Radar localization of breast and axillary lesions with SCOUT: a prospective single institution pilot study
Abstract
Background
Wire-guided localization has been the mainstay of localization techniques for non-palpable breast and axillary lesions prior to excision. Evidence is still growing for relatively newer localization technologies. This study evaluated the efficacy of the wireless localization technology, SCOUT®, for both breast and axillary surgery.
Methods
Data were extracted from a prospective database (2021–2023) of consecutive patients undergoing wide local excision, excisional biopsy, targeted axillary dissection, or axillary lymph node dissection with SCOUT at a high-volume tertiary centre. Rates of successful reflector placement, intraoperative lesion localization, and reflector retrieval were evaluated. A survey of surgeon-reported ease of lesion localization and reflector retrieval was also evaluated. Clinical trial registration: ACTRN386751.
Results
One-hundred-ninety-five reflectors were deployed in 172 patients. Median interval between deployment and surgery was 3 days (range 1–20) and mean distance from reflector to lesion was 3.2 mm (standard deviation, SD 3.1). Rate of successful localization and reflector retrieval was 100% for both breast and axillary procedures. Mean operating time was 65.8 min (SD 33). None of the reflectors migrated. No reflector deployment or localization-related complications occurred. Ninety-eight percent of surgeons were satisfied with ease of localization for the first half of cases.
Conclusion
SCOUT is an accurate and reliable method to localize and excise both breast and axillary lesions, and it may overcome some of the limitations of wire-guided localization.
Introduction
Breast cancer is the most common cancer among Australian women.1 Early identification of early and non-palpable breast cancer through population-based screening has helped improve outcomes.2-4 Many patients with non-palpable breast lesions may be candidates for wide local excision (WLE), which offers disease-free survival rates similar to mastectomy and results in higher quality of life partly due to cosmetic preservation of tissue.5, 6
The practice of axillary lymph node dissection (ALND) in clinically node positive disease has been challenged with the advent of more effective neoadjuvant chemotherapy (NAC), allowing for de-escalation of surgery in cases with a good response.7, 8 Targeted axillary dissection (TAD) involving ‘clipping’ of the involved node at time of initial diagnosis, with subsequent localization using a hook wire or radioactive seeds has also been shown to reduce false negative rates.9
Wire-guided localization (WL) has facilitated the surgical excision of non-palpable breast and axillary lesions since first described by Frank and Hall in 1976.10 The advantages of WL are that it is an effective, well-established, and economical technique.11 There are, however, procedural related disadvantages, which include discrepancy between wire entry site and ideal surgical approach, wire migration and transection, which could result in inaccuracy with excision of target tissue, potential for excessive tissue removal, and inadequate margins.12, 13 Workflow related disadvantages include that the wire must be placed the day prior or day of surgery to reduce risk of wire migration. This directly couples radiology and theatre schedules with the risk of costly delays to surgery.14
The challenges associated with WL have led to the development of alternatives, such as radioactive and magnetic seeds, radiofrequency identification tags, and radar reflectors.4, 15-19 SCOUT® (Merit Medical Systems, Inc. South Jordan, Utah, USA) is a non-radioactive, wireless localization technology that has several potential advantages such as lower susceptibility of displacement, increased comfort, and convenience of placement over 30 days prior to surgery.19 While promising clinical data has emerged since initial approval from the Food and Drug Administration in 2014, and recently being listed as a service subsidized by the Australian Government in the Medicare Benefits Schedule (MBS), there is ongoing need for further data to elucidate its efficacy to assist with potential adoption of this device. This study evaluated the rates of successful reflector placement, intraoperative lesion localization, and reflector retrieval of SCOUT for both breast and axillary surgery.
Methods
Study design and patient population
Data were extracted from a prospective database from a high-volume tertiary institution in Australia (February 2021 to August 2023). Patients undergoing either breast and/ or axillary surgery were eligible for inclusion in this study if they were females at least 18 years of age with non-palpable breast lesion(s) that required excision. Patients were excluded if they met any of the following criteria: (1) had advanced (Stage IV) malignancy; (2) were pregnant or lactating; (3) required stereotactic localization with WL (a small number of patients had dual localization with wire and SCOUT prior to this study); (4) had a known allergy to components of SCOUT (e.g., nickel) (Table S1). All patients with malignant disease were discussed at a breast cancer multidisciplinary team meeting that included surgeons, radiologists, radiation oncologists, medical oncologists, cancer geneticists, and breast care nurses. An earlier study of this data focused on the cost-effectiveness of WL compared to SCOUT for WLE of non-palpable breast lesions, both of which are too substantial to be reported in one study.20
This study was approved by the Human Research Ethics Committees (HREC) Sydney Local Health District, Australia (X23-0162/ETH00854/PID00966). It was registered on the Australian New Zealand Clinical Trials Registry (ANZCTR: ACTRN386751).
Study outcomes and procedure
Demographic information included age, ASA (American Society of Anesthesiologists) Classification status, and body mass index (BMI). Operative duration, length of hospital stay, and postoperative complications up to 30 days postoperative were documented. Primary outcomes were rates of successful reflector placement, intraoperative lesion localization, and reflector retrieval of SCOUT for both breast and axillary surgery. Time from reflector placement to surgery, distance from reflector to lesion, specimen weight, specimen volume, operative time, rate of margin positivity, re-excision rate, and complication rate were documented for the breast surgeries. Tumour characteristics of the tumour specimen included tumour type, grade, size, weight and volume, ER/PR/HER2/Ki67 status, and histologic type. Outcome measures for the axillary cases included frequency of retrieval of clipped node, total number of lymph nodes removed, and rates of axillary pathologic complete response.
SCOUT system and reflector insertion
The SCOUT system involves implantation of an infrared-activated electromagnetic wave reflector into a lesion of interest. The reflector has no external components and consists of an infrared light receptor, resistor, and two nitinol antennae that secure the reflector in the tissue (Fig. 1).21 The surgeon utilizes a transcutaneous handpiece that emits radar and infrared light and receives a radar signal back from the reflector. The SCOUT console processes the returned radar signal generating an audible signal that increases in cadence as the handpiece is moved over the reflector. The console also calculates the distance from the reflector facilitating an accurate real-time estimation of the location of the lesion and can be used to a depth of 60 mm with an accuracy of within 1 mm of the lesion.
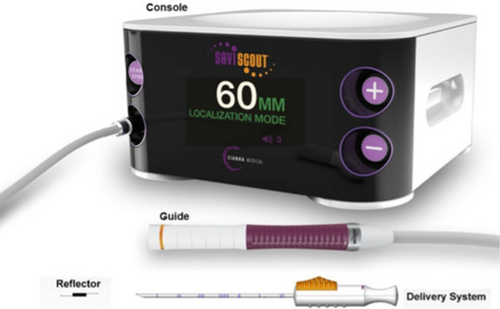
SCOUT reflectors were inserted by interventional breast radiologists under ultrasound guidance utilizing a preloaded 16-gauge needle. Multiple reflectors were used per case if bracketing was required, or in the event of multi-focality. A distance of at least 2 cm was maintained between reflectors in these cases. A post-deployment mammogram was performed to ensure accuracy of reflector placement. Reflector insertion was commonly planned within 2 weeks of surgery.
Surgery
All operations were performed by experienced breast surgeons with intraoperative specimen x-rays performed to ensure adequacy of lesion excision. WLE, excisional biopsy, TAD, and ALND were carried out in the usual manner except with SCOUT localization. Participating surgeons were surveyed following each procedure. Their experience with the SCOUT system for the first half of the cases was quantified with respect to ease of lesion localization and ease of reflector retrieval using a 5-point Likert scale from 1, which was considered ‘very easy’, to 5, which was considered ‘very difficult’.
Targeted axillary dissection
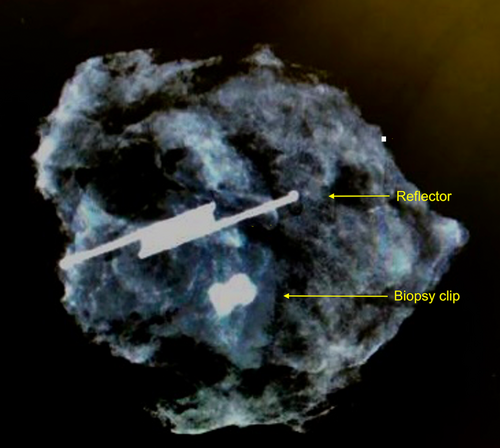
Patients that underwent TAD had placement of SCOUT reflectors into the previously biopsied metastatic lymph node(s) preoperatively within 2 weeks of surgery. Several patients had reflectors deployed at the time of lymph node biopsy prior to NAC. TAD was performed utilizing sentinel lymph node mapping and targeted excision of the SCOUT-lymph node following completion of NAC. All TAD patients underwent pre-operative lymphoscintigraphy with peritumoral and/or subareolar injections of technetium-99 m administered on the day of surgery or the day before surgery. Patent blue dye was administered intra-operatively. The reflector was tested pre-operatively after placement and prior to surgery to ensure proper functioning before each case. The sentinel node(s) and SCOUT-localized involved node(s) were identified utilizing a gamma probe and SCOUT probe, respectively, with a minimum of 3 nodes being excised for each TAD. An intraoperative x-ray was used to confirm retrieval of both the clip and the reflector for each axillary specimen (Fig. 2). All excised lymph nodes were sent for histopathological analysis.
Histopathology
Breast pathologists produced histopathological reports including biopsy result, surgical pathology, and margin status. A negative margin for invasive malignancy was considered no ink on the tumour and 2 mm for ductal carcinoma in situ. Close margin was defined as <2 mm for invasive and in situ pathology.
Statistical analyses
Continuous variables were presented as means with standard deviation (SD) or as median with interquartile ranges (IQR) and dichotomous and categorical data as frequencies with percentages. Statistical analysis was performed with RStudio, v2023.09.2.
Results
One hundred seventy-two consecutive patients were included in this study. A total of 195 SCOUT reflectors were used to identify 166 non-palpable breast lesions and 29 axillary lymph nodes (Table 1). Median interval between deployment of reflector and surgery was 3 days (range 1–20) and mean distance from reflector to lesion was 3.2 mm (SD 3.1). There were several patients that had reflector insertion at the time of lymph node biopsy and then subsequently had NAC. The mean operating time was 65.8 min (SD 33) and there was no incidence of reflector migration. No reflector deployment or localization-related complications were observed and there were no delays to theatre associated with reflector deployment. Surgeon reported ease of lesion localization and reflector retrieval on a Likert scale was 4.8 (SD 0.4) and 4.9 (SD 0.3), respectively. There was global satisfaction among surgeons with ease of localization being described as ‘easy’ or ‘very easy’ in 98% of the first 83 cases (48.3%).
| Procedure | Reflectors, n = 195† |
|---|---|
| Breast, n (%) | |
| Wide local excision | 130 |
| Excisional biopsy | 36‡ |
| Total | 166 |
| Axilla, n (%) | |
| Targeted axillary dissection | 26 |
| Axillary lymph node dissection | 3§ |
| Total | 29 |
- †195 total reflectors placed in a total of 172 patients. ‡Intraductal papilloma, sclerosed fibroadenoma, atypical ductal hyperplasia, scar, harmatoma. §SCOUT localization prior to neoadjuvant therapy.
Wide local excision
One-hundred-thirty WLE cases using SCOUT were performed. The demographics and tumour characteristics are presented in Table 2. Reflectors were placed at a median 3 days (IQR 2, 5) and there were no complications associated with the reflector placement procedure. The rate of successful intraoperative localization and reflector retrieval was 100%. Histopathology confirmed invasive disease in 83.8% and mean tumour size was 16.5 mm (SD 13.7). Median specimen weight was 27 g (IQR 15.1, 40), and median specimen volume was 55 cc (IQR 48.2, 65). Positive margin and re-excision rates were 10.8% and 13.1%, respectively (Table 3). Bracketing was successfully undertaken utilizing SCOUT in a subset of five patients. Surgeon reported ease of lesion localization and reflector retrieval was between ‘easy’ and ‘very easy’ for WLE cases (4.7 (SD 0.4) and 4.9 (SD 0.3), respectively).
| Whole cohort, n = 130 | |
|---|---|
| Age, mean (SD) | 56 (12.1) |
| ASA grade, median (IQR) | 2 (2, 2) |
| BMI, mean (SD) | 25.8 (3.5) |
| Pathology, n (%) | |
| IDC | 87 (66.9) |
| ILC | 11 (8.5) |
| DCIS | 16 (12.3) |
| Other | 8 (6.2) |
| Mixed | 3 (2.3) |
| Tumour size, mean mm (SD) | 16.5 (13.7) |
| Tumour grade, n (%) | |
| 1 | 28 (21.5) |
| 2 | 63 (48.5) |
| 3 | 18 (13.8) |
| Tumour characteristics, n (%) | |
| ER+ | 106 (81.5) |
| PR+ | 98 (75.4) |
| HER2+ | 21 (16.2) |
| Ki67 ≥ 14% | 54 (41.5) |
| Triple negative | 7 (5.4) |
- ASA, American Society of Anesthesiologists; BMI, body mass index; DCIS, ductal carcinoma in situ; ER+, oestrogen receptor positive; HER2+, human epidermal growth factor receptor 2 positive; IDC, invasive ductal carcinoma; ILC, invasive lobular carcinoma; IQR, interquartile range; PR+, progesterone receptor positive; SD, standard deviation.
| Whole cohort, n = 130 | |
|---|---|
| Days between reflector insertion and surgery, median days (IQR) | 3 (2, 5) |
| Tumour weight, median g (IQR) | 27 (15.1, 40) |
| Tumour volume, median cc (IQR) | 55 (48.2, 65) |
| Operation duration, mean mins (SD) | 69 (17.6) |
| Positive margin, n (%) | 14 (10.8) |
| Re-excision, n (%) | 17 (13.1) |
- CC, cubic centimetre; IQR, interquartile range; SD, standard deviation.
Targeted axillary dissection
A total of 26 patients completed NAC and underwent a SCOUT-guided TAD (Table 4). The median number of nodes removed was 4 (IQR 3, 6.5). The rate of successful placement was 100% with post-insertion mammogram corroborating placement accuracy. There were no complications associated with the reflector placement procedure. Reflectors were placed at a median 2 days (IQR 1.2, 4.8) and the rate of successful intraoperative localization of the clipped node and reflector retrieval was 100%. The reflector was within a lymph node in all patients and the metallic clip was seen within the SCOUT-lymph node on intraoperative specimen radiography. Surgeon reported ease of lesion localization and reflector retrieval for TAD cases was between ‘easy’ and ‘very easy’ (4.8 (SD 0.4) and 4.9 (SD 0.2), respectively). A complete pathological response in the axilla was observed in 65.4% (17/26) of cases (Table 5).
| Whole cohort, n = 26 | |
|---|---|
| Age, mean (SD) | 52.8 (11.6) |
| ASA grade, median (IQR) | 2 (2, 2) |
| BMI, mean (SD) | 25.4 (3.5) |
| Clinical nodal stage | |
| cN1 | 21 (80.8) |
| cN2-3 | 5 (19.2) |
| Tumour grade, n (%) | |
| 1 | 3 (11.5) |
| 2 | 8 (30.8) |
| 3 | 15 (57.7) |
| Tumour biomarkers, n (%) | |
| ER+ | 16 (61.5) |
| PR+ | 14 (53.8) |
| HER2+ | 6 (23.1) |
| Breast surgery, n (%) | |
| Wide local excision | 17 (68) |
| Mastectomy | 6 (21.1) |
| Operation duration, mean minutes (SD) | 77.5 (31.8) |
- ASA, American Society of Anesthesiologists; BMI, body mass index; ER+, oestrogen receptor positive; HER2+, human epidermal growth factor receptor 2 positive; IQR, interquartile range; PR+, progesterone receptor positive; SD, standard deviation.
| Whole cohort, n = 26 | |
|---|---|
| Days between reflector insertion and surgery, median days (IQR) | 2 (1.2, 4.8) |
| Total lymph nodes at TAD, median (IQR) | 4 (3, 6.5) |
| SCOUT-lymph node retrieved, n (%) | |
| Yes | 26 (100) |
| No | 0 |
| Reflector/clip in SCOUT-lymph node, n (%) | |
| Yes | 26 (100) |
| No | 0 |
| Nodal pCR at TAD, n (%) | |
| Yes | 17 (65.4) |
| No | 9 (34.7) |
- IQR, interquartile range; pCR pathologic complete response; TAD, targeted axillary dissection.
Discussion
This study identified high rates of successful reflector placement, intraoperative lesion localization, and reflector retrieval of SCOUT in the breast and axilla of 172 patients. Reflectors were inserted a median 3 days (range 1–20) prior to surgery without complication, and all were successfully localized and retrieved intraoperatively. This success included reflectors localized and retrieved for metastatic lymph nodes in the axilla. A notable difference observed with the implementation of SCOUT was the more directional nature of this system compared to the gamma probe. It required more deliberation and slower articulation of the handpiece to allow detection of the reflector. The learning curve of this technology was not evaluated in this study, but the ease of use was appreciated among the surgeons. Surgeons described the overall use of SCOUT as either ‘easy’ or ‘very easy’ in 98% of the first half of cases.
WL has been the mainstay of preoperative localization techniques for WLE of non-palpable breast lesions, but carries peri-operative scheduling challenges, patient discomfort, and risk of wire migration.22, 23 Wire localization has been the gold standard for localization of non-palpable breast lesions for decades. Its disadvantages from a patient and surgeon perspective have led to newer technologies. Intraoperative ultrasound has demonstrated equivalent clear margin and re-excision rates compared to WL but is operator dependant. Radioactive seeds has also shown equivalence to WL, but its use is not widely available due to strict radiation regulations in some countries. Magnetic markers, radiofrequency identification tags, carbon localization, and SCOUT appear to have potential but high-quality data is not yet available.13, 24, 25
Pilot data from the US on SCOUT localization was first published in 2016.12 A recent systematic review and pooled analysis of 842 cases from 11 studies demonstrated high deployment and retrieval rates of over 99% with SCOUT.13 There are however only a small number of cohort studies comparing SCOUT to standard WL, and a paucity of prospective evidence including localization of axillary lymph nodes with the SCOUT technique.13, 21-23, 26, 27 This current study adds more evidence to the literature on a technique that is not widely used, in particular with its feasibility in localizing axillary nodes during the current paradigm shift towards de-escalating axillary surgery. It also identified that SCOUT was an effective technique for localization of non-palpable breast lesions during WLE with acceptable positive margin and re-excision rates as supported by previous studies.13, 21-23, 26, 27 The technology also allowed for the planning of surgical incisions that are not predicated on the trajectory of a localizing wire. The need for coupling of radiological and surgical services due to the requirement for the day prior to surgery or same-day wire placement can potentially result in delays and inefficiencies in theatre utilization. Reflector placement was able to be performed well in advance of surgery in this current study, thus allowing more flexibility with coordinating theatre and radiology scheduling. There were no delays to theatre associated with reflector deployment. The Therapeutic Goods Administration does not stipulate a time limit for reflector placement. This enabled reflectors to be placed at the time of tumour and nodal clipping as an alternative to marking clips for several of the patients in this current study. A recent review of cases reported placement of reflectors up to 17 months prior to surgical excision with no deleterious effect.28 This approach could potentially reduce the number of interventions that patients require for localization and excision.
Until recently, ALND was routinely performed after neoadjuvant therapy in node-positive patients, irrespective of the response to treatment in the axilla. Although a growing body of evidence favours de-escalation of axillary surgery in this setting, the practical dilemma of identifying involved nodes at surgery remains vexing.29 While ALND remains the standard axillary staging procedure in node-positive breast cancer, TAD involving sentinel lymph node biopsy and targeted excision of the clipped lymph node in patients achieving nodal clinical response after NAC is an increasingly acceptable staging alternative.7, 30, 31 Some studies have found that TAD may improve staging accuracy over performing sentinel lymph node biopsy alone.31 Localization of the clipped lymph node after NAC is, however, associated with practical challenges and the ideal staging technique in this scenario has not been established.32, 33 These technical limitations could potentially be overcome with the placement of the localizing device into the metastatic lymph node prior to chemotherapy for targeted removal at surgery at a later date. Several patients in this current study also had the reflector placed into the metastatic axillary lymph node at the time of node biopsy prior to starting chemotherapy. A previous study was able to achieve accurate localization of axillary metastatic lymph nodes in all 25 patients using this approach.34 This could possibly be due to the metastatic lymph node being larger and more abnormal, allowing easier visualization on ultrasound prior to chemotherapy. A potential disadvantage of deploying reflectors prior to NAC is the possibility of axillary down-staging and not qualifying for TAD at time of surgery. There were no cases of the reflector migrating from the lymph node in this current study and this could be related to the physical features of the device being tiny and with two projecting antennae to anchor into the soft tissue after deployment. The current study demonstrated that SCOUT reflectors deployed in biopsy-confirmed metastatic nodes can help facilitate TAD.
During one TAD case, the clipped pre-operatively involved node was successfully identified outside of the anatomical borders of a conventional axillary clearance by SCOUT. The node was clearly below the level of the angular vein and may have otherwise been missed if a conventional axillary dissection had been performed. In another case, an on-table anaphylaxis led to cessation of surgery after 9 min. The TAD component of surgery was able to be successfully completed prior to abandonment of surgery due to the ease of use and accuracy of localization provided by SCOUT. The technique of bracketing was first described over 30 years ago with the suggestion that large areas of disease were better excised when the boundaries were delineated by multiple wires.35 Bracketing was successfully undertaken in this current study utilizing SCOUT in a small number of patients. There were no instances of failure of localization or failure of reflector retrieval, supporting the findings from a previous study.21 SCOUT also has excellent MRI compatibility compared to current wireless technologies with the least amount of artefact, which is especially useful if MRI is used during NAC.36
Strengths of this current study include the prospective nature in consecutive patients. It was limited by the small cohort resulting in the inability to power statistical significance which limits the strength of conclusions to be drawn. Its single institution nature may also not allow for generalizability. Larger prospective multi-centre studies, including randomized controlled trials, would help to further validate the efficacy of this technology. Future studies could also formally investigate the learning curve as surgical targeting with SCOUT, although similar in concept to lymphoscintigraphy for sentinel lymph node mapping and biopsy, is still a technically different approach. A significant challenge with moving to wireless technology is the cost considerations. Outside of capital cost, the main consideration for ongoing cost of using SCOUT is the reflectors in the pre-loaded delivery needle that are more expensive than the wires alone. Although it is more expensive than WL on a simple cost level, the total cost to the institution is a multifactorial economic analysis considering purchase price, reimbursement, radiology and theatre efficiencies, patient satisfaction, and other relevant quality metrics. SCOUT could potentially confer a considerable cost saving overall owing to avoidance of theatre delays and potentially speed of surgery, especially with respect to TAD. Cost-analysis studies would provide relevant insight to assist surgical units with purchasing decisions.20
In summary, this study demonstrated that SCOUT was an accurate and reliable method to localize and excise both breast and axillary lesions. It has potential to overcome some of the limitations of WL, but this warrants ongoing study.
Author contributions
Neshanth Easwaralingam: Conceptualization; formal analysis; investigation; methodology; writing – original draft; writing – review and editing. Chu Luan Nguyen: Conceptualization; data curation; formal analysis; investigation; methodology; writing – original draft; writing – review and editing. Fatema Ali: Formal analysis; investigation; writing – original draft; writing – review and editing. Belinda Chan: Conceptualization; writing – original draft; writing – review and editing. Susannah Graham: Conceptualization; writing – original draft; writing – review and editing. Fred Azimi: Conceptualization; writing – original draft; writing – review and editing. Cindy Mak: Conceptualization; writing – original draft; writing – review and editing. Sanjay Warrier: Conceptualization; data curation; formal analysis; investigation; methodology; writing – original draft; writing – review and editing.
Acknowledgements
The authors would like to thank the Sydney Breast Cancer Foundation for purchase of the SCOUT guidance system. Open access publishing facilitated by The University of Sydney, as part of the Wiley - The University of Sydney agreement via the Council of Australian University Librarians.
Conflicts of interest
None declared.
Open Research
Data availability statement
Available upon request from the corresponding author.