UNOS policy change benefits high-priority patients without harming those at low priority
Abstract
The heart transplantation policy change (PC) has improved outcomes in high-acuity (Old 1A, New 1–3) patients, but the effect on low-priority (Old 1B/2, New 4–6) patients is unknown. We sought to determine if low-priority patient outcomes were compromised by benefits to high-priority patients by evaluating for interaction between PC and priority status (PS). We included adult first-time heart transplant candidates and recipients from the UNOS registry during a 19-month period before and after the PC. We compared clinical characteristics and performed competing risks and survival analyses stratified by PC and PS. There was a dependence of PC and PS on waitlist death/deterioration with an interaction sub-distribution hazard ratio (adjusted sdHR) of 0.59 (0.45–0.78), p-value < .001. There was a trend toward a benefit of PC on waitlist death/deterioration (adjusted sdHR: 0.86 [0.73–1.01]; p = .07) and an increase in heart transplantation (adjusted sdHR: 1.08 [1.02–1.14], p = .007) for low-priority patients. There was no difference in 1-year post-transplant survival (log-rank p = .22) when stratifying by PC and PS. PC did not negatively affect waitlisted or transplanted low-priority patients. High-priority, post-PC patients had a targeted reduction in waitlist death/deterioration and did not come at the expense of worse post-transplant survival.
Abbreviations
-
- BMI
-
- body mass index
-
- IABP
-
- intra-aortic balloon pump
-
- IQR
-
- interquartile range
-
- MELD
-
- model for end-stage liver disease
-
- sdHR
-
- sub-distribution hazard ratio
-
- csHR
-
- cause-specific hazard ratio
-
- UNOS
-
- United Network of Organ Sharing
-
- VA-ECMO
-
- venoarterial-extracorporeal membrane oxygenation
1 INTRODUCTION
The six-tiered prioritization scheme implemented with the 2018 United Network for Organ Sharing (UNOS) policy change was designed to prioritize the sickest patients awaiting heart transplantation with the goal of decreasing waitlist mortality and improving donor organ availability. Several analyses of the 2018 policy change have examined the effect of the policy change on either waitlist outcomes and/or short-term post-transplant survival. The main findings of these analyses have demonstrated a decrease in waitlist death/deterioration, an increase in rates of heart transplantation, and either worse or unchanged short-term post-transplant survival.1-8 Some analyses were limited in interpretation due to informative censoring and repeated analyses have begun to address this issue.2, 8-10
An analysis of Status 1 patients bridged to heart transplantation with veno-arterial extracorporeal membrane oxygenation (VA-ECMO) identified reduced waitlist mortality, with shorter waitlist times, and improved post-transplant survival.3 Prior analyses demonstrated shorter waitlist times, reduced waitlist mortality and equivocal post-transplant survival in patients bridged to heart transplant with an intra-aortic balloon pump (IABP).5, 11, 12 One current limitation is that most analyses have examined outcomes for either all statuses or have focused on high-priority (Status 1 and Status 2) patients alone. One recent study by Fuery et al.13 provided an analysis of “low-priority” patients (Old 2, New 6) and contrasted these findings with “high-priority” patients (Old 1A, New 1 and 2). The authors found that low-priority patients had similar post-transplant survival before and after the UNOS policy change and longer waitlist times. Both low- and high-priority patients had shorter waitlist times after the policy change, however, lower priority patients received hearts from donors with greater comorbidities. While informative, this study did not assess for a potential interaction between the UNOS policy change and priority status and did not perform a competing risks analysis on waitlisted patients. As a result, it is currently unknown whether the observed benefits in waitlist and post-transplant outcomes in high-priority status patients negatively affect low-priority patients.
Thus, the purpose of this study was to evaluate the combined effect of priority status and policy change on waitlist and post-transplant outcomes for first-time adult heart transplant candidates and recipients and to determine if the gains seen in outcomes among high-priority patients came at a cost to low-priority patients.
2 MATERIALS AND METHODS
2.1 Database and patient cohort
After exempt status approval from the University of Southern California Institutional Review Board, we analyzed all adult (≥18 years old), first-time, heart transplant candidates that were single-organ heart transplant recipients from the UNOS Registry. Thus, a minority of heart transplant candidates in our cohort were listed for dual organ transplantation, but ultimately all recipients that underwent a heart transplant in our study cohort were single-organ recipients. We selected pre-policy (PRE) change and post-policy (POST) change time periods to address the differences in UNOS reporting requirements as have been discussed previously by Parker et al.9 and Hanff et al.4 Thus, the PRE time period was October 18, 2016 through May 30, 2018 and the POST time period was between October 18, 2018 through May 30, 2020. Inclusion into the competing risks cohort required waitlist registration within the PRE or POST time period, whereas inclusion in the survival analysis required both registration and transplantation within the PRE or POST time period. Like the study design of Goff et al,2 we chose the May 30th cutoff date to maximize follow-up of all transplant recipients in the POST era. This was done to minimize the potential effects of informative censoring due to delayed reporting of continued survival compared to mortality.9 Follow-up data was available through June 2021. There was a small number of patients that were either listed or transplanted with concurrent temporary mechanical circulatory support (tMCS) devices that had a “low-priority” status recorded in the UNOS registry. Due to this inconsistency, we chose to exclude these patients from our analysis as the presence of tMCS should have placed these patients in a “high-priority” status.
2.2 Definition of priority status
High-priority status was defined as Status 1A and Status 1–3 for the pre- versus post-policy era cohorts, respectively. Similarly, Old Status 1B/2 and Status 4–6 were defined as low-priority status for the pre- versus post-policy eras, respectively. Priority status for waitlisted patients was based on the initial priority status at the time of registration, while priority status for patients that underwent heart transplantation was based on their final priority status at the time of transplantation.
2.3 Statistical analysis
All analyses were performed with R Version 4.0.3. p-values for all analyses were two-sided with a significance level of .05.
2.3.1 Baseline characteristics
Baseline clinical characteristics of heart transplant recipients (or candidates) and heart transplant donors are presented as median with interquartile range (IQR) or frequency (percentage). Group comparison between continuous variables was performed using the Kruskal-Wallis test. Pearson's Chi-squared test or Fisher's exact test, depending on cell counts, were used to compare categorical variables. Additional pairwise comparison of subgroups was performed depending on the results of group comparisons (e.g., Mann–Whitney tests) and clinical relevance.
2.3.2 Competing risks analysis
A competing risks analysis was performed to calculate and compare the cumulative incidence between the following two events after being registered for heart transplantation: (1) death or deterioration or (2) heart transplantation. The competing risk analysis cohort was stratified by policy era (PRE or POST, as defined above). Unadjusted cumulative incidence curves for the outcome of interest (heart transplant or death/deterioration) between PRE and POST patients were compared using Gray's test.14 Patients listed in the PRE cohort that did not undergo an event (death/deterioration or heart transplantation) by the time of the policy change were censored on October 18, 2018; to permit the same amount of time on the waitlist; similar administrative censoring was performed on the POST cohort for patients not experiencing an event by October 18, 2020. Multivariable Fine-Gray proportional sub-distribution hazards models15 and cause-specific Cox proportional hazards models were used to evaluate the adjusted policy-era and listing priority status effect on waitlist outcomes. For each outcome of interest, the initial multivariable model included demographic characteristics (i.e., gender, race, BMI, age) with additional clinical variables selected based on a priori clinical relevance and existing publications.3, 6, 8, 16 Hemodynamic measurements were not included in the multivariable models due to many missing observations.
2.3.3 Survival analysis
Unadjusted post-transplant survival (freedom from death or graft failure) between PRE and POST patients was estimated using Kaplan–Meier curves and differences in survival were compared using a standard log-rank test. A multivariable Cox proportional hazards model17 was used to evaluate the effect policy era had on post-transplant survival, adjusting for other variables. Patients registered for a heart transplant in the PRE era and transplanted in the POST era were censored as alive on October 18, 2018. Additionally, patients were censored at the time of the last follow-up or at 365-days post-heart transplant, whichever occurred first. Variable selection for our multivariable model was done like that described above for our competing risks analysis. To avoid issues of multicollinearity, we chose to only include one predictor when two or more highly correlated predictors (e.g., BMI and body surface area, MELD score, and creatinine or total bilirubin levels) are recommended for the multivariable model.
3 RESULTS
3.1 Comparison of baseline characteristics by priority status at the time of listing
See Table 1 for a comparison of baseline characteristics (stratified by policy era and priority status) at the time of listing.
| High-priority status at listing | Low-priority status at listing | |||||||
|---|---|---|---|---|---|---|---|---|
| PRE ERA (N = 1434) | POST Era (N = 2000) | p-value | # Missing | PRE Era (N = 4261) | POST Era (N = 3379) | p-value | # Missing | |
| 1A (Old policy) | 1434 | - | - | - | - | - | - | |
| 1B (Old policy) | - | - | - | 2749 (64.5) | - | - | ||
| 2 (Old policy) | - | - | - | 1512 (35.5) | - | - | ||
| 1 | - | 218 (10.9) | - | - | - | - | ||
| 2 | - | 1091 (54.5) | - | - | - | - | ||
| 3 | - | 691 (34.5) | - | - | - | - | ||
| 4 | - | - | - | - | 2134 (63.2) | - | ||
| 6 | - | - | - | - | 1245 (36.8) | - | ||
| Age | 55 [45, 63] | 55 [44, 63] | .273 | - | 56 [46, 63] | 56 [47, 63] | .888 | - |
| Gender (% Male) | 1048 (73.1) | 1488 (74.4) | .408 | - | 3133 (73.5) | 2445 (72.4) | .264 | - |
| Ethnicity | .166 | - | .275 | - | ||||
| Asian | 56 (3.9) | 89 (4.4) | - | 119 (2.8) | 96 (2.8) | - | ||
| Black | 354 (24.7) | 511 (25.6) | - | 973 (22.8) | 824 (24.4) | - | ||
| Hispanic | 126 (8.8) | 212 (10.6) | - | 360 (8.4) | 306 (9.1) | - | ||
| Other | 19 (1.3) | 17 (0.9) | - | 52 (1.2) | 32 (0.9) | - | ||
| White | 879 (61.3) | 1171 (58.6) | - | 2757 (64.7) | 2121 (62.8) | - | ||
| Body Mass Index (kg/m2) | 27.1 [23.6, 31.1] | 27.1 [23.7, 31.5] | .663 | 4 | 27.9 [24.5, 31.7] | 28.4 [24.8, 32.1] | <.001 | - |
| Blood type | .762 | 8 | ||||||
| A | 575 (40.1) | 736 (36.8) | .256 | 1562 (36.7) | 1250 (37.0) | |||
| AB | 70 (4.9) | 97 (4.9) | 195 (4.6) | 144 (4.3) | ||||
| B | 231 (16.1) | 347 (17.3) | 567 (13.3) | 429 (12.7) | ||||
| O | 558 (38.9) | 820 (41.0) | 1937 (45.5) | 1556 (46.0) | ||||
| History of cigarette usea | 656 (45.7) | 821 (41.0) | .007 | - | 1922 (45.1) | 1498 (44.3) | .514 | - |
| History of ischemic cardiomyopathya | 328 (22.9) | 443 (22.1) | .646 | - | 809 (19.0) | 538 (15.9) | .001 | - |
| History of diabetes mellitusa | 419 (29.2) | 555 (27.8) | .366 | - | 1195 (28.0) | 976 (28.9) | .434 | - |
| Prior cardiac surgerya | 563 (39.3) | 678 (33.9) | .001 | - | 1665 (39.1) | 1466 (43.4) | <.001 | - |
| Dialysis after listinga | 28 (2.0) | 41 (2.1) | .902 | - | 31 (0.7) | 16 (0.5) | .185 | - |
| Implantable cardioverter defibrillatora | 991 (69.1) | 1287 (64.3) | .004 | - | 3335 (78.3) | 2557 (75.7) | .008 | - |
| On mechanical ventilation at listing | 67 (4.7) | 90 (4.5) | .876 | - | - | - | NA | - |
| On intravenous inotropes at listing | 638 (44.5) | 918 (45.9) | .433 | - | 1117 (26.2) | 729 (21.6) | <.001 | - |
| Hemodynamics at listing | ||||||||
| Cardiac index (L/min/m2) | 2.11 [1.72, 2.58] | 2.00 [1.64, 2.45] | <.001 | 260 | 2.12 [1.78, 2.51] | 2.11 [1.79, 2.49] | .716 | 266 |
| Pulmonary capillary wedge pressure, mm Hg | 20 [13, 26] | 21 [15, 27] | .006 | 466 | 17 [11, 24] | 16 [10, 22] | <.001 | 327 |
| IABP at listing (%) | 230 (16.0) | 636 (31.8) | <.001 | - | - | - | - | - |
| VA-ECMO at listing (%) | 94 (6.6) | 152 (7.6) | .27 | - | - | - | - | - |
- a Counts based on the number of confirmed affirmative responses in the database.
3.1.1 High-priority patients
There were significantly more patients listed at high priority status in the POST era (2000/5379 [37.2%] vs. 1434/5695 [25.2%], p-value < .001). The median age was similar at 55 years old. A similar majority of patients of the male gender was present in both eras. Fewer patients had implantable cardioverter defibrillators in the POST era (64.3% vs. 69.1%, p = .004). There were also fewer patients with a history of prior cardiac surgery in high-priority POST-era patients (39.3% vs. 33.9%, p = .001). There was a similar number of patients listed on mechanical ventilation (90 [4.5%] patients vs. 67 [4.7%] patients, p = .876) and VA-ECMO (152 [7.6%] patients vs. 94 [6.6%] patients, p = .27) in the POST and PRE eras, respectively. Consistent with prior studies, IABP use was significantly increased in the POST era (636 [31.8%] patients vs. 230 [16.0%] patients, p < .001). Cardiac index was significantly, but only marginally, lower in the POST-era at 2.00 L/min/m2 versus 2.11 L/min/m2, p < .001.
3.1.2 Low-priority patients
The median age was similar between eras at 56 years old. Again, there was a similar majority of male patients in both eras. Fewer patients in the POST era were on IV inotropes at the time of listing (21.6% vs. 26.2%, p < .001). There was no difference in baseline cardiac index between the two eras (p = .716).
3.2 Comparison of baseline characteristics by priority status at the time of heart transplantation
See Table 2 for a comparison of baseline characteristics (stratified by policy era and priority status) at the time of heart transplantation.
| High-priority status at transplant | Low-priority status at transplant | |||||||
|---|---|---|---|---|---|---|---|---|
| Recipient characteristics | PRE Era (N = 1863) | POST Era (N = 2447) | p-value | # Missing | PRE Era (N = 833) | POST Era (N = 639) | p-value | # Missing |
| 1A (Old policy) | 1863 | - | - | - | ||||
| 1B (Old policy) | - | - | - | 766 (92.0) | - | |||
| 2 (Old policy) | - | - | - | 67 (8.0) | - | |||
| 1 | - | 274 (11.2) | - | - | - | |||
| 2 | - | 1554 (63.5) | - | - | - | |||
| 3 | - | 619 (25.3) | - | - | - | |||
| 4 | - | - | - | - | 512 (80.1) | |||
| 6 | - | - | - | - | 127 (19.9) | |||
| Age | 57 [47, 63] | 56 [46, 63] | .026 | - | 58 [48, 65] | 58 [47, 64] | .713 | - |
| Time on waitlist (days) | 43 [16, 115] | 15 [6, 52] | <.001 | - | 65 [23, 154] | 62 [23.50, 153] | .995 | - |
| Gender (Male, %) | 1377 (73.9) | 1811 (74.0) | .971 | - | 534 (64.1) | 378 (59.2) | .059 | - |
| Ethnicity | .329 | - | .241 | - | ||||
| Asian | 67 (3.6) | 104 (4.3) | 33 (4.0) | 19 (3.0) | ||||
| Black | 432 (23.2) | 570 (23.3) | 169 (20.3) | 128 (20.0) | ||||
| Hispanic | 154 (8.3) | 235 (9.6) | 82 (9.8) | 62 (9.7) | ||||
| Other | 22 (1.2) | 22 (0.9) | 11 (1.3) | 2 (0.3) | ||||
| White | 1188 (63.8) | 1516 (62.0) | 538 (64.6) | 428 (67.0) | ||||
| Body mass index (kg/m2) | 26.93 [23.62, 30.58] | 27.06 [23.63, 31.07] | .464 | 5 | 27.18 [23.92, 30.91] | 27.80 [24.67, 31.17] | .02 | - |
| Blood type | .311 | - | .269 | - | ||||
| A | 768 (41.2) | 950 (38.8) | 397 (47.7) | 320 (50.1) | ||||
| AB | 104 (5.6) | 125 (5.1) | 79 (9.5) | 62 (9.7) | ||||
| B | 288 (15.5) | 397 (16.2) | 138 (16.6) | 117 (18.3) | ||||
| O | 703 (37.7) | 975 (39.8) | 219 (26.3) | 140 (21.9) | ||||
| History of cigarette usea | 862 (46.3) | 1017 (41.6) | .002 | - | 364 (43.7) | 270 (42.3) | .616 | - |
| History of ischemic cardiomyopathya | 553 (29.7) | 654 (26.7) | .035 | - | 264 (31.7) | 183 (28.6) | .228 | - |
| Dialysis after listinga | 33 (1.8) | 50 (2.0) | .576 | - | 3 (0.4) | 1 (0.2) | .637 | - |
| Diabetes mellitusa | 518 (27.8) | 669 (27.3) | .761 | - | 234 (28.1) | 172 (26.9) | .659 | - |
| Prior cardiac surgerya | 746 (40.0) | 856 (35.0) | .001 | - | 308 (37.0) | 244 (38.2) | .664 | - |
| Implantable cardioverter defibrillatora | 1428 (76.7) | 1708 (69.8) | <.001 | - | 655 (78.6) | 470 (73.6) | .026 | - |
| Total bilirubin | 0.70 [0.50, 1.10] | 0.70 [0.50, 1.20] | .002 | 4 | 0.60 [0.40, 1.00] | 0.60 [0.40, 0.90] | .069 | 2 |
| Creatinine | 1.16 [0.95, 1.43] | 1.12 [0.90, 1.40] | .001 | 1 | 1.11 [0.91, 1.39] | 1.15 [0.92, 1.40] | .259 | - |
| MELD-XI Score | 9.44 [5.90, 12.91] | 9.34 [5.76, 12.86] | .637 | 4 | 8.74 [5.54, 11.86] | 8.71 [5.17, 12.15] | .663 | 2 |
| On mechanical ventilation | 17 (0.9) | 77 (3.1) | <.001 | - | - | - | - | - |
| On intravenous inotropes | 779 (41.8) | 1192 (48.7) | <.001 | - | 347 (41.7) | 151 (23.6) | <.001 | - |
| IV antibiotics within 14-days of transplanta | 206 (11.1) | 312 (12.8) | .1 | - | 19 (2.3) | 6 (0.9) | .076 | - |
| Cardiac index (L/min/m2) | 2.22 [1.83, 2.68] | 2.07 [1.71, 2.54] | <.001 | 177 | 2.20 [1.87, 2.62] | 2.18 [1.87, 2.61] | .97 | 35 |
| Mean pulmonary artery pressure, mm Hg | 26 [20, 34] | 28 [21, 36] | <.001 | 143 | 24 [18, 32] | 23 [17.75, 30] | .002 | 46 |
| Pulmonary capillary wedge pressure, mm Hg | 17 [11, 24] | 20 [13, 25] | <.001 | 316 | 15 [10, 21] | 14 [9, 20] | .007 | 48 |
| VA-ECMO at time of transplant | 28 (1.5) | 179 (7.3) | <.001 | - | - | - | - | - |
| IABP at time of transplant | 253 (13.6) | 1024 (41.8) | <.001 | - | - | - | - | - |
- a Counts based on the number of confirmed affirmative responses in the database.
3.2.1 High priority
More patients underwent heart transplantation from a high-priority status in the POST era compared to the PRE-era (2447/3086 [79.2%] vs. 1863/2696 [69.1%], p-value < .001). Time on the waitlist was notably shorter in the high-priority POST era patients (15 days vs. 43 days, p < .001). The median age was between 56 and 57 years old in the two groups. Approximately 74% of high-priority heart transplant recipients, both PRE and POST, were male gender. In stark contrast to the similar percentage of patients being on VA-ECMO at the time of listing (see above), there was a marked increase during the POST era in the percentage of patients that underwent heart transplantation from VA-ECMO (7.3% vs. 1.5%, p < .001). Heart transplantation from IABP support was more common in the POST era (41.8% vs. 13.6%, p < .001). There was a significant increase in heart transplantation from mechanical ventilation in the POST era (3.1% vs. 0.9%, p < .001). This is despite the similar frequency of listing for heart transplantation while on mechanical ventilation between the PRE and POST eras (see above). Not surprisingly, cardiac index (p < .001) was significantly lower and pulmonary capillary wedge pressure (p < .001) was significantly higher in the POST era.
3.2.2 Low priority
There was a trend toward fewer patients of the male gender undergoing heart transplants from a low-priority status in the POST versus PRE era (59.2% vs. 64.1%, p = .059). Overall, a greater fraction of women underwent heart transplantation at low-priority status compared to high-priority status (p < .001).
3.3 Donor characteristics
See Table 3 for donor characteristics stratified by high-priority and low-priority status and PRE/POST eras.
| High-priority status at transplant | Low-priority status at transplant | |||||||
|---|---|---|---|---|---|---|---|---|
| Donor characteristics | PRE Era (N = 1863) | POST Era (N = 2447) | p-value | # Missing | PRE Era (N = 833) | POST Era (N = 639) | p-value | # Missing |
| Donor age | 31 [23, 39] | 31 [24, 39] | .878 | - | 32 [24, 41] | 33 [26, 43] | .002 | - |
| Donor gender (male, %) | 1298 (69.7) | 1885 (77.0) | <.001 | - | 496 (59.5) | 326 (51.0) | .001 | - |
| Donor female, recipient male | 264 (14.2) | 231 (9.4) | <.001 | - | 123 (14.8) | 101 (15.8) | .633 | - |
| Donor ethnicity | .617 | - | .209 | - | ||||
| Asian | 26 (1.4) | 39 (1.6) | 15 (1.8) | 8 (1.3) | ||||
| Black | 309 (16.6) | 403 (16.5) | 139 (16.7) | 84 (13.1) | ||||
| Hispanic | 302 (16.2) | 438 (17.9) | 119 (14.3) | 86 (13.5) | ||||
| Other | 35 (1.9) | 48 (2.0) | 17 (2.0) | 10 (1.6) | ||||
| White | 1191 (63.9) | 1519 (62.1) | 543 (65.2) | 451 (70.6) | ||||
| Donor body mass index (kg/m2) | 26.4 [23.2, 30.7] | 26.7 [23.7, 31.0] | .02 | 2 | 26.0 [22.9, 30.3] | 26.7 [23.1, 32.0] | .029 | - |
| DONOR blood type | .011 | - | .007 | - | ||||
| A | 681 (36.6) | 818 (33.4) | 381 (45.7) | 302 (47.3) | ||||
| AB | 37 (2.0) | 27 (1.1) | 33 (4.0) | 46 (7.2) | ||||
| B | 175 (9.4) | 250 (10.2) | 130 (15.6) | 109 (17.1) | ||||
| O | 970 (52.1) | 1352 (55.3) | 289 (34.7) | 182 (28.5) | ||||
| Donor total bilirubin | 0.70 [0.50, 1.10] | 0.70 [0.50, 1.10] | .682 | 5 | 0.70 [0.50, 1.20] | 0.60 [0.40, 1.10] | .011 | - |
| Donor creatinine | 1.00 [0.75, 1.58] | 1.05 [0.80, 1.60] | .009 | 5 | 0.95 [0.71, 1.40] | 1.04 [0.75, 1.65] | .004 | - |
| Donor MELD-XI | 8.30 [3.52, 14.6] | 8.76 [3.92, 14.8] | .061 | 5 | 7.84 [2.71, 13.8] | 8.15 [3.25, 15.1] | .198 | - |
| Ischemic time (hours) | 3.10 [2.33, 3.72] | 3.48 [2.92, 4.02] | <.001 | 19 | 2.97 [2.22, 3.62] | 3.20 [2.38, 3.88] | <.001 | 10 |
| Donor-hospital to recipient hospital distance | 83 [13, 261] | 259 [106, 412] | <.001 | - | 65 [11, 215] | 150 [27, 335] | <.001 | - |
| Donor history of hypertension | 304 (16.3) | 359 (14.7) | .149 | - | 127 (15.2) | 125 (19.6) | .035 | - |
| Donor history of diabetes | 78 (4.2) | 74 (3.0) | .049 | - | 30 (3.6) | 33 (5.2) | .181 | - |
| LVEF | 60 [56, 65] | 60 [55, 65] | .933 | 4 | 60 [58, 65] | 60 [55, 65] | .204 | 1 |
| PHS High-risk donor | 591 (31.7) | 849 (34.7) | .044 | 0 | 258 (31.0) | 261 (40.8) | <.001 | - |
| BMI ratio (donor/recipient) | 0.99 [0.85, 1.17] | 1.00 [0.86, 1.19] | .179 | 7 | 0.97 [0.84, 1.14] | 0.98 [0.83, 1.16] | .435 | - |
| Predicted heart mass ratio (donor/recipient) | 1.01 [0.91, 1.13] | 1.03 [0.93, 1.17] | <.001 | 2 | 1.00 [0.91, 1.11] | 0.99 [0.90, 1.10] | .167 | - |
| Donor cause of death | .07 | 0 | <.001 | - | ||||
| Anoxia | 740 (39.7) | 1038 (42.4) | 312 (37.5) | 314 (49.1) | ||||
| CVA/Stroke | 268 (14.4) | 321 (13.1) | 132 (15.8) | 111 (17.4) | ||||
| Head trauma | 806 (43.3) | 1013 (41.4) | 376 (45.1) | 195 (30.5) | ||||
| CNS/Tumor | 11 (0.6) | 7 (0.3) | 2 (0.2) | 2 (0.3) | ||||
| Other | 38 (2.0) | 68 (2.8) | 11 (1.3) | 17 (2.7) | ||||
3.3.1 High-priority recipients
Donor age was similar between eras (p = .878). Male gender donors were more common in the POST era (77.0% vs. 69.7%, p < .001) and female donor/recipient male combinations were less common in the POST era (9.4% vs. 14.2%, p < .001). As has been shown before, donor ischemic times were longer in the POST era (3.48 vs. 3.10 h, p < .001). The predicted heart mass ratio (donor/recipient) was marginally higher in the POST era (1.03 vs. 1.01, p < .001).
3.3.2 Low-priority recipients
Use of male donors was less common in the POST era (51% vs. 59.5%, p < .001), while female donor/recipient male combinations in low-priority recipients were similar across eras (p = .633). Donor ischemic times in low-priority patients remained higher in POST era patients (3.20 vs. 2.97 h, p < .001).
3.4 Waitlist outcomes
3.4.1 Death/deterioration
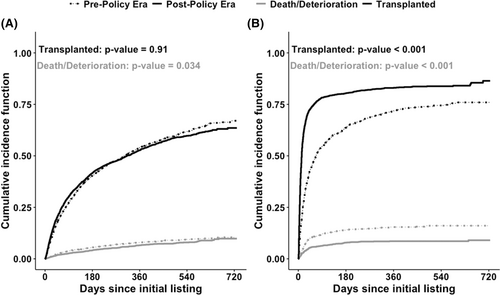
The cumulative incidence plots for the waitlist outcome of death/deterioration stratified by policy era and initial listing priority status are shown in Figure 1. The cumulative incidence of waitlist death/deterioration was lower in the POST era when compared to the PRE era for both low- and high-priority patients (p = .034 and p < .001, respectively). However, this difference was noticeably larger in the high-priority patients (Figure 1—right panel) than in the low-priority patients (Figure 1—left panel). The results of the Fine-Gray model, adjusted for additional confounders, are shown in Table 4. There was a non-significant trend toward a beneficial effect of PC on the cumulative incidence of waitlist death/deterioration for patients initially listed as low priority (adjusted sdHR: 0.86 [0.73–1.01]; p = .07 - see Table 4). Patients who were initially listed at high priority status have a significantly lower cumulative incidence of waitlist death/deterioration in the POST era than those who are in the PRE era (adjusted sdHR: 0.51 [0.41–0.63]; p-value < .001 - see Table 4). When looking at the interaction term (Status × Policy), we found a significant dependence between policy era and initial priority status on the cumulative incidence of waitlist death/deterioration (adjusted sdHR: 0.59 [0.45–0.78], p-value < 0.001 - see Table 4). In contrast to the subdistribution hazards results, the cause-specific hazard ratios (see Table 5) examining the effect of the policy era on death/deterioration were not significant for initial high-priority status patients (adjusted cause-specific hazard ratio [csHR]: 1.07 [0.87–1.31], p = .55). On the other hand, there was a trend toward a protective effect of policy era on initial low-priority status patients (adjusted csHR: 0.86 [0.73–1.01], p = .07), but did not meet significance. We did not observe a dependence (or interaction) between policy era and initial priority status (Status × Policy) on the cause-specific hazard (adjusted csHR: 1.23 [0.95–1.61], p = .12). Overall, there was a discrepancy in the sdHR and csHR for the waitlist outcome of death/deterioration.
| Waitlist death/deteriorationa | Heart Transplantationb | |||
|---|---|---|---|---|
| sdHR (95% CI) | p-value | sdHR (95% CI) | p-value | |
| Post vs. Pre (initial Low-priority status) | 0.86 (0.73, 1.01) | .07 | 1.08 (1.02, 1.14) | .007 |
| Post vs. Pre (initial High-priority status) | 0.51 (0.41, 0.63) | <.001 | 2.16 (1.96, 2.38) | <.001 |
| Interaction Term (status × policy) | 0.59 (0.45, 0.78) | <.001 | 2.00 (1.79, 2.23) | <.001 |
- Notes: Each main effect is modeled as a binary covariate: Policy = PRE/POST, Priority Status = LOW/HIGH as defined in the main text. While the interaction term, by itself, is difficult to interpret, the p-value assess whether or not the effect policy (PRE/POST) has on the outcome of interest is dependent on/modified by priority status (Low/High) and vice versa. Abbreviation: sdHR, sub-distribution hazards ratio.
- a Adjusted for age, gender, race, blood type, BMI, diabetes mellitus, mechanical ventilation at registration, and prior cardiac surgery after listing.
- b Adjusted for age, gender, race, blood type, BMI, diabetes mellitus, mechanical ventilation at registration, prior cardiac surgery after listing, ischemic cardiomyopathy, and dialysis after listing (12 observations were omitted due to missing values). The sdHR in the first two rows restricts calculation to either only initial low-priority status at listing patients or initial high-priority status at listing patients, respectively.
| Waitlist death/deteriorationa | Heart transplantationb | |||
|---|---|---|---|---|
| csHR (95% CI) | p-value | csHR (95% CI) | p-value | |
| Post vs. Pre (initial Low-priority status at listing) | 0.86 (0.73, 1.02) | .09 | 1.07 (1.00, 1.13) | .046 |
| Post vs. Pre (initial High-priority status at listing) | 1.07 (0.87, 1.31) | .55 | 2.20 (2.04, 2.39) | <.001 |
| Interaction Term (status × policy) | 1.23 (0.95, 1.61) | .12 | 2.07 (1.87, 2.29) | <.001 |
- Notes: Each main effect is modeled as a binary covariate: Policy = PRE/POST, Priority Status = LOW/HIGH as defined in the main text. While the interaction term, by itself, is difficult to interpret, the p-value assess whether or not the effect policy (PRE/POST) has on the outcome of interest is dependent on/modified by priority status (low/high) and vice versa. Abbreviation: csHR, cause-specific hazards ratio.
- a Adjusted for age, gender, race, blood type, BMI, diabetes mellitus, mechanical ventilation at registration, and prior cardiac surgery after listing.
- b Adjusted for age, gender, race, blood type, BMI, diabetes mellitus, mechanical ventilation at registration, prior cardiac surgery after listing, ischemic cardiomyopathy, and dialysis after listing (12 observations were omitted due to missing values). The csHR in the first two rows restricts calculation to either only initial low-priority status at listing patients or initial high-priority status at listing patients, respectively.
3.4.2 Heart transplantation
The cumulative incidence of heart transplantation (Figure 1) was significantly higher in the POST era than in the PRE era for those listed as either high (adjusted sdHR: 2.16 [1.96–2.38], p < .001) or low (adjusted sdHR: 1.08 [1.02–1.14], p = .007) priority. The interaction term (Status × Policy) demonstrated a significant dependence of policy era and initial priority status (adjusted sdHR: 2.00 [1.79–2.23], p < .001) on heart transplantation (Table 4). The cause-specific hazard ratios (csHR) for the waitlist outcome of heart transplantation were nearly identical to the corresponding sdHRs (see Table 4 and Table 5).
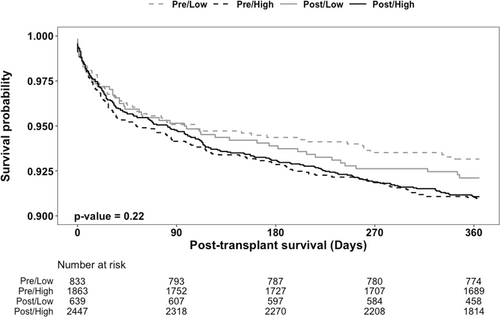
3.5 One-year post-transplant survival
We also examined the impact of policy era and final priority status at transplant on 1-year post-transplant survival. Kaplan–Meier curves of the four subgroups, stratified by policy status and priority status, are shown in Figure 2. We observed that 1-year post-transplant survival did not differ when stratified by policy change and final priority status (log-rank p-value = 0.22). The multivariable Cox model (Table 6) suggests there was no impact of policy change, irrespective of listing status, on 1-year post-transplant survival (HR: 1.03 [0.70–1.51], p-value = .90); see Table 6. Furthermore, there was no significant interaction between policy and listing status on 1-year post-transplant survival (HR: 0.85 [0.55–1.32], p = .5; see Table 6).
| Variable | Hazard ratio (95% CI) | p-value |
|---|---|---|
| Policy change | 1.03 (0.70, 1.51) | .90 |
| Listing status at transplant | 1.26 (0.93, 1.70) | .14 |
| Interaction (Policy × Listing status) | 0.85 (0.55, 1.32) | 0.50 |
- Notes: Analysis was adjusted for age, gender, race/ethnicity, BMI at transplant, blood type, ischemic cardiomyopathy, prior cardiac surgery, ventilator, dialysis after listing, diabetes mellitus, total bilirubin, creatinine at transplant, and intravenous antibiotics 14 days prior to a heart transplant, ischemic time.
4 DISCUSSION
In this analysis of UNOS data pre- and post-policy change, we observed the following: (1) POST era patients had a significant reduction in the cumulative incidence of waitlist death/deterioration and increase in heart transplantation, (2) waitlist outcomes were either the same or improved for low-priority patients, and (3) there was no significant difference in 1-year post-transplant survival across all subgroups. Taken together, adult, first-time, high-priority, POST era patients received a targeted reduction in waitlist death/deterioration, and an increase in access to heart transplantation, without worsening waitlist or survival outcomes in low-priority patients. As such, the overall effects of the UNOS policy change appear to be meeting the intended goal of improving waitlist survival via improved access to donor hearts for the highest urgency patients and does so without harming low-priority patients.
One noteworthy result to focus on is the discrepancy between the subdistribution and cause-specific hazard ratios for the waitlist outcome of death/deterioration. Specifically, there was no decrease in the cause-specific HR for (1) the interaction (Status × Policy) between the policy era and initial priority status or (2) the effect of the policy era on only the initial high-priority status patients. The sdHR on the other hand was reduced (protective) for these two categories (interaction and initial high-priority status patients). We interpret this discrepancy to mean that the decreased cumulative incidence of waitlist death/deterioration is driven primarily by the rapid rate of heart transplantation rather than by the policy change per se. In other words, the primary byproduct of the policy change appears to be more rapid heart transplantation in higher acuity patients, and this secondarily leads to a decreased cumulative incidence of death or deterioration. We base this interpretation18, 19 on the understanding that a cause-specific hazards model provides a causal (or etiologic) interpretation of the effect of policy change on outcomes, whereas the subdistribution hazards model is limited to predicting the outcome of the patient at some time after being listed for a heart transplant. This is consistent with the lack of an effect of policy change on waitlist death/deterioration in our cause-specific hazards analysis. Regardless of the interpretation, the policy change appears to be meeting its overall goal of rapidly providing donor hearts to the highest acuity patients on the waitlist. Moreover, there is no signal for harm to any patient subgroup in our analysis.
Our study adds to the literature by providing an analysis of the interaction, or dependence between, the UNOS policy change of 2018 and patient priority status. Our analysis sought to answer whether the gains seen in hospitalized and mechanically supported patients in the new allocation system came at the expense of worse outcomes in lower priority, ambulatory patients. Based on this analysis, lower priority patients had no observable adverse effects. As alluded to above, one potential mechanism for the observed targeted benefits to high priority, POST era patients is that status upgrades provide a means to “rescue” waitlisted ambulatory patients that suffer from an acute decompensation; we did observe an overall increase in heart transplantation in low-priority patients in the POST era. Similarly, patients with no prior history of cardiomyopathy who present in acute cardiogenic shock also benefit from the “rescue” effect of the policy change. A recent analysis highlighted that one drawback of the rapid time to heart transplantation under the new policy has been an association with a small, but significant reduction in observed myocardial recovery.20 Additional tools to identify patients that have an increased likelihood of recovery are therefore needed.
Another important observation is that there was a similar proportion of patients on VA-ECMO at the time of listing for both the PRE and POST eras, however, there were approximately 4.9 times more patients transplanted from VA-ECMO in the POST era compared to the PRE era. This further highlights the importance of an allocation policy that prioritizes patients based on clinical acuity. As shown by Gonzalez et al,3 there was both a substantial waitlist and post-transplant survival benefit in VA-ECMO bridged patients during the POST era. Similarly, we previously observed12 significant waitlist benefits for POST era IABP-supported (status 2) patients bridged to heart transplantation without any difference in post-transplant survival. Additionally, our analysis identified a nearly 3-fold increase in the number of patients undergoing heart transplantation from mechanical ventilation. This appears to support the idea that in the POST era transplant centers are more inclined to take risks on sicker patients than before; however, an alternative interpretation is that centers are instead prioritizing patients with “sicker therapies.” Whether this represents patient advocacy, “gaming” or simply treating patients according to agreed-upon consensus cardiogenic shock criteria is debatable. Nonetheless, future iterations of the organ allocation policy should consider instances where the cardiogenic shock criteria fall short in risk stratification and whether additional markers of end-organ malperfusion should be incorporated.21
We deliberately selected our study inclusion time periods to minimize the risk of informative censoring to our post-transplant survival analysis. With this in mind, repeated analysis with more complete follow-up will be important to ensure that reported findings to date regarding the effects of the allocation policy remain accurate.9, 10
Another notable finding in our analysis is that fewer women donors appear to be selected in high-priority patients. In concert with this, there has been less utilization of female donors for male recipients, especially in high-priority patients. While this change was not found to be a predictor of post-transplant survival, higher status patients are likely seeing more organ offers and thus some programs may have less incentive to accept gender mismatched organs. This finding warrants a dedicated evaluation.
4.1 Limitations
The major limitations of this study are those imposed by data entry limitations and inconsistencies present in a large registry. Another limitation is that waitlisted patients were stratified based on initial listing status, which is frequently different than the status listing at the time of heart transplantation. With this in mind, many low-priority patients based on their initial listing status were transplanted at a higher priority status, and, therefore, the waitlist outcomes analyzed for the low-priority patients are likely biased by this discrepancy. There were large numbers of missing hemodynamic variables and therefore these parameters were not accounted for in our regression analyses.
5 CONCLUSIONS
We observed that in the post-policy era that high-priority transplant candidates have a large and targeted reduction in waitlist death/deterioration, while waitlist outcomes for low-priority patients were either improved or no different. One-year post-transplant survival was not affected by policy change or priority status. Taken together, these findings support the conclusion that high-priority patients have benefited from the policy change and low-priority patients have not been harmed. Additional analyses of other patient subgroups are needed to evaluate for potential inequities that may remain despite the recent UNOS policy change.
AUTHOR CONTRIBUTIONS
Study design: AMW, ECD, ESK, ASV. Data analysis: AMW, ECD, ESK, ASV. Writing of the manuscript: AMW, ECD, ESK, SST, MWF, LZ, KP, ASV.
FUNDING INFORMATION
ESK was supported by the National Institute of Environmental Health Sciences (NIEHS) grant # T32ES013678.
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
Open Research
DATA AVAILABILITY STATEMENT
UNOS registry data is freely available from the OPTN. R code for our analysis is available upon request.