low since assessment of neurological deficit in infancy was performed by experienced neurosurgeons, and details of deaths were provided by the Health and Social Care Information Centre.
The limitations are the small size of the cohort (although this is similar to other studies8), and that modern management has improved life expectancy. Findings may not accurately reflect the prognosis for individuals born later, or apply to non-white groups or different systems of medical care.2, 10
Comparison with other studies
This is the only spina bifida cohort with complete data. Loss to follow-up in other studies ranges from 20% to 45%.8, 10, 18 Series based on hospital clinic populations may miss the most severe cases who succumbed in infancy or the healthier cases who may no longer attend the clinic. They may also include cases of spina bifida occulta11 or skin-covered meningocele who tend to have lower rates of mortality and disability.10 Sudden deaths in the community,10 which occurred in 17 out of 38 (45%) of those who died after the age of 5 years, may be under-reported.
In line with a recent systematic review of urological outcome4 that recommended standardized reporting of level of the lesion, our results highlight the importance of neurological level rather than cutaneous or radiological level in predicting functional outcome. Although cutaneous thoracic lesions are more often associated with severe leg deficits than lower lesions, a few patients with cutaneous thoracic lesions have only mild functional deficits, and this discrepancy may be explained by the unexpected finding of a low sensory level. Our results also support previous suggestions5, 19 that a distinguishing feature between high and low lesions is the absence or presence of an active quadriceps in infancy. However, sensory level can usually be identified with greater precision than motor level.11
Renal failure is a leading cause of mortality and morbidity in people with spina bifida.4 Our results show this applies particularly to those with neurological level of L1 or above. By their mid- to late-40s, many of the cohort had undergone several procedures at various ages and in over 20 different hospitals to preserve renal function and/or continence. But this did not seem to influence the consistent relationship between neurological deficit and urological deaths. However, even though there were none in this cohort, urological-related deaths have been reported in those with a sacral sensory level.20
Implications
This study demonstrates the importance of neurological level at birth in predicting urological death or survival to middle age in open spina bifida. Accurate evaluation of sensory level10-12 requires experience. Motor level is difficult to measure above L1 and may be inaccurate immediately after breech delivery.12 In addition, apparent quadriceps extension when assessed at birth may be caused by reflex movement,12 as in case 17 (Table 2) who was subsequently found to have no quadriceps activity when assessed at the age of 10 years. Experts have recently recommended that sensory level be used for assessing the level of the lesion in accordance with the international standards for neurological and functional classification of spinal cord injury.11 Cutaneous and bony levels are generally easier to assess but much less clearly related to outcome.1 In our cohort, those who did best were born with a sensory level below L3 (i.e. sensation absent only below the knee). They were more likely than those with greater neurological deficit to survive to adulthood, to walk, be continent of urine, to have normal intelligence (IQ≥80), and to live independently in the community.16
It is likely that those with high and low sensory levels are biologically different in ways that influence urological mortality. It is also possible that management of complications was less aggressive in those with high lesions, many of whom were severely disabled. However, our data do not support this; for example, age at initiation of intermittent catheterization (where indicated) appeared similar between groups. Finally, non-adherence with medical/surgical management may be more common in those with intellectual disability or who lack support, and poor compliance may be associated with death caused by renal failure.
The novel finding that urological deaths reflect the extent of the neurological deficit in infancy has important clinical implications. Those with sensory levels of L1 and above lack normal bladder sensation and function, and are more likely than those with a lower sensory level to have a palpable, poorly emptying bladder and renal damage.20 They may be unaware of an overfull bladder, or may have detrusor-sphincter incoordination leading to renal damage because of back-pressure or even to bladder rupture.10 Clean intermittent catheterization should be started early,21 together with lifelong regular urological review.4 In our cohort, seven individuals with a neurological deficit of L1 and above are still alive and at risk of urological death. By contrast there were no urological deaths in those with perineal sensation to pinprick (S2–4), most of whom achieved urinary control.22
Neurologists, neurosurgeons, paediatricians, urologists, and orthopaedic surgeons should be aware that the extent of the neurological deficit at birth is the most reliable predictor of long-term outcome. Neurological level, particularly sensory level, should be included in the standardized assessment11 of all infants born with open spina bifida.
Acknowledgements
This study was funded by Newlife Foundation for Disabled Children. SG/11-12/06. We thank the patients and their carers; and Maria Harrington and Cathy Mackay. The Health and Social Care Information Centre/Office for National Statistics provided information on deaths. The authors have stated that they had no interests that could be perceived as posing a conflict or bias.