Adipocyte regulation of cancer stem cells
Abstract
Cancer stem cells (CSCs) are a highly tumorigenic subpopulation of the cancer cells within a tumor that drive tumor initiation, progression, and therapy resistance. In general, stem cell niche provides a specific microenvironment in which stem cells are present in an undifferentiated and self-renewable state. CSC niche is a specialized tumor microenvironment for CSCs which provides cues for their maintenance and propagation. However, molecular mechanisms for the CSC-niche interaction remain to be elucidated. We have revealed that adipsin (complement factor D) and its downstream effector hepatocyte growth factor are secreted from adipocytes and enhance the CSC properties in breast cancers in which tumor initiation and progression are constantly associated with the surrounding adipose tissue. Considering that obesity, characterized by excess adipose tissue, is associated with an increased risk of multiple cancers, it is reasonably speculated that adipocyte–CSC interaction is similarly involved in many types of cancers, such as pancreas, colorectal, and ovarian cancers. In this review, various molecular mechanisms by which adipocytes regulate CSCs, including secretion of adipokines, extracellular matrix production, biosynthesis of estrogen, metabolism, and exosome, are discussed. Uncovering the roles of adipocytes in the CSC niche will propose novel strategies to treat cancers, especially those whose progression is linked to obesity.
Abbreviations
-
- AdipoR
-
- adiponectin receptor
-
- ANGPTL4
-
- angiopoietin-like protein 4
-
- BAT
-
- brown adipose tissue
-
- BMI1
-
- B lymphoma Mo-MLV insertion region 1 homolog
-
- BMP8b
-
- bone morphogenetic protein 8b
-
- C3aR
-
- complement component 3a receptor
-
- CAA
-
- cancer-associated adipocyte
-
- CAP
-
- adenylyl cyclase-associated protein
-
- CCR
-
- C-C motif chemokine receptor
-
- CFD
-
- complement factor D
-
- CRC
-
- colorectal cancer
-
- CSC
-
- cancer stem cell
-
- DCN
-
- decorin
-
- ECM
-
- extracellular matrix
-
- EMT
-
- epithelial–mesenchymal transition
-
- ER
-
- estrogen receptor
-
- FA
-
- fatty acid
-
- FGF2
-
- fibroblast growth factor 2
-
- FOXC2
-
- forkhead box protein C2
-
- Gp
-
- glycoprotein
-
- HGF
-
- hepatocyte growth factor
-
- HSC
-
- hematopoietic stem cell
-
- IGF-1
-
- insulin-like growth factor-1
-
- IL
-
- interleukin
-
- JAK
-
- Janus kinase
-
- LEPR
-
- leptin receptor
-
- LIF
-
- leukemia inhibitory factor
-
- LSC
-
- leukemic stem cell
-
- MAPK
-
- mitogen-activated protein kinase
-
- MCP-1
-
- monocyte chemotactic protein 1
-
- MMP
-
- matrix metalloproteinase
-
- NF-κB
-
- nuclear factor of kappa-light-chain gene enhancer in B cells
-
- NOTCH2
-
- neurogenic locus notch homolog protein 2
-
- NRG4
-
- Neuregulin 4
-
- OSMR
-
- oncostatin M receptor
-
- PPAR
-
- peroxisome proliferator-activated receptor
-
- ROR
-
- receptor tyrosine kinase-like orphan receptor
-
- ROS
-
- reactive oxygen species
-
- SAT
-
- subcutaneous adipose tissue
-
- SOX
-
- SRY (sex-determining region Y)-box transcription factor
-
- Sp
-
- specificity protein transcription factor
-
- STAT
-
- signal transducer and activator of transcription
-
- T2D
-
- type-2 diabetes
-
- TLR
-
- toll-like receptor
-
- TME
-
- tumor microenvironment
-
- UCP1
-
- uncoupling protein 1
-
- VAT
-
- visceral adipose tissue
-
- VEGF
-
- vascular endothelial growth factor
-
- WAT
-
- white adipose tissue
1 INTRODUCTION
Interactions between tumor cells and the associated stroma, called tumor microenvironment (TME), represent a powerful relationship that influences disease initiation, progression, and patient prognosis. Adipocytes are a component of TME which is composed of a variety of cells, including fibroblasts, infiltrating inflammatory cells, vascular endothelial cells, lymphatic cells, and neural cells,1 and those that promote tumor proliferation, invasion, and immune suppression are called cancer-associated adipocytes (CAAs).2 In the phenomena called adipocyte–mesenchymal transition (AMT), tumor cells induce the dedifferentiation of adipocytes into multiple cell types, including myofibroblast- and macrophage-like cells.3 These AMT cells become involved in various biological processes, such as immune response, inflammation, and extracellular matrix (ECM) remodeling and regulate tumor progression. AMT is at least partly induced by tumor-derived soluble factors, such as TNF-α, plasminogen activator inhibitor 1, Wnt3a, IL-6, IL-1β, and TGF-β, and exosomal microRNAs.
Adipose tissue is not simply the primary site for energy storage but functions as an active endocrine organ in which adipocytes secrete cytokines and hormones called adipokines. Adipokines play numerous roles in tumor formation and progression via modulating oncogenic signaling, metabolism, angiogenesis, and immune microenvironment.4-6 Furthermore, lipids such as fatty acids (FAs) and FA derivatives, including phospholipids, sterols, and sphingolipids, secreted from adipocytes modulate processes ranging from the ECM remodeling to cancer cell signaling.7 Many cancers, such as colorectal, breast, prostate, lung, ovarian cancers, and hematologic malignancies, obtain FA from surrounding adipose tissue by stimulating lipolysis in adipocytes to promote energy metabolism (β-oxidation), membrane synthesis, and biosynthesis of lipid-derived cell-signaling molecules.8 Hypoxia in the adipose tissue of obese patients is caused by insufficient blood perfusion owing to a relatively low density of microvessels, which triggers angiogenesis, inhibits macrophage migration and preadipocyte differentiation, augments fibrosis, and suppresses recruitment of immune cells, all of which confer drug resistance abilities to cancer cells.9
Cancer stem cells (CSCs) are a highly tumorigenic subpopulation of cancer cells within a tumor and have a higher ability to promote tumor initiation10, 11 and metastatic progression, especially at the initial steps of metastases.12 Therefore, CSCs are considered to be a critical target to ensure the complete elimination of tumor cells. Cell surface markers such as CD34, CD133, CD44, CD166, and CD24 and ALDH1 activity among others, have been operationally used to identify CSC populations.10 The purified CSC population is still heterogenous and some types of CSCs, like those of colorectal cancers (CRCs), exhibit high plasticity, allowing them to dynamically switch phenotype, such as stem/non-stem cell, epithelial–mesenchymal transition (EMT), and quiescent/proliferative condition, depending on stem cell niche and metabolic pathways of glycolysis and oxidative phosphorylation.13 Stem cells have a long-term self-renewal ability, a specific cellular action that involves proliferation accompanied by maintenance of both multipotency and tissue regenerative potential; and frequency and timing of actual stem cell self-renewal divisions are tightly regulated within the tissue to ensure the lifelong maintenance of the stem cell population. CSCs share several properties with normal stem cells from which they are derived, such as self-renewal ability and the ability to generate differentiated progenies. Epigenetic mechanisms, such as Polycomb gene complexes, histone modifications, microRNAs, and other noncoding RNAs, play important roles in the regulation of self-renewal and differentiation of both normal and malignant stem cells. We have revealed that targeting Polycomb group gene BMI1 by microRNA (miR)-200c is a shared molecular mechanism for stem cell regulation in both tissue stem cells and CSCs in breast and colon epithelium.14, 15
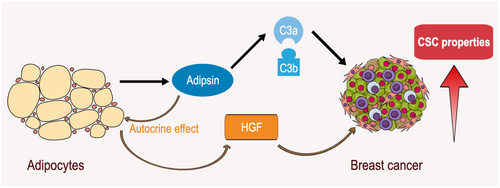
The CSC niche maintains the properties of CSCs and facilitates their metastatic potential.16 We have proposed that mammary adipocytes function as a CSC niche in breast cancers and secrete adipsin (complement factor D, CFD) and its downstream effector HGF, resulting in the enhancement of CSC properties of breast cancer cells17, 18 (Figure 1). Understanding the essential roles of CSC niche in tumor initiation and progression will uncover novel strategies to treat cancers, especially those whose progression is linked to obesity.
2 CLASSIFICATION OF ADIPOSE TISSUES
Adipose tissue is classified into two main types: white adipose tissue (WAT) and brown adipose tissue (BAT), and WAT is further subdivided into subcutaneous adipose tissue (SAT) and visceral adipose tissues (VAT). A third and fourth types of adipocytes, beige and pink adipocytes, are generated by the transdifferentiation of SAT.
White adipose tissue, the most common type of adipose tissue in the body, is responsible for energy storage in the form of triglycerides, as well as adipokine secretion, hormone biosynthesis, insulation, mechanical protection of organs, and inflammation.19 WAT can be further subdivided into SAT and VAT. SAT is located just under the skin and throughout the body. It serves as an energy reserve and also provides insulation. VAT is found in the abdomen and around the internal organs. VAT is more metabolically active, contains more immune cells than SAT, and is associated with a higher risk of metabolic diseases like type-2 diabetes (T2D) and cardiovascular disease.
Brown adipose tissue is a specialized type of adipose tissue that generates heat to maintain body temperature. Thermoregulation by BAT utilizes uncoupling protein 1 (UCP1) that uncouples mitochondrial respiration from ATP synthesis. It is mainly found in infants and hibernating animals, but it also exists in small amounts in adults. Being rich in mitochondria, BAT is brownish in color and more metabolically active than WAT. BAT secretes a collection of active peptides called batokine, including FGF2, BMP8b, NRG4, IL-6, and IGF-1.20
Beige adipocytes are interspersed within the WAT and can be induced by “browning” of WAT. Activated beige adipocytes are characterized by high levels of FA β-oxidation, mitochondrial content, and thermogenesis.21
Pink adipocytes are found in lactating mammary adipose tissue and are named after their distinctive pink appearance when stained with hematoxylin and eosin. During lactation, the mammary gland undergoes extensive remodeling, including an increase in adipose tissue to support milk production. Pink adipocytes are thought to play a role in providing energy substrates to support milk production, and emerging evidence suggests that they derive from the transdifferentiation of subcutaneous white adipocytes.22
White adipose tissue and its association with various diseases, including cardiovascular disease, T2D, metabolic syndrome, and cancers, have been extensively studied. In contrast, the roles of BAT, beige and pink adipocytes in cancers are not fully elucidated. Activation of thermogenic metabolism in BAT facilitates tumor suppression by enhancing blood glucose uptake in adipocytes and impeding the glycolysis-based metabolism in cancer cells, which are alleviated by the removal of BAT or genetic deletion of UCP1.23
3 ADIPOCYTES AND CSCs
The relationship between adipocytes and CSCs is complex, and the precise effects of adipocytes on CSCs can vary depending on the type of cancer and the particular context.
3.1 Breast cancer
The mammary microenvironment is primarily composed of adipocytes which are implicated in breast tumor growth and stemness maintenance.17 Adipocytes accelerate mammosphere formation, the expression of stem-like markers Sox2, c-Myc, and Nanog, tumor formation, and metastasis.24
Obesity is one of the risk factors for breast cancer development and progression, with a 35% to 40% increase in cancer mortality in obese patients.25 The expression of CSC-associated genes, such as Sox2, Notch2, Foxc2, and Twist2, is increased in the tumors of obese mice, whereas leptin expression is elevated in the surrounding obese mammary fat pads.26
3.2 Colorectal cancer
Colorectal cancer is located in an adipose tissue-rich environment, and obesity is a risk factor for this malignancy, suggesting the underlying link between CRC and adipocytes. Coculture of CRC cells with adipocytes promotes organoid formation,27 increases the expression of Wnt target CSC genes Lgr5 and Cd44, and decreases the markers for epithelial cell differentiation, such as sucrase-isomaltase (Sis) and mucin 2 (Muc2).27 Tumors neighboring visceral adipose stromal cells secrete IL-6 and HGF and expand the metastatic colorectal CSC compartment (CD44v6+); CSCs, in turn, recruit adipocytes through secreting neurotrophins, including NGF and NT-3.28
3.3 Pancreas cancer
While SAT and VAT appear to be indirectly associated with pancreas cancers, intrapancreatic fat deposition is observed in individuals with diabetes, pancreatitis, and pancreatic cancer.29 These adipocytes may derive from pancreatic stromal mesenchymal stem cells that can differentiate into adipocytes. It has been reported that stem or progenitor cells in the adipose tissue can migrate to the tumor stroma, thereby promoting cancer progression.30
3.4 Leukemia
Adipocytes in the bone marrow, derived from the same mesenchymal stem cells as osteoblasts, are classically considered negative regulators of normal hematopoiesis. However, they also support active red bone marrow regeneration and myeloid-erythroid maturation. Recent research has demonstrated that adipose tissue serves as an extramedullary reservoir of hematopoietic stem cells (HSCs), indicating the presence of an HSC niche in the adipose tissue.31
In a mouse model of the blast crisis phase of chronic myeloid leukemia, adipose tissue in the bone marrow or gonadal region functions as a reservoir of LSCs, especially those expressing the FA transporter CD36+.32 The lipolysis of triglycerides to FA is induced by leukemic cells to promote their proliferation and survival.33 Furthermore, adipocytes secrete cytokines that inhibit T-cell function and alter the immune response to leukemia, which may influence the behavior of leukemic stem cells (LSCs).34
3.5 Ovarian cancer
The omentum is a visceral WAT depot and one of the most common sites of ovarian cancer metastasis, with 80% of all serous ovarian carcinomas metastasizing to the omentum.35 Omental adipocytes secrete IL-6, IL-8, TIMP1, and MCP1 and promote early metastatic seeding to the omentum. Ovarian cancer cells, in turn, activate Wnt/β-catenin signaling and induce dedifferentiation of omental adipocytes into CD73, CD90, CD105, and alpha-smooth muscle actin (α-SMA) expressing mesenchymal stem cell and myofibroblast-like fibroblasts which promote ovarian cancer cell proliferation and migration.36 IL-6 cytokine secreted from adipocytes inhibits mitochondria-initiated apoptosis in chemoresistant ovarian CSCs, including CD44+/MyD88+ cancer cell population.37
3.6 Prostate cancer
Obesity has been widely associated with a more aggressive tumor and poorer therapeutic outcomes in prostate cancer.38 Adipocyte-conditioned media exert a significant protumor effect on prostate cancer cells and promote tumor sphere formation and CD133 and CD44 upregulation.39
3.7 Endometrial cancer
Due to limited treatment options, advanced endometrial cancer continues to have a poor prognosis, which may be worsened by obesity. Treatment with metformin decreases the ratio and activity of both ALDHhigh and CD133+ve endometrial CSC populations without affecting the viability of the cells. However, exposure to patient-derived adipocyte-conditioned media inhibits this impact.40
4 MOLECULAR MECHANISMS OF CSC REGULATION BY ADIPOCYTES
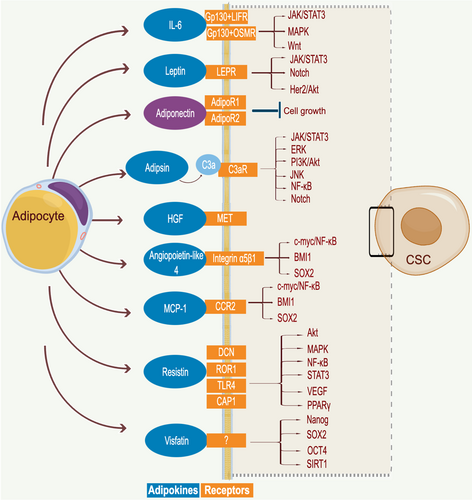
Adipocytes regulate the stem cell properties in the tissues, such as mammary tissue and bone marrow. However, the molecular mechanism for the stem cell and CSC niche function of adipocytes is not clearly demonstrated (Figure 2).

4.1 Adipokine
Adipokines released from the adipocytes contain more than 600 bioactive molecules that act in paracrine and endocrine manners and function as mediators of adipocyte–cancer cell interactions. Some of these adipokines are exclusively released from adipocytes, whereas the others are secreted from other tissues as well. Adipokine secretion is induced by various stimuli, including metabolic status, adipokines, inflammation, mechanical stress, and exosomes, which are derived from cancer cells, CSCs, adipocytes themselves, and surrounding microenvironments.41, 42 In addition, the differentiation status of adipocytes, for example, long-term adipogenic differentiation (LTAD), is the factor that regulates the secretion level of multiple adipokines from adipocytes.43
Under normal physiological conditions, these adipokines perform valuable functions to maintain homeostasis. However, the dysregulation of adipokine secretion in CAA promotes CSC properties and the growth and spread of cancer cells (Figure 3).
4.1.1 Interleukin (IL)-6
Interleukin-6 is a glycosylated, 22–27-kDa secreted glycoprotein with pleiotropic effects on inflammation, immune response, and hematopoiesis and is produced in response to environmental stressors such as infections and tissue injuries.44 IL-6 activates the Janus kinase (JAK)/STAT and mitogen-activated protein kinase (MAPK) cascades via the signal transducer glycoprotein-130 (gp-130), LIF receptor, and oncostatin M (OSM) receptor.
Interleukin-6 functions as a stimulator of various types of CSCs, such as colorectal, breast, and ovarian cancers, and activates CSC properties through its induction of OCT4, ZEB2, NANOG, and FRA1, a member of the FOS family of transcription factors through the JAK/STAT3 pathway,28 and the stemness and metastasis-related genes, such as WNT5A, WNT5B, WNT7A, matrix metalloproteinase 2 (MMP-2), MMP-9, TWIST, NODAL, SDF1, and ZEB2.28 Multiple copies in T-cell Malignancy 1 (MCT-1/MCTS1) and Syndecan-1 are upstream regulators of IL-6 secretion in cancer cells.5, 45
In breast cancer, IL-6 secreted from adipocytes enhances mammosphere formation and CSC marker expression by activating Src. Activated Src, in turn, upregulates Sox2, and Sox2-dependent miR-302b induction increases CSC-like properties.24 The combination of anti-IL-6 antibody and cisplatin destroys the lung cancer organoids, while cisplatin alone is not.46
4.1.2 Leptin
Leptin and adiponectin are among the first adipokines discovered in the 1990s. Leptin, derived from the Greek word leptos, meaning thin, is a multifunctional neuroendocrine peptide hormone secreted from fat cells in WAT in response to the overall amount of energy stored and acute changes in energy intake. Leptin, 16 kDa in size and comprising 167 amino acids (including a 21-amino-acid secretory signal sequence), is originally identified as the product of the obese (ob) gene of the genetically obese (ob/ob) mice47 and generally functions in appetite suppression, energy reserve, metabolism, immune response, and reproductive processes.
Leptin acts through six isoforms of transmembrane receptors called LEPRs (LEPRa through LEPRf), which are widely distributed throughout the body. LEPRs differ in the length of their intracellular domain and are structurally similar to the class I family of cytokine receptors.
Hijacking leptin and LEPR signaling is involved in the benign-to-malignant transition and functions as an inducer of cancer stemness. Leptin-induced JAK/STAT3 regulates lipid metabolism and promotes breast CSCs.48 Tumor growth, self-renewal, and cell proliferation are significantly reduced in LEPR-silenced cells in vivo.49 The expression of the CSC transcription factors CD44, NANOG, SOX2, and OCT4 is reduced as a result of LEPR silencing.49, 50 Mammary adipocyte-derived leptin upregulates STAT3-induced carnitine palmitoyltransferase 1B (CPT1B) expression and FA β-oxidation activity in breast CSCs.50
4.1.3 Adiponectin
Adiponectin is produced almost exclusively by adipocytes in WAT and at lower concentrations in BAT. Its plasma concentration is inversely correlated with body mass index (BMI) and is inversely linked to the risk of obesity-associated malignancies and insulin resistance. Adiponectin has opposing biological functions to leptin and exerts antineoplastic effects. Lower plasma adiponectin levels are associated with the risk for various cancers, such as colorectal, breast, and endometrial cancers.51 Sphere formation ability is stimulated by leptin and is suppressed by adiponectin.52
4.1.4 Adipsin
Adipsin (CFD) is predominantly secreted in significant amounts from adipocytes and is induced during adipogenesis by PPARγ, the master regulator of adipocyte biology. Adipsin is a serine protease that is indispensable for the activation of the alternative pathway of the complement system in which it cleaves complement factor B into Ba and Bb, and then a C3 convertase composed of Bb and complement component 3b (C3b) cleaves C3 into C3a and C3b. It has been reported that the adipsin/C3a pathway plays multiple roles, such as immune regulation, cell migration, insulin tolerance, adipocyte differentiation, and homing of HSCs.53-55
We have reported that adipsin is an adipokine secreted from the adipocyte-derived stem cells isolated from the human mammary adipose tissue. Adipsin and its downstream effector HGF enhance the proliferation and CSC properties of breast cancer cells and patient-derived xenograft cells through the activation of alternative complement pathway17 (Figure 1).
4.1.5 Angiopoietin-like 4
Angiopoietin-like protein 4 (ANGPTL4) is a key regulator of lipoprotein lipase, which prevents their dimerization and subsequent activation. Modulation of ANGPTL4 has a significant impact on the body's processing and distribution of triglycerides and cholesterol.
Angiopoietin-like protein 4 secreted by adipocytes plays a vital role in the therapeutic resistance of cancers. The glycosylated ANGPTL4 protein binds to integrin α5β1 on the surface of ovarian cancer cells, thereby activating the c-myc/NF-kB pathway.56 The overexpression of ANGPTL4 induces the enrichment of glioma stem-like cells characterized by Polycomb complex protein BMI1 and SOX2 expression and results in temozolomide resistance in glioblastoma.57
4.1.6 Monocyte chemoattractant protein-1
Monocyte chemoattractant protein-1 (MCP-1, CCL2), the first discovered human CC chemokine located on chromosome 17 (chr.17, q11.2), is a monomeric polypeptide produced by various cell types, including human adipocytes, macrophages, and endothelial cells; and functions as a potent chemotactic factor for monocytes, memory T lymphocytes, and natural killer (NK) cells. In addition, the abundance of MCP-1 in both WAT and plasma is increased in obese mice.58
MCP-1 protein induces Notch1 expression and enhances the CSC signaling that stimulates the sphere-forming phenotype in breast cancer cells.59 In vitro coculture of adipocytes and breast cancer cells upregulates MCP-1 secretion from adipocytes, which in turn induces mammosphere formation and expression of CSC markers SOX2, c-MYC, and NANOG in breast cancer cells.24
4.1.7 Visfatin
Visfatin, also referred to as nicotinamide phosphoribosyl transferase (NAMPT), is a 52-kDa enzyme that is involved in NAD+ biosynthesis.60 The intracellular visfatin expression in cancer cells increases cell proliferation through PI3K/AKT and ERK/MAPK activation. The extracellular visfatin is secreted from several tissues with a higher secretion from adipose tissue, especially from fully differentiated WAT and BAT.
Adipokine visfatin increases stemness and angiogenesis in breast cancer. Visfatin enhances tumor sphere formation and protein expression levels of the stem cell genes NANOG, SOX2, OCT4, and Sirtuin 1 (SIRT1), which is diminished by the visfatin inhibitor FK866.61
4.1.8 Resistin
Resistin is a cysteine-rich hormone that is secreted by human peripheral blood mononuclear cells (PBMC) and macrophages and by rodent WAT and BAT. Human resistin is a peptide with a mature sequence consisting of 108 amino acids, whereas rodent resistin has 114 amino acids. The isoforms of decorin (DCN), mouse receptor tyrosine kinase-like orphan receptor 1 (ROR1), toll-like receptor 4 (TLR4), or adenylyl cyclase-associated protein 1 (CAP1) are proposed to be the resistin receptors.
Resistin has been linked to an increased risk of tumor progression in various cancer models. It is also associated with chemoresistance and stemness induction in cancer.62 For example, resistin promotes EMT and stemness in breast and ovarian cancer cells.63 It is, however, still insufficient to conclusively link the impact of resistin on the initiation and development of cancers.
4.2 Extracellular matrix
The ECM is a major structural component of the TME, and ECM proteins establish a physical and biochemical niche for CSCs.64 Adipocytes promote the synthesis of matrix proteins, such as collagen VI, and activate matrix-related enzymes, such as MMP-2 and -9, thereby inducing breast cancer tumorigenesis.65 In triple-negative breast cancer, tumor-associated adipocytes upregulate fibronectin expression and stiffness through the secreted TGF-β. However, the roles of adipocyte-mediated ECM remodeling in the regulation of CSCs remain to be elucidated.
4.3 Biosynthesis of estrogen
Estrogen is a sex steroid hormone that plays a role in both male and female reproductive systems. Estrone (E1), estradiol (E2), estriol (E3), and estetrol (E4) are four estrogens that are spatially and temporally present during different female reproductive phases, with E2 being the most abundant and extensively studied. Estrogens are synthesized from androgens using cytochrome P450 aromatase, which is encoded by the CYP19 gene.66 After menopause, estrogen biosynthesis is primarily mediated by peripheral aromatization of androgen precursors in adipose tissue.67
Although exposure to estradiol promotes the growth and maintenance of papillary thyroid CSCs68 and the importance of estrogen in breast cancer is well established, the effects of estrogen on breast CSCs are not fully understood. Several studies have reported that estrogens alone do not increase, and breast CSCs lack expression of estrogen receptor (ER) or express it at very low levels.69 Breast CSCs expand through the indirect effects of estrogen. Inflammatory cytokine production in human mammary adipocytes increases with obesity after menopause, and in proximity to cancers. Interaction of these more inflammatory adipocytes with cancer cells stimulates E1- and NF-κB-dependent cytokine induction and expansion of CSC cells.
4.4 Metabolism
Adipocytes release metabolites, such as FA and glutamine, which are transferred to cancer cells and modulate cellular metabolism and the CSC properties of cancer cells.
4.4.1 FA release
FA released by adipocytes into the TME promotes cancer cell survival under energy-stress conditions by upregulating autophagy and mitochondrial FA oxidation (FAO) via AMPK activation.27 Coculture of human adipocytes and breast cancer cells increases the expression of CD36, an FA transporter protein, in breast cancer cells, the ablation of which reduces adipocyte-induced EMT and stemness.70 CD36 activates STAT3 signaling, and STAT3 binds to the CD36 promoter to upregulate its expression. CD36 expression results in a shift toward FAO as a result of metabolic reprogramming. CPT1A, a key enzyme controlling FAO, is upregulated in CRC cells upon exposure to adipocytes or FAs and promotes the acetylation and nuclear translocation of β-catenin. Genetic ablation of CPT1A reduces the protective effect provided by FAs against nutrient deprivation, tumor organoid formation, and the expression of CSC genes downstream of Wnt/β-catenin signaling.71
4.4.2 Glutamine
Glutamine promotes glutathione (GSH) synthesis and consequently regulates redox homeostasis, which is the basis for the maintenance of stem cell properties and therapeutic resistance. Adipose tissue secretes significant amounts of glutamine into the interstitial fluid.72 Therefore, CAA in the TME indirectly influences CSC fate by modulating glutamine availability. In head and neck squamous cell carcinoma (HNSCC), CD44 variant (CD44v)-positive CSCs survive only with the cystine-glutamate antiporter xCT activity. Sulfasalazine inhibits xCT and GSH synthesis in CSCs, causing reactive oxygen species (ROS)-mediated cell death without affecting CD44v-negative, differentiated cells in the same tumor.73, 74
4.5 Exosome
Exosomes (30–100 nm) are derived from the luminal vesicles of the multivesicular body and contain functional biomolecules, such as proteins, lipids, RNA, and DNA. They are secreted by cell membrane fusion events controlled mainly by Rab family proteins, specifically Rab27a and Rab27b. Tumor-secreted exosomes with particular exosomal integrins direct organ-specific colonization by fusing with target cells in a tissue-specific fashion, thereby initiating premetastatic niche formation.75
Exosomes and extracellular vesicles (EVs) derived from adipocytes promote the stemness and aggressiveness of breast cancer cells. Thrombospondin family protein TSP5, which is more abundant in exosomes from adipocytes, contributes partially to EMT and potentially to cancer stemness in recipient cells.76 Exosomes secreted from mesenchymal stromal/stem cell-derived adipocytes (AD-MSCs) promote breast cancer cell growth by activating the Hippo signaling pathway, which is implicated in CSC regulation; and upregulates genes, including CTGF, ANKRD1, and CYR61.77 EVs derived from adipocytes significantly enhance the ability of breast cancer cells to form mammospheres and increase the percentage of CD44+/CD24− breast CSCs and the expression levels of stemness markers CD44, OCT4, and BMI1 mRNA in breast cancer cells.78
5 CONCLUSION
The incidence of obesity is rising, and greater than 40% of the world's population is expected to be overweight or suffer from obesity by 2030. Obesity increases mortality from cancers, such as prostate and stomach in men, breast (postmenopausal), cervix, and uterus in women, and kidney (renal cell), colon, esophagus (adenocarcinoma), pancreas, gallbladder, and liver in both sexes,5 posing obesity-related cancer as one of the leading causes of death.7, 79
In this review, we discussed the molecular mechanisms of CSC regulation by adipocytes. Although adipocyte–cancer cell interactions have been extensively studied, the number of studies elucidating adipocyte–CSC interactions is still limited (Table 1). Indeed, most of the findings depend on tumor sphere assays of cancer cells, demonstrating the necessity for further studies to confirm these findings in in vivo experimental settings and using patient-derived tumor xenograft models.
| Adipokine | Cancer type | Experimental findings (CSC-related) | References |
|---|---|---|---|
| IL-6 | Breast | TS ↑, ES genes ↑, CD44 ↑ | [5] |
| TS ↑, CD44 ↑, ALDH1 ↑ | [45] | ||
| TS ↑, ES genes ↑, miR-302 ↑ | [24] | ||
| Ovary | TS ↑, ES genes ↑, ALDH1 ↑ | [6] | |
| Colorectal | TS ↑, ZEB2 ↑, TG ↑ | [28] | |
| Lung | Organoid ↑ | [46] | |
| Leptin | Breast | TS ↑, ES genes ↑, TG ↑ | [49] |
| TS ↑, ES genes ↑(TNBC cell lines and patient tumor), TG ↑, ALDH1 ↑(murine tumor) | [50] | ||
| TS ↑, CD44 ↑(patient tumor) | [48] | ||
| Adiponectin | Breast | TS ↓ | [52] |
| Adipsin | Breast | TS ↑, CD44 ↑, TG ↑ | [17] |
| TS ↑ | [18] | ||
| Angiopoietin-like 4 | Glioblastoma | TS ↑, ES genes ↑, BMI1 ↑, ANGPTL4 ↑ (patient tumor) | [57] |
| MCP-1 | Breast | TS ↑, Notch-1 ↑(BC cell lines and patient tumor), TG ↑ | [59] |
| TS ↑, ES genes ↑ | [24] | ||
| Visfatin | Breast | TS ↑, ES genes ↑ | [61] |
| Resistin | Breast | TS ↑, ES genes ↑ | [62] |
| Ovary | TS ↑, ES genes ↑ | [63] |
- Abbreviations: ALDH, aldehyde dehydrogenase; BC, breast cancer; CSC, cancer stem cell; ES, embryonic stem cell; TNBC, triple-negative breast cancer; TG, tumorigenicity; TS, tumor sphere formation; ZEB, zinc finger E-box-binding homeobox.
Direct contact of stem cells with their niche is at least partly mediated by cell adhesion molecules, such as VCAM1/VLA4 and JAG1/NOTCH, in the hematopoietic system.80 Similarly, it is reasonably speculated that sets of adhesion molecules will mediate the direct contact of CSCs with adipocytes inside the niche to promote CSC properties. Finally, it is reasonable to speculate that modulation of adipokine secretome and other mechanisms during LTAD will modify the ability of adipocytes to interact with CSCs. Further studies will uncover the unique roles of adipocytes as a CSC niche and the ways to overcome obesity-related cancers.
ACKNOWLEDGMENTS
We thank present and previous colleagues and collaborators for their great contributions and excellent achievements. Mind the Graph platform (www.mindthegraph.com) was used to depict the graphics in the figures under the CC BY-SA license (https://creativecommons.org/licenses/by-sa/4.0/deed.en).
FUNDING INFORMATION
This work was supported by (1) grants-in-aid from the Japan Society for the Promotion of Science (JSPS KAKENHI) (18K07231 and 21H02769 to Y.S.; 22K15532 to B.K.); (2) the Princess Takamatsu Cancer Research Fund (to Y.S.); (3) the Fujita Health University (to B.K. and Y.S.); (4) an extramural collaborative research grant of the Cancer Research Institute, Kanazawa University (to Y.S.); (5) the Promotion and Mutual Aid Corporation for Private Schools of Japan (to Y.S.); and (6)Memorial Fund of the General Meeting of the Japanese Association of Medical Sciences (to Y.S.). The funders had no role in study design, data collection, analysis, decision to publish, or preparation of the manuscript.
CONFLICT OF INTEREST STATEMENT
Yohei Shimono is a coinventor on a patent application owned by Stanford University (US-20110021607) describing the use of miRNAs as biomarkers for the identification and therapeutic targeting of CSCs and on a patent and a patent application owned by Fujita Health University (6664685 and 137508) describing the use of adipsin inhibitors and statins for therapeutic targeting of CSCs. Yohei Shimono holds a financial relationship with a pharmaceutical company that might be considered relevant to this study: Quanticel Pharmaceuticals, now a fully-owned subsidiary of Celgene and Bristol Myers Squibb (patent royalties). L.T. and B.K. have no conflict of interest.
ETHICS STATEMENT
- Approval of the research protocol by an Institutional Reviewer Board: Human primary cancers were obtained from patients admitted to the Division of Breast and Endocrine Surgery and the Division of Surgery of Kobe University Hospital and the Department of Breast Surgery of Fujita Health University Hospital. The research was preapproved by Kobe University's Institutional Review Board (permission number: 1299 and 1481) and Fujita Health University's Institutional Review Board (permission number: HM22-323) and was conducted in accordance with recognized ethical guidelines.
- Informed Consent: All patients included in the study provided written informed consent.
- Registry and the Registration No. of the study/trial: N/A.
- Animal Studies: Animal experiments were performed with the approval of Kobe University's Animal Care and Use Committee (permission number: P100905 and P150802) and Fujita Health University's Animal Care and Use Committee (permission number: AP19062 and AP19146) and carried out according to the Animal Experiment Regulations of Kobe University and Fujita Health University.
DISCLOSURE
Yohei Shimono is a current Editorial Board member of Cancer Science.




