November 14–15, 2023, T1DX-QI Learning Session, Journal of Diabetes Abstracts
Abstract #1 Reduction in hospitalizations for underserved young adults (YA) with type 1 diabetes (T1D) in the supporting emerging adults with diabetes (SEAD) program: An adult-based healthcare transition model
Priyanka Mathias1; Clyde Schechter2; Judith A Long2, Shivani Agarwal1
1Fleischer Institute of Diabetes and Metabolism, Division of Endocrinology, Montefiore Medical Center and Albert Einstein College of Medicine, Bronx, New York, USA. 2Department of Family and Social Medicine, Albert Einstein College of Medicine, Bronx, New York, USA; 3University of Pennsylvania Perelman School of Medicine, Philadelphia, Pennsylvania, USA.
Objective: YA with T1D transitioning from pediatric to adult care experience increased risk of hospitalization and premature mortality. We report hospitalization outcomes from a four-year analysis of the Supporting Emerging Adults with Diabetes (SEAD) program, an adult-based healthcare transition receivership program offering developmentally appropriate YA-centered care.
Methods: We planned a priori SEAD program evaluation by collecting lab, prescription, and health utilization data prospectively from 2019 to 2022 on YA with T1D receiving SEAD endocrinology care compared with non-SEAD endocrinology care. We used Cox proportional hazards model to compare incidence of hospitalization and logistic regression to compare hospitalization days between SEAD and non-SEAD participants over time.
Results: From 2019 to 2022, 416 YA with T1D received SEAD (n = 244) or non-SEAD (n = 172) care. SEAD YA were younger, higher proportion of Hispanic race-ethnicity, and commercially insured (p < 0.05), but had similar HbA1c levels at baseline (9.2%, p = 0.624). In multivariate analysis, accounting for differences in baseline demographics, SEAD participants had 20% lower incidence of hospitalizations (HR 0.80 [0.625, 1.045]) and spent less days in hospital (−0.49 days [−0.64, −0.35]). High-risk YA with HbA1c > =9% had a 34% lower incidence of hospitalizations (HR 0.66 [0.49, 0.88]).
Conclusions: Receiving care in the SEAD program resulted in reduction in overall hospitalizations and less days spent in hospital, with an even more pronounced benefit for high-risk YA with HbA1c levels ≥9%. Improvement in hospitalization outcomes could have long-term impacts on longitudinal YA outcomes and overall cost effectiveness.
Keywords: Young Adults, Transition care, Hospitalizations, Diabetes-related hospitalizations
Abstract #2 Promoting continuous glucose monitoring (CGM) prescriptions in academic training clinics
Jovan Milosavljevic1; Rohan Maini2; Sarah Baron2; Jing-Yu Pan2; Priyanka Mathias1; Shivani Agarwal1,3
1Fleischer Institute of Diabetes and Metabolism, Division of Endocrinology, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, New York, USA. 2Department of Medicine, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, New York, USA. 3Fleischer Institute of Diabetes and Metabolism, New York-Regional Center for Diabetes Translation Research, Division of Endocrinology, Albert Einstein College of Medicine, Bronx, New York, USA
Objective: Academic training clinics often serve the most vulnerable patients with diabetes. CGM could be a transformative diabetes management tool, yet little is understood about CGM prescribing behaviors in training clinics. We examined CGM prescription rates and associated factors to plan new quality improvement initiatives (QI) in our training clinics.
Methods: We extracted CGM prescription and demographic data from the electronic health record. Patients were eligible if they had completed an outpatient visit in selected endocrinology or primary care training clinics from January to March 2023. We used descriptive statistics and logistic regression to measure overall CGM prescription rates and associated factors.
Results: We included 244 eligible patients from endocrinology (n = 96) or primary care (n = 148) training clinic (mean age 58.5 ± 14.7, 48% female, 50% Hispanic, 23% non-Hispanic Black, 24% Spanish preferred, 10% T1D). CGM prescription rate overall was 26%: 64% Libre, 33% Dexcom, 2% both brands. In multivariate regression, CGM was 89% less likely to be prescribed in primary care versus endocrinology (OR 0.11 [0.05–0.22], p < 0.001) and 56% less likely if Hispanic race-ethnicity (OR 0.44 [0.22–0.89], p = 0.02), despite no difference in preferred language.
Conclusions: CGM prescriptions were overall low, which was expected in primary care, but unexpected in endocrinology training clinics. CGM was less likely to be prescribed for patients of Hispanic race-ethnicity but was not associated with Spanish language preference. CGM prescribing behaviors must be further examined in academic training clinics to better inform subsequent QI interventions.
Keywords: continuous glucose monitoring; training clinic; health equity
Abstract #3 Implementing an early T1D clinic for patients with stage 1 and stage 2 type 1 diabetes
Kimber MW Simmons; Lexie Chesshir; Holly K O'Donnell; Paige Trojanowski; Taylor M Triolo; G. Todd Alonso; Rebecca Campbell; Andrea K Steck; Peter Gottlieb; Brigitte Frohnert
Barbara Davis Center for Diabetes, University of Colorado Anschutz Medical Campus Aurora, CO, USA
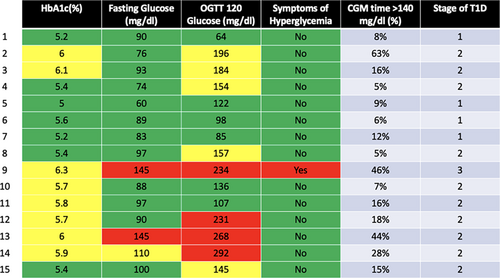
Background/Objective: Teplizumab-mzwv was approved for delaying onset of stage 3 type 1 diabetes in November 2022. We designed an early T1D clinic to identify individuals eligible for treatment and provide proper guidance around treatment options.
Methods: In December 2023, we opened a weekly clinic staffed with a nurse, physician and psychologist. Individuals with islet autoimmunity and concern for dysglycemia are offered metabolic staging, which includes a fasting glucose level, HbA1C, 2-h OGTT, and 10-day CGM wear. Patients are offered a health and behavior assessment to assess coping and T1D risk perception. Metabolic staging results are obtained during clinic and treatment options are discussed. If a patient desires Teplizumab-mzwv therapy, we prescribe and initiate the prior authorization process.
Results: We have completed staging in 15 patients (TABLE). Using ADA T1D staging criteria, 10/15 (67%) patients are stage 2, 4/15 (27%) are stage 1, and one patient was diagnosed with stage 3. Of those with stage 2, we have successfully infused a 14-day course of teplizumab-mzwv in four patients aged 10, 14, 15, and 32 years. One patient initially classified as stage 2 progressed to symptomatic T1D before treatment. Two additional stage 2 patients are authorized for teplizumab-mzwv treatment, and three are under review for treatment by their insurance carriers.
Conclusions: Individuals attending Early T1D clinic tolerated complete metabolic staging per ADA guidelines. Of those meeting criteria for teplizumab-mzwv treatment, all wanted to pursue therapy. We successfully treated approximately half of eligible patients to date.
Abstract #4 Systematically developing and piloting an eating disorder screening process at a large pediatric diabetes clinic
Paige Trojanowski; Bailey Tanner; Rebecca Campbell; G. Todd Alonso; Holly K. O'Donnell
Barbara Davis Center for Diabetes, University of Colorado Anschutz Medical Campus Aurora, CO, USA
Background/Objective: People with type 1 diabetes (T1D) are at increased risk for eating disorders, which can lead to severe medical complications and compromised diabetes care. Despite heightened risk, most pediatric diabetes clinics do not routinely screen for disordered eating. Of those who do, less than half use a validated measure. This study aimed to (1) describe the process for developing an eating disorder screening protocol at a large pediatric diabetes clinic, (2) report preliminary results piloting the protocol, and (3) describe provider response to screening.
Methods: We completed a gap analysis, selected a validated measure of disordered eating and method of administration, developed a screening process (including templated documentation), and trained providers on screening procedures. Cycles included biweekly multidisciplinary team meetings, gathering feedback from diabetes providers, and consultation with an expert from an outside institution.
Results: Gap analysis revealed 0.0009 of 3207 active patients aged 12–25 years had disordered eating documented in their medical record. REDCap was used to record patient responses to the Diabetes Eating Problems Survey–Revised (DEPS-R) and entered into a medical record flowsheet. Providers recognized need for screening; however, lack of confidence discussing disordered eating and weight/shape concerns necessitated multiple staff trainings. Review of provider notes revealed inconsistency in documentation for one of five providers. Piloting (N = 28, Mage = 17.7, SD = 3.1 years) revealed 28.6% positive scores (M = 14.4, SD = 10.5, range 4–42).
Conclusions: Eating disorder screening is feasible and will help centers meet American Diabetes Association screening recommendations. Increasing provider comfort and confidence addressing elevations is essential to success.
Keywords: Behavioral medicine, Delivery of health care, Eating disorders, Needs assessment, Type 1 diabetes
Abstract #5 Understanding facilitators and barriers to clinic-wide implementation of a population-based tool to identify patients with type 1 diabetes (T1D) at high risk for suboptimal glycemic outcomes
Emily L. DeWit1, Katie Noland1, Sophie MacColl1, Franziska Bishop2, Mark Clements1
1Children's Mercy Kansas City, 2Stanford School of Medicine
Background/Objective: To gain insights from clinicians to inform clinic-wide implementation of a CGM-based population health management tool (Ferstad et al, 2021) that identifies patients in need of support due to the presence of suboptimal glycemic outcomes.
Methods: We recruited diabetes clinicians (physicians, nurses, dieticians, a fellow and a social worker) at a pediatric hospital in the Midwestern United States to participate in QUEST, a qualitative study designed to gather input to inform design and implementation of patient and provider-facing care delivery interventions. Clinician experience ranged from 2 months to 25 years (average 6 years) in their current role, and clinicians were naive to the tool. Participants completed an electronic survey that included a video introduction to the Timely Interventions for Diabetes Excellence (TIDE) platform, followed by 34 Likert scale, multiple choice, and free text response questions. The Capability, Opportunity, Motivation, and Behavior (COM-B) model and Organizational Readiness for Implementing Change (ORIC) scale provided the framework for these questions.
Results: Fifty-six clinicians received study information; 20 consented to participate. Participants perceived that the platform could serve as a proactive tool to support youth to improve glycemic management. Clinicians scored on average 45/60 on the ORIC scale, suggesting an overall readiness for implementing this change. Clinicians endorsed lack of time and training as barriers to implementing the tool. They identified that de-implementing ineffective clinical practices could address time as a barrier.
Conclusion: Results will guide implementation of the TIDE platform in new organizations.
Keywords: continuous glucose monitoring, glycemic management, implementation, population health
Abstract #6 Effect of remote patient monitoring on subsequent three-month hemoglobin A1c (HbA1c) in youths and young adults with type 1 diabetes (T1D) with suboptimal glycemic outcomes
Claire Petty1; Britaney Spartz1; Erin M. Tallon1; Kelsey Panfil; Emily L1; Craig Vandervelden; Brent Lockee; Katie Noland; Mark Clements
Children's Mercy Kansas City; Kansas City, Missouri, USA
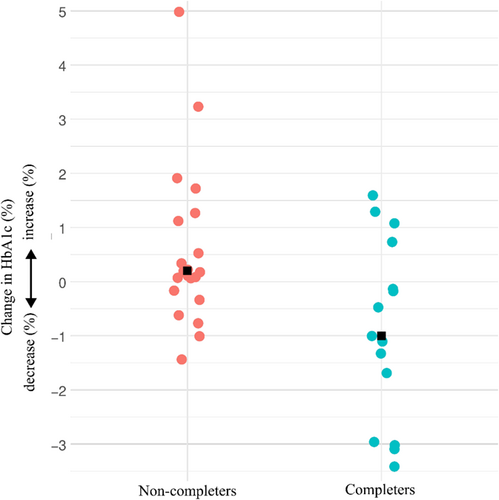
Background/Objective: Deterioration of glycemic management between diabetes clinic visits is common in youth and young adults (YYA) with T1D. Remote Patient Monitoring (RPM) is a telehealth intervention that offers patients additional one-on-one visits with healthcare providers between standard clinic visits, focusing on optimizing diabetes self-management. We investigated whether YYA with elevated HbA1c (≥9.0%) who participate in RPM, versus those who do not, experience improved HbA1c.
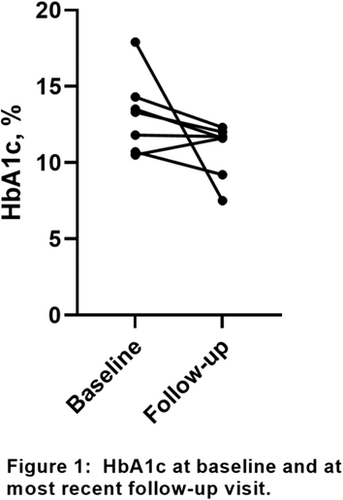
Methods: We retrospectively analyzed data from 36 YYA (36.1% female; 14.8 [12.7–15.8] years, median [IQR] age; 83.3% CGM users; 52.8% pump users) seen at a tertiary diabetes clinic (Midwest USA; 2020–2023). All patients had ≥2 elevated HbA1c results (≥9.0%) within 12 months and were offered RPM. Of these, 15 patients enrolled and completed at least one 15–20-min RPM visit; 21 patients did not. We evaluated change in HbA1c in those who did and did not complete an RPM visit (completers and non-completers, respectively) by comparing baseline HbA1c (the qualifying HbA1c [≥9.0%]) and HbA1c obtained 3 months after RPM was offered.
Results: HbA1c improved in 73.3% (11/15) of completers and 28.6% (6/21) of non-completers. In completers, median change in HbA1c was −1.0%; in non-completers, median change was +0.2% (Figure 1). In completers whose HbA1c improved, median change was −1.3%.
Conclusions: Completers experienced a substantial decrease in median HbA1c. By facilitating proactive diabetes management, RPM for YYA with elevated HbA1c (≥9.0%) may lead to significant improvements in glycemic management. Future research with larger matched patient cohorts is warranted, to enable rigorous evaluation of intervention efficacy and ideal dose.
Abstract #7 Strategies to improve smart pen uptake–lessons learned from a pediatric diabetes center
Brian Miyazaki; Jose Aceves; Jessica Alula; James Connard; Lily C. Chao
Center for Endocrinology, Diabetes and Metabolism, Children's Hospital Los Angeles Los Angeles, CA, USA
Background: Smart insulin pen (SIP) can improve consistency and accuracy of insulin dosing. Its uptake has been slow in children with diabetes. We participated in the T1DX-QI Collaborative Project to increase shared decision making and equitable access of SIP use.
Methods: Between December 2022 and April 2023, we implemented three major interventions with four clinicians: (1) the Diabetes Technology Assessment tool (not specific to SIP), (2) pictorial handout of diabetes technologies, and (3) diabetes technology sample boxes to provide visual and tactile demonstrations (SIP, insulin pod, pumps, and sensors). We tracked changes in technology usage after the intervention was implemented. In parallel, our center partnered with the SIP (Inpen) manufacturer to pilot a new workflow. This workflow included an instruction booklet, sample pen, virtual training, while the vendor seeks insurance authorization.
Results: Between December 2022 to April 2023, we documented 45 total share decision making instances (N = 31 for type 1, N = 45 for type 2 diabetes; 18 already using continuous glucose monitor [CGM]), of which 64% (N = 29) resulted in proposed changes in technology. 65% (N = 19) elected to trial CGM, 28% (N = 8) showed interest in insulin pump, and 20% (N = 6) showed interest in SIP technology. Among patients interested in the latter, none initiated SIP. Barriers to SIP initiation included copay requirement, lack of insulin cartridge samples in clinic to facilitate in-clinic device training, and poor responsiveness when trainer reaches out to family.
Conclusions: Successful implementation of SIP may require minimizing cost and infrastructure to facilitate pen initiation during the clinical encounter.
Keywords: Diabetes mellitus, type 1; diabetes mellitus, type 2, shared decision making; insulin pen
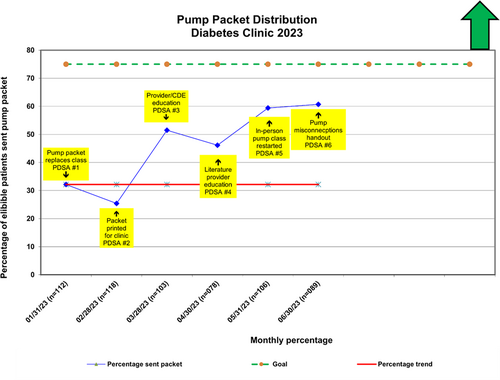
Abstract #8 Reducing requirements for pump referral improves pump initiation for publicly insured patients
Brian Miyazaki; Jennifer Baldwin; James Connard; Jose Aceves; Casey Berman; Jessica Ferris; Rebecca Ortiz La Banca Barber; Debbie Miller; Lily C. Chao
Center for Endocrinology, Diabetes and Metabolism, Children's Hospital Los Angeles, Los Angeles, CA, USA
Background: Conventional process (CP) for insulin pump initiation strives to optimize insulin doses prior to obtaining insurance authorization. Disparity in completion of the CP exists in publicly insured patients with type 1 diabetes (PWD). We hypothesize that reducing requirements for insulin pump initiation will improve pump access and reduce health inequity.
Methods: We created a new pathway (NP) for insulin pump referral for PWD, consisting of a virtual informational session conducted in English, collection of two-weeks of glucose readings, and two phone calls with a diabetes nurse. Pump training was conducted virtually. Data was collected from patients over 6 months at a large urban children's hospital. We compared insulin pump clearance, initiation, and insurance status between patients in the CP and NP. Fisher's exact test and student t-test were used for analysis, with p < 0.05 considered significant.
Results: The demographic data from CP (N = 63) and NP (N = 34) were comparable in gender (54% vs 52%) and insurance status (public insurance 71% for both). Pump clearance occurred more commonly in NP (p = 0.015). There was no difference in pump initiation among those who completed requirements (p > 0.999). Patients with public insurance were 5.6-times as likely to initiate insulin pump in the NP (p = 0.0023, 95% CI 1.817 to 17.90).
Conclusions: Reducing requirements for insulin pump improves access for publicly insured patients. Future studies are needed to determine if outcomes differ in patients from diverse language and social-economic status.
Keywords: Type 1 Diabetes, Insulin Infusion Systems, Health Equity
Abstract #9 Developing a tracking tool for continuous glucose monitor prescriptions among children and young adults with type 1 and type 2 diabetes
Amanda Perkins; Mai Tran; Jody Grundman; Sarah Lydia Holly; Jennifer Reilly; Shideh Majidi
Children's National Hospital, 111 Michigan Ave NW, Washington, DC, 20010
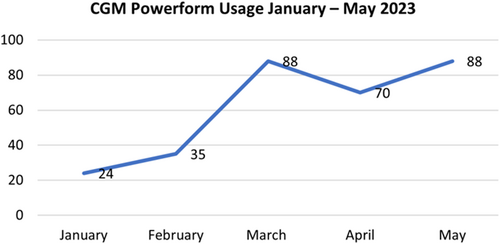
Background/Objective: Rates of Continuous Glucose Monitor (CGM) uptake remain suboptimal despite evidence that CGM use improves diabetes outcomes. Successful CGM uptake requires a multi-disciplinary team of prescribers, pharmacists, diabetes educators and administrative staff. Ability to track the process is a strategy to increase uptake.
Methods: Inability to track new CGM prescriptions through initiation, fulfillment and patient education and was identified in a key driver diagram of barriers to uptake. Process mapping was completed with input from a multi-disciplinary team. Iterative Plan-Do-Study-Act cycles were undertaken to develop a tracking tool which was integrated into the Cerner electronic medical record (EMR), trialed with key staff for 6 weeks, rolled-out department-wide for 3 months, and enhanced based on user feedback.
Results: The CGM Powerform (CGMPF) consists of four tabs accessible for documentation by a multi-disciplinary team. When initiated by the prescriber, the CGMPF sends a prompt to the pharmacist alerting of a new CGM request. Separate tabs allow for documentation of insurance-required record submission, prior authorizations and appeals for patients with durable medical equipment or pharmacy benefits, and patient education. A total of 305 CGMPFs (Figure) were initiated since inception.
Conclusions: A CGMPF embedded in the EMR creates a centralized location for documentation of new CGM prescriptions and allows for a multi-disciplinary team to follow progress. Extracted data from this form will identify areas for further process improvement and disparities in the process. The QI team plans to implement a similar form to track insulin pump initiation.
Keywords: Continuous Glucose Monitors, Quality Improvement, Technology, Pediatric Diabetes
Abstract #10 Improving access to closed-loop technology (IMPACT)
Kristina Cossen1, Sobenna George1, Anna Albritton2, Kristine Jaknke2, Alison Higgins2, Pat Tatro2, and Angela Bryant Curry2
1Division of Endocrinology, Department of Pediatrics, Emory+ Children's Pediatric Institute, Atlanta, GA, USA; Children's Healthcare of Atlanta, Atlanta, GA, USA
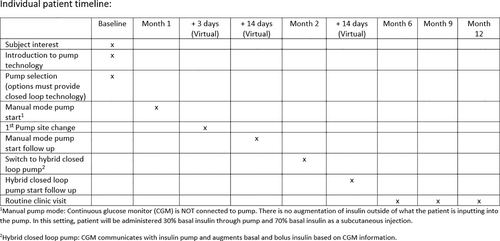
Background/Objective: Despite documented benefits in diabetes technology, the utilization inequalities continue. We propose a pilot program focused on improving rates of closed-loop systems in a pre-defined at-risk pediatric type 1 diabetes (T1D) population.
Methods: The Diabetes Support Program (DSP) implemented at CHOA in 2016 aims to reduce acute diabetes complications in patients at high-risk, defined as more than 2 DKA (diabetes ketoacidosis) events within 12 months, or at-risk, defined as 1 DKA within 12 months (diagnoses event excluded). DSP includes a psychologist, a dedicated clinical diabetes educator (CDE) and social worker. Technology utilization has not been a focus. With the addition of 3 providers and 3 CDEs, patients within the DSP population interested in pump technology with insurance that approves closed-loop systems were approached for enrollment. To improve compliance, the team simplified pump initiation and proposed an untethered start. (see table 1).
Results: In 2022, DSP comprised of 276 of the 3410 patients with T1D followed at Children's Healthcare of Atlanta. Compared to patients not enrolled, DSP patients had HbA1c on average 2.4% higher, were more likely to receive Medicaid (75% vs 47%) and be non-white (66% vs 49%). Pump use was lower in the DSP (24 vs 42%). Difficulties encountered for enrollment in IMPACT include identifying and confirming appropriate candidates, making contact with families outside of clinic and ensuring that patients have a general understanding of carbohydrate counting.
Conclusions: This quality initiative pilot aims to show high-risk patient populations can safely improve their diabetes care using insulin pump therapy through a supportive, tailored program. Enrollment in this project is ongoing.
Abstract #11 Sustained quality improvement implementation of a transition preparation program for adolescents and emerging adults with type 1 diabetes
Sarah D. Corathers; Rajvi Desai; Rachael Jones; Kyle Kaplan; Mary Jolly; Jessica C. Kichler
Cincinnati Children's Hospital Medical Center, University of Cincinnati College of Medicine Cincinnati, OH USA
Background/Objective: Transition of care (TOC) for adolescents and emerging adults (AEA) with type 1 diabetes (T1D) is complex. Despite consensus on the need for transition preparation, implementation strategies to initiate and sustain a program remain limited. The purpose of this quality improvement (QI) initiative is the development and maintenance of a pediatric T1D transition program over time.
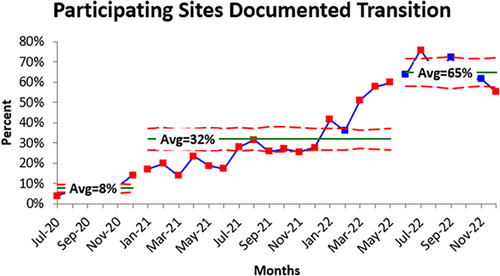
Methods: A multidisciplinary QI team identified key drivers consistent with Got Transition guidelines including: (1) establishing expectations for families and staff, (2) integrating transition readiness assessment into clinic workflow, and (3) documenting transition plan and longitudinal tracking. Interventions with iterative PDSA cycles addressed each of these drivers. Primary outcome of % AEA with documented transition plan was tracked over time using a run chart. A convenience sample of patients was followed to track post-transfer outcomes.
Results: Cincinnati Children's Diabetes Center adopted a transition policy, developed standard tracking, uses READDY assessment tool, documents transition planning, partners with adult receivership practices, and uses a care coordinator to confirm successful transfer. Over 5 years the percentage of patients with T1D ages 15–18 years with a documented TOC plan increased from 10% to 80% and over age 19 years with documented TOC plan from 20% to over 90%. Mean age of transfer of convenience sample (n = 54) is 22 years; one-year post-transfer HbA1c value was stable.
Conclusions: Improving the percentage of AEA patients with TID with documented TOC plans is feasible and sustainable using QI methods supported by diabetes specific transition readiness tools and care delivery processes.
Keywords: Diabetes Mellitus, Type 1; Pediatric Transition to Adult Care
Abstract #12 Mind the gap: Lessons learned from addressing inequities in CGM Access
Nana-Hawa Yayah Jones; Amy Grant; Sarah Corathers; Laura Smith; Jennifer Kelly; Amanda Riley; Desireé N. Williford; Kyle Kaplan; Amanda Howell
Cincinnati Children's Hospital Medical Center Cincinnati, Ohio, USA
Background/Objective: In healthcare mind the gap refers to addressing health disparities. Inequities in rates of healthcare utilization and adverse outcomes are systematically overrepresented in patients from marginalized communities. Our diabetes team is working diligently to close these gaps—specifically by promoting the use of diabetes technology.
Methods: Between June 2021 and 2023, we implemented several targeted strategies: barriers assessment; CGM sampling program; DEI training; listening sessions; onsite pharmacy and DME distribution; shared decision-making tool; social determinants of health screening; targeted patient outreach; and voice of the customer videos. Health-equity-focused QI tools and Iterative Plan-Do-Study-Act (PDSA) cycles were used to monitor and assess implementation, impact, and improvement opportunities. Health outcomes were collected via patient registry. Data were stratified by race and insurance.
Results: CGM usage among patients identifying as Black increased from 38% to 63% and from 65% to 86% for those identifying as White (reduced gap by 4%). CGM usage among patients on public insurance increased from 56% to 80% and from 77% to 89% for patients on private insurance (reduced gap by 12%). Mean HbA1c for patients on public insurance decreased from 9.4% to 8.9% and from 9.9% to 9.6% for Black patients.
Conclusions: Multi-faceted, targeted interventions and QI methodology resulted in improved CGM utilization while simultaneously improving glycemic outcomes in T1D patients by race and insurance. Iterations of these interventions have demonstrated the importance of redesigning innovative, transformative, and inclusive healthcare solutions in partnership with patients.
Keywords: CGM access; Equity; Health disparities; Quality Improvement; Type 1 diabetes
Abstract #13 ConnecT1D: A care model designed to achieve excellent and equitable glycemic and psychosocial outcomes for youth with type 1 diabetes (T1D)
Sarah Corathers; Nana-Hawa Yayah Jones; Pat Bradyc; Laura Smith; Amanda Howell; Kyle Kaplan; Dimitrios Makrozahopoulos; Justin Masterson; Amanda Riley; Amy Grant
Cincinnati Children's Hospital Medical Center, University of Cincinnati College of Medicine, Cincinnati, Ohio, USA
Background/Objective: Despite remarkable advancement of diabetes technology, outcomes for youth with T1D remain suboptimal and the impact of diabetes-related morbidity disproportionately affects youth of minority race or ethnicity, and those experiencing poverty. By focusing design on needs of medically and socially vulnerable youth with T1D, ConnecT1D aims to reorient diabetes care from episodic visits to proactive delivery model that supports families through equitable access to technology, community partnerships, and communication between visits.
Methods: People with T1D and caregivers, clinicians, quality improvement (QI) specialists, social workers, and diabetes educators participated in a Design Session (n = 27 attendees). Four focus areas generated 130 ideas and over 50 candidate interventions to improve HbA1c and related process measures for a cohort of youth with T1D on public insurance (n = 293). The team pursued iterative PDSA cycles to test interventions including social determinants of health screening, diabetes community health worker, embedded psychologist, addressing barriers to diabetes technology access, and proactive dose adjustments between visits.
Results: At baseline, youth with public insurance had lower rates of diabetes technology access and 1% higher mean HbA1c. After 1 year of ConnecT1D interventions, 95% had consistent clinic visits, 68% had visit with psychology; CGM increased from 56% to 80%, insulin pump increase from 55% to 65%, Mean HbA1c decrease from 9.4% to 8.9% with narrowing of health disparities in all metrics.
Conclusions: Participatory design and QI methodology resulted in improved access to diabetes technology, psychosocial supports, and glycemic outcomes while reducing health disparity gaps for children with T1D on public insurance.
Keywords: Diabetes Mellitus, Type 1; Health Equity; Glycated Hemoglobin; Community Health Services
Abstract #14 Increasing insulin pump use by adapting pump enrollment process
Stephanie Ogburn; Candice Williams; Christin Morell; Luke Cielonko; Susan Hsieh
Cook Children's Medical Center, Fort Worth, TX, USA
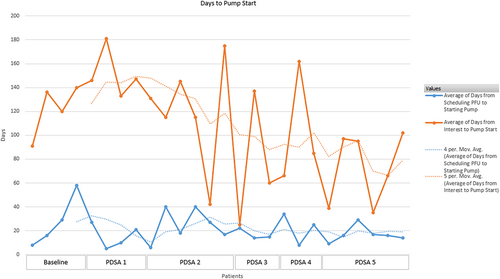
Background/Objective: Insulin pump therapy in Type 1 diabetes has been associated with lower hemoglobin A1c. The objective of this project is to decrease time from pump interest to pump start to less than 100 days in 12 months and secondary objective to increase pump use by 15% from baseline at Cook Children's Endocrinology and Diabetes Clinic.
Methods: Providers identified 29 patients for group pump follow up (PFU), virtual pump class or phone PFU. The following interventions tested in rapid PDSA cycles: Group pump training/group PFU (10), Phone PFU contacted on two consecutive Fridays (4), and Phone PFU, contacted on Friday after training (15).
Results: Before implementing interventions, families waited 90–150 days to attend class and another 30–180 days for in-person PFU. After implementation, the time between pump interest to initiation improved from 122 days to 105 days. The aim of 15% pump use was not met. Barriers identified include provider bias, insurance/pharmacy problems, patient preference, and appointment availability.
Conclusions: Implementing virtual pump class/phone PFU allowed families to start insulin pump therapy in a shorter period. Use of fishbone diagram/PDSA were effective in improving wait time. Future steps include development of a patient led pump Education and identifying provider barriers to earlier pump therapy.
Abstract #15 Managing diabetes ketoacidosis in a moderate care unit: A quality improvement initiative
Nellie S. Hani; Ashley Garrity; Athina Sikavitsas*; Christine E. Mikesell^; Kimberly K. Monroe^; Inas Thomas
Division of Pediatric Endocrinology; *Division of Pediatric Emergency Medicine; ^Division of Pediatric Hospital Medicine, University of Michigan, Ann Arbor, MI, USA
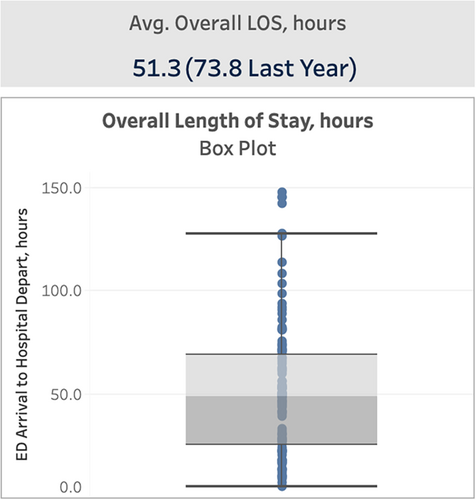
Background: Pediatric diabetes ketoacidosis (DKA) has been managed either in the emergency department (ED) or pediatric intensive care unit (PICU) at our institution. Our objective was to establish a moderate care unit on the general pediatrics floor to care for patients with mild–moderate DKA. We hypothesized this shift in our care model would shorten overall length-of-stay (LOS), improving bed availability and reducing patient burden.
Methods: We used quality improvement (QI) methods to map the current state and proposed moderate care workflows. Members from pediatric endocrinology, hospital medicine, ED, and nursing reviewed the proposed workflow and collaborated with pharmacy, phlebotomy, and information technology staff to ensure all elements of the workflow could be executed. The team collaboratively developed educational materials and delivered training for residents, nurses, and attending physicians. Patients with “mild–moderate DKA” were characterized as those with a pH on a venous blood gas (VBG) of ε7.2 and a serum bicarbonate ε13. Eligible patients were ε5 years old. Patients meeting these criteria were transitioned to moderate care.
Results: From May 2022 to June 2023, 25% of DKA patients (n = 28) were cared for under this new workflow. When compared to DKA patients treated the previous year, overall hospital LOS decreased by 30% from an average of 73.8 h to an average of 51.3 h (Figure 1). No untoward events occurred with need to reinstate an insulin drip.
Conclusions: We found that mild–moderate DKA can be successfully cared for in a moderate care setting, shortening LOS for hospitalized patients who present in DKA.
Abstract #16 Improving glycemic management in patients with type 1 diabetes through time in range patient education
Alexander Waselewski; Ashley Garrity; Christina Finn; Janet Dominowski; Elizabeth S. Sandberg; Inas Thomas; Joyce M. Lee
Division of Pediatric Endocrinology, University of Michigan, Ann Arbor, MI, USA
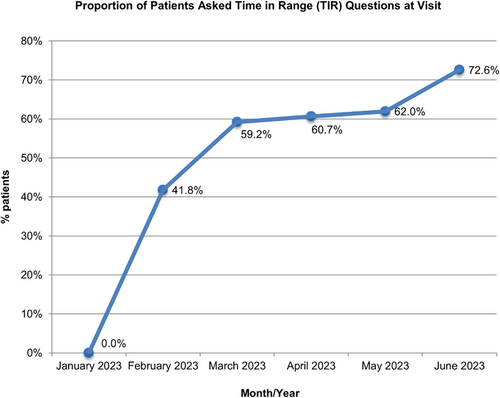
Background: The American Diabetes Association (ADA) guidelines for management of type 1 diabetes (T1D) recommend targeting time in range (TIR) ≥70% (blood sugars between 70 and 180 mg/dL) along with <4% time in hypoglycemia (below 70 mg/dL) as optimizing TIR reduces microvascular complications of diabetes. The overall aim of this project is to improve TIR among our patients using a continuous glucose monitor (CGM) by increasing point-of-care TIR education at quarterly clinic visits from 0% to 95% over 12 months.
Methods: Our interdisciplinary quality improvement team identified a knowledge gap among our patients related to TIR goals. Through several plan-do-study-act (PDSA) cycles, we created and tested a patient/family education handout, an electronic health record (EHR) SmartPhrase that can be included in after-visit instructions, and questions about TIR goals with associated education in our EHR visit flowsheet, to standardize the process of discussing and documenting TIR goals, education, and patient/family knowledge about TIR. We are currently scaling these interventions across the division.
Results: Since beginning the project in January 2023, we have increased the proportion of patients with T1D we discussed TIR goals with from 0% to 72.6% (Figure 1). The median proportion of patients meeting TIR goals (≥70% in range) is 19.2%.
Conclusions: Developing patient education materials and standardizing documentation about TIR goals increased provider-patient discussions about TIR. During this short period, we have not yet seen a change in the proportion of patients who meet TIR goals, but we anticipate improvement over time with continued education interventions.
Abstract #17 Ongoing efforts for improving depression screening at a pediatric diabetes center
Jeniece Ilkowitz; Becky H. Lois; Kathryn Licciardello; Mary Pat Gallagher
Hassenfeld Children's Hospital at NYU, Pediatric Diabetes Center, New York, NY, USA
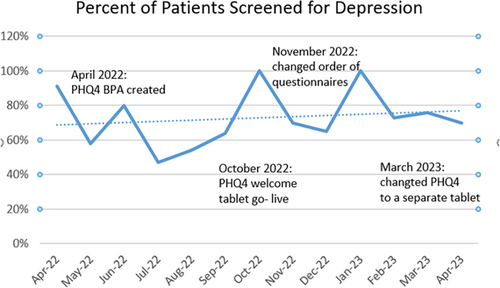
Background/Objective: In 2021, a Quality Improvement (QI) project began to increase rates of depression screening at a Pediatric Diabetes Center in NYC. Screening completion rates increased from 0% to 2% to 50% over 6 months. In this ongoing QI project, we aimed to show another 10% increase in screens completed from April 2022 to 2023 using Electronic Medical Record (EMR) features.
Methods: The PHQ-4 was utilized to assess depression and anxiety for patients 11 and older. Rates of screening were tracked monthly. Workflow initially included paper screens and provider input. In this QI initiative, multiple Plan-Do-Study-Act (PDSA) cycles were performed to optimize EMR integration. PDSA cycles included: creation of a best practice advisory; completion on Welcome tablet at check-in; and completion on a separate tablet for patients only.
Results: Following multiple PDSA cycles, the trend of screening completion rates continued to increase (Figure 1). Screening rates ranged from 65% to 100% in the last 6 months of QI work. After creating a patient facing PHQ-4 version administered by tablet at check in, a 100% screening rate was reported that month. When moved to a separate tablet, there was a decreased screening rate (70%).
Conclusions: EMR integration helped increase depression screening rates. Clinicians reported improvement in workflow. Future efforts should investigate reasons for decreased screening rates when a separate PHQ-4 tablet is used. Providing the PHQ-4 on a separate tablet to ensure the patient completed it (and not a caregiver), however change in the workflow initially decreased completion rates. Depression screening with EMR integration increased screening completion rates.
Abstract #18 Implementation of a school diabetes education and support program
Jeniece Ilkowitz; Christine Lally; Vanessa Wissing; Mary Pat Gallagher
Hassenfeld Children's Hospital at NYU, Pediatric Diabetes Center, New York, NY, USA
Background: Without diabetes education for school staff, diabetes management during the school day can interfere with a child's academic success and emotional well-being. The purpose of this quality improvement (QI) project was to increase school education sessions by 15% each year following the creation of a school education program at a NYC pediatric diabetes center.
Methods: Through the creation of a diabetes school liaison our center began establishing a diabetes in school program for schools attended by children at our center. School educational sessions were tracked and surveys, events, and ongoing program evaluations were done. Multiple Plan-Do-Act-Study (PDSA) cycles were performed and included: creation of a school liaison-specific email/phone, initiation of monthly zoom sessions, remote and in-person education sessions at individual schools, and a post-diagnosis school management class.
Results: In year one (2020–2021) of the program, 26 schools received individual in-person or remote diabetes education sessions, 35 sessions in 2021–2022 (38% increase) and 42 in 2022–2023 (17% increase). Survey responses showed 52.9% of the school professionals (27/51) reported they had limited education and understanding prior to education sessions regarding diabetes technology proficiency.
Conclusions: There is an unmet need for diabetes education for school educators and staff, and with ongoing support. Our findings show a program for school educators and staff was well received. Additionally, school nurses report a need for education on diabetes technology. Ongoing QI initiatives should continue to improve the education available to schools.
Keywords: Type 1 Diabetes, Type 2 Diabetes, Schools, Nursing, Quality Improvement
Abstract #19 The design of the electronic health record in type 1 diabetes centers: implications for metrics and data availability for a quality collaborative
Donna Eng
Helen Devos Children's Hospital, Grand Rapids, MI US
[email protected] and the team
Background/Objective: The optimal design of the Electronic Health Record (EHR) is critical for ensuring the quality and reliability to capture data and improve care and outcomes. We sought to describe EHR tools and workflows which contribute to core quality metrics in the T1DX Quality Improvement Collaborative (T1DX-QI).
Methods: We conducted interviews with 13 T1DX-QI centers about their EHR tools and clinic workflows.
Results: Thirteen centers had access to structured data tools, nine had access to patient questionnaires and two had integration with a device platform. There was significant variability in measure specification, tool use, and workflow, thus the number of available metrics per center ranged from 4 to 15. A greater number of centers had information about glycemic outcomes and diabetes technology use, but fewer centers had measurement of other self-management behaviors. Centers did capture patient reported outcomes including social determinants of health (n = 9), depression (n = 11), transition to adult care (n = 7) and diabetes distress (n = 3). A variety of stakeholders including diabetes providers, CDCESs, medical assistants, and quality improvement coordinators were responsible for capturing data. Centers that had a paired staffing model to support joint involvement of diabetes CDCESs in clinic encounters distributed the burden of data capture across the healthcare team, and was associated with a higher number available of data elements available.
Conclusions: Further work is needed to address the lack of standardization in EHR data elements, tools, and workflows, to support measurement and subsequently improved quality of care and outcomes for individuals with T1D.
Keywords: Electronic Health Record, quality improvement, type 1 diabetes, workflows, metrics
Abstract #20 Integrated diabetes education and support (IDEAS) program
Anna Neyman; Kathryn Haberlin-Pittz; Tamara Hannon
Indiana University School of Medicine, Indianapolis IN, USA
Background/Objective: To improve education and support for patients with post diabetes diagnosis DKA, we established the Integrated Diabetes Education and Support Program (IDEAS).
Methods: A multi-disciplinary team was assembled to co-design a structured in-person and virtual follow-up program including clinical, social, and health coaching services. 4 PDSA cycles have been completed. The statistical analysis was done with GraphPad Prism 9.5. A paired t-test was performed to assess HbA1c changes.
Results: A total of 14 youth were referred to IDEAS and 11 attended the initial IDEAS visit. Mean age 13.9 ± 1.8 years, 64% M, 57% white non-Hispanic, 36% black non-Hispanic, 7% Hispanic, 71% public insurance, 50% using CGM, 7% using an insulin pump, mean HbA1c 12.2 ± 2.5%. The most common etiology for DKA was insulin omission (85%). After improvements in scheduling, 100% of those referred to IDEAS attended (6/6). A total of seven participants had a repeat HbA1c ≥1 month (mean 3.1 ± 1.3 months) after baseline. There was a trend towards reduction in HbA1c (13.1% vs 10.8%, p = 0.16) (Figure 1). All participants consulted with a LMSW, 1 completed health coaching which was associated with a reduction in HbA1c (−1.9%). One participant had a history of 5 DKA episodes in the prior year and has had 1 DKA admission after enrolling in IDEAS. This participant has not been admitted to the hospital in past 4 months and HbA1c has decreased from 14.4% to 12.3%.
Conclusion: Youth with repeated episodes of DKA who have a standardized follow-up program with clinical, social, education, and health coaching support may have improvement in diabetes follow-up and outcomes.
Abstract #21 Establishing social determinants of health screening to improve pediatric diabetes patient outcomes
Blake Adams; Margaret Shepherd; Fatina Caldwell-Jones; Grace Nelson
University of Tennessee Health Science Center, Le Bonheur Children's Hospital, Memphis, TN USA
Background/Objective: Our mission at Le Bonheur Diabetes Clinic is to partner with families to aid them in finding the best ways to manage their children's diabetes. Patients with lower income and education levels have been shown to have worse glycemic outcomes. Despite this correlation between social factors and diabetes management, our clinic was not previously screening for Social Determinants of Health (SDOH) for people with type 1 and 2 diabetes (PWD). To address this disparity, we implemented SDOH screening for PWD with a goal to screen 10% of eligible PWD and offer resources and/or referrals to those who screened positive.
Methods: We met as a multidisciplinary team to establish screening parameters and partnered with the University of Michigan and utilized their “Partners in Care” survey. We implemented the survey and screened eligible PWD who had an A1C of 9.5%. Our social worker followed up with positive screens and provided resources based on individual family needs. Patients who screened positive for issues such as food insecurity, housing instability, transportation barriers, healthcare financial strain, and so forth, were referred and connected with appropriate resources.
Results: We successfully implemented SDOH screening for PWD. During our first two testing cycles, of the PWD who were eligible for screening, 59% completed screens. 50% of the completed screens were positive, and 81% of the PWD that screened positive were offered referrals to social workers and connected with appropriate resources.
Conclusions: Standardizing our SDOH clinic processes helped us increase screening rates and connect PWD to essential community resources.
Keywords: Social Determinants of Health, Health Equity
Abstract #22 Incorporating shared decision-making to facilitate equitable insulin pump use among pediatric patients with type 1 diabetes
Grace Nelson; Blake Adams
University of Tennessee Health Science Center, Le Bonheur Children's Hospital, Memphis, TN USA
Background: Technology use has improved outcomes for patients with T1D. However, race disparities exist. This was evident by the discrepancy in non-Hispanic Black patients (NHB) on insulin pumps (7%) versus non-Hispanic white patients (NHW) (21%) in our clinic. Our goal is to safely and equitably increase the number of patients using insulin pumps.
Methods: We identified a group of NHB patients who were not candidates for starting insulin pumps based on our clinic's “typical” practice but showed interest in pumps. After demonstrating efficacy and safety of pump use in this group, we expanded outreach. Beyond continued education for nurse educators and changing pump start criteria, we also used shared decision-making to ensure that all patients could regularly discuss technology use with their providers.
Results: As of December 2022, we have helped >35% of our interested patients navigate the process of obtaining insulin pumps. Equity was improved, with 22% of our NHB patients using pumps and 27% of NHW patients. Some of these patients would not previously be candidates for pumps but were able to safely begin using this technology because of these interventions.
Conclusions: Utilizing shared decision-making can help to identify patients who might not initially be considered for technology. We have demonstrated that many interested patients can safely initiate pumps which will help improve their diabetes management. We are continually adjusting our processes to improve equity in pump use and increase the number of patients utilizing pumps in our clinic.
Abstract #23 Appointment lag time and tracking transition in young adults
Sean DeLacey; Naomi Sullivan; Laura Levin; Naomi R. Fogel
Ann and Robert H. Lurie Children's Hospital of Chicago, Chicago, Illinois, USA
Background: Transfer from pediatric to adult providers is a sensitive time for Type 1 Diabetes care and is part of a transition process that should start early. If transition is not appropriately discussed, transfer of care is often frustrating for both patients and providers. Delay in transfer can lead to gaps in care and sub-optimal outcomes.
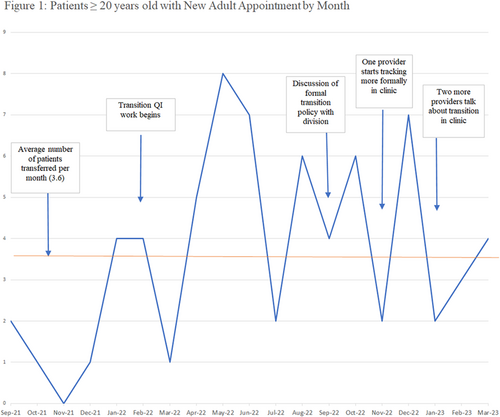
Methods: To improve transition of care we began quality improvement efforts, which included the development of a transition policy, recording of transition discussion in clinic, and tracking transfer within a patient registry including date of adult provider appointment. Data was collected via a diabetes registry between September 2021 and March 2023, with efforts to improve transition/transfer of patient care beginning in February 2022.
Results: As of March 2023, there were 186 patients ≥20 years old in the diabetes registry and 95 (51%) had transfer recorded, while 77 (41%) had confirmed appointments. The average time between last pediatric and first adult appointment was 4.72 months (standard deviation 3.26 months). Over time from 9/2021 to 3/2023 an average of 3.6 patients saw a new adult provider per month. In the 6 months before our efforts started, 12 patients had confirmed transfer and in the 6 months afterwards, 29 had confirmed transfer (Figure 1).
Conclusions: Starting to discuss transition in a structured way and the development of a transition policy led to an improvement in rates of transfer of care. Continued efforts will focus on patient skill development and facilitating transfer to decrease transfer lag time.
Abstract #24 Nationwide children's hospital (NCH) diabetes patient and family focus group program: A new initiative to incorporate the voice of the consumer
Toyetta Barnard-KirkW; Mary Joy Okafor; Amy Thompson; Alicia Clark; Don Buckingham; Justin Indyk; Malak Abdel-Hadi; Manmohan K. Kamboj
Nationwide Children's Hospital, Columbus, OH, USA
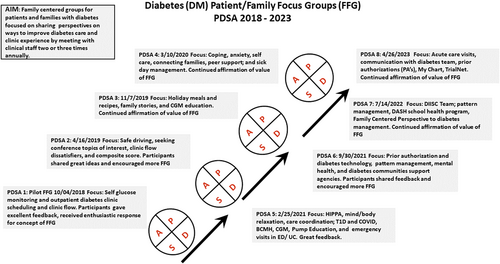
Objectives: Diabetes mellitus (DM) is a challenging chronic medical condition requiring active participation of patient/families in self-care. The objective of this project was to initiate family-centered groups for DM patients/families focused on sharing perspectives to improve diabetes management.
Methods: DM team members meet with patients/families 2–3 times annually with dinner provided. Agenda items are preplanned and topics that have been discussed thus far include but are not limited to diabetes daily management, sick day management, DM technologies, school diabetes resources, medical handicap/insurance, and psycho-social strategies and resources for coping with DM. Our groups encompass diversity in age, gender, ethnicity, race, socio-economic backgrounds, allowing for families to correlate their experiences with other families.
Results: Session participation has demonstrated encouragement in a desire of patients/families to increase the use of technology for diabetes management, improve emotional support, develop coping mechanisms, decrease difficulty with social determinants of health, and improve health literacy. Additionally, this allowed the DM team to identify areas for practice change. Some of the feedback testimonials include: “I do not feel alone,” “Great to feel our feedback matters,” “We are all on different paths but still have some similarity”.
Abstract #25 Pre-visit diabetes device data capture
Edelina Cohen; Michael Natter; Lauren Golden
Center for Diabetes and Metabolic Health at NYU Langone Health New York, NY, USA
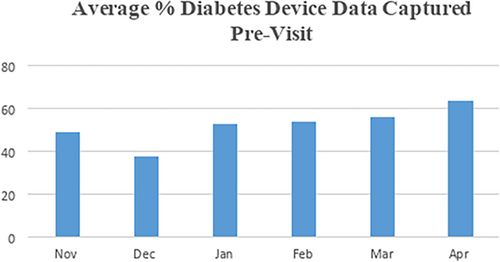
Background/Objective: Diabetes device data capture is essential for effective and efficient patient care. Our practice identified a deficit in pre-visit diabetes device data capture. To address this, strategies to improve pre-visit downloads/uploads (“data”) were implemented with the aim of increasing device data capture prior to patient visits.
Methods: The patient care coordinator (PCC) collected the glucose data prior to patient visits from November 2022 to mid-April 2023. A five-day notice was sent to patients via MyChart with instructions on how to download their diabetes device (continuous glucose monitor, meter, insulin pump, or smart pen) reports and upload as an attachment on MyChart, if not already linked to share their data with our practice. The PCC placed a follow up call 24–48 h prior to the patient's visit to remind them to download/upload their diabetes device data or link their device with the practice.
Results: Prior to intervention, approximate data capture was 43%. After intervention, data capture peaked at 65%, with an average of 52% over 24 weeks.
Conclusions: We attributed the increase in data capture to multi-modal reminders, patients' increased familiarity with the pre-visit diabetes device data process, and patients linking their devices to share with the practice. The pre-visit data capture enabled clinicians to tailor patient care and provide targeted diabetes care given they had the data needed to make clinical decisions. Future steps include assessing interventions to diabetes care after implementation of data capture.
Abstract #26 Improving depression screening in patients with type 1 diabetes mellitus
Siham Accacha, Danielle Alessio; Lori Benzoni; Sheila Dennehy; Ulka Kothari
Department of Pediatric Endocrinology, NYU Long Island School of Medicine, Mineola, NY, USA
Background/Objective: Depression is one of the most common mental illnesses among adolescents. Despite its higher prevalence in youth with type 1 diabetes (T1D), about 40% of pediatric patients are not recognized. The Patient Health Questionnaire 9 in adolescent (PHQ-9A), is a widely used, validated screener for depression.
Purpose: To improve recognition of depression in adolescents with T1D, age 11–17 years old, using PHQ9A from baseline of 0% to 75% from March to December of 2022.
Methods: We created a multidisciplinary team of physicians, RN, CDCES, medical assistants, and social workers.
Multiple PDSA cycles was conducted for education, folder for resources, algorithm, EMR changes, and referral to mental health.
Results: We used run charts to track our data. We improved our outcome measure of depression screening from baseline 0% to 75% over 9 months. We have now created a stable hardwired process for depression screening and referral with minimal variability as demonstrated by sustained improvement over the duration of project.
Conclusions: Multidisciplinary approach to chronic disease management is key to improving patient outcomes. Co-location of mental health provider helps facilitate timely screening, referral and follow up for patients with depression. Tracking data and ongoing PDSA cycles helped initiate and improve screening for depression in adolescent patients with T1D.
Keywords: Pediatrics, depression, screening
Abstract #27 To contract or not to contract? paying for NICH to address the social drivers of diabetes outcomes
Michael A. Harris; Samantha Barry-Menkhaus; Kim Spiro; Kristen Leadem; David V. Wagner
Oregon Health and Science University, Portland, Oregon, USA.
Background/Objective: NICH, or Novel Interventions in Children's Healthcare, addresses the barriers to care and access in young people living with diabetes who also experience a disproportionate amount of social burden. NICH has successfully secured contracts with insurers using data, demonstrating significant cost savings in youth experiencing the highest needs and highest risk. However, despite the compelling results around cost savings, NICH has not been uniformly adopted by insurers and healthcare institutions. The aim of the project was to identify key outcomes that drive contracting for NICH services for youth living with diabetes and high social risk.
Methods: We conducted a retrospective qualitative review of contracts with insurers for NICH services delivered to young people living with diabetes. We identified the most compelling outcomes that resulted in establishing contracts for NICH.
Results: The results of our retrospective review identified five distinct, but related outcomes that resulted in successful contracting for NICH; reducing costs and medical waste, improving care, improving health, improving provider experiences with care, and decreasing health disparities and inequities. In addition, we identified several barriers to contracting for NICH for youth with diabetes experiencing high cost, high needs, and high risk.
Conclusions: Despite data demonstrating the incredible cost savings of NICH, the uptake from both healthcare systems and insurers has been slow. To more successfully establish care for our most vulnerable youth living with diabetes, programs must be able to demonstrate value across several domains including savings, health outcomes, improved care, provider wellness and reducing disparities.
Keywords: Diabetes, health disparities, social drivers of health
Abstract #28 Improving food insecurity screening in children and adolescents with type 1 and type 2 diabetes
Jennifer Ruiz1; Jeannie S. Huang1,2; Jacob Parker1; Yesenia Parker1; Anna Cymbaluk1,2; Christy Byer-Mendoza1; Kim McNamara1; Andrea Huber1; Carla Demeterco-Berggren1,2
1Rady Children's Hospital, San Diego, 2University of California, San Diego San Diego, California, USA
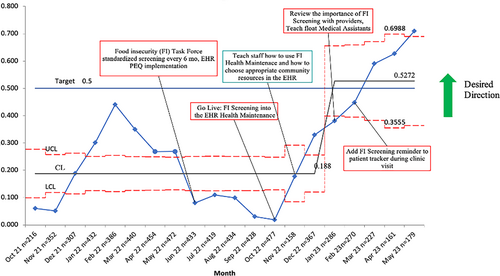
Background/Objective: Families raising a child with diabetes face higher health care costs and are more likely to be food insecure. We embarked on a Quality Improvement (QI) project to increase the percentage of youth with diabetes screened for food insecurity (FI) and provided FI resources from 27% to 50% in 12 months.
Methods: Rady Children's Hospital, San Diego (RCHSD) uses the Hunger Vital Sign™ tool for food insecurity screening (FIS). A care gap checklist identifies patients due for FIS and an electronic medical record (EMR) data dashboard tracks rate of FIS performance and whether FI resources are provided. A multidisciplinary team identified key change targets for interventions which were tested in several Plan-Do-Study-Act cycles. Interventions included: standardizing FIS performance at six-month intervals, automating assignment of patient-entered questionnaires (PEQ) in English and Spanish to clinical encounters, training providers and staff regarding FIS protocols, using a patient clinic tracker to ensure performance of FIS, and EMR documentation of FI resource provision.
Results: As of May 2023, the percentage of youth with diabetes screened for food insecurity and provided with resources increased by 44% from May 2022 baseline of 27%–71% (exceeding our goal of 50%) Figure 1.
Conclusions: Application of QI methodology enabled improved FIS rates at our diabetes center. Utilizing EMR tools and data collection enabled automation to help standardize FIS protocols and FIS data tracking. FIS success can be potentiated by the EMR.
Abstract #29 Increasing insulin pump utilization in public insured patients
Anna Cymbaluk1,2, Christy Byer-Mendoza1N; Kim McNamara1; Andrea Huber1; Carla Demeterco-Berggren1,2
1Rady Children's Hospital, San Diego, 2University of California, San Diego San Diego, California, USA
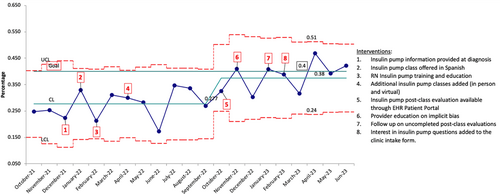
Background/Objective: Diabetes technology use is associated with improved type 1 diabetes (T1D) outcomes. American youth with public insurance, often used as a proxy for lower socioeconomic status, use less diabetes technology. We executed a Quality Improvement (QI) project to increase the percentage of public insured patients with T1D using an insulin pump from 30% to 40% in 15 months.
Methods: A T1D data dashboard within the electronic health record (EHR) allowed our team to identify the percentage of public insured patients with T1D seen in diabetes clinic using an insulin pump. A multidisciplinary team identified key change concepts. These were tested in a series of PDSA cycles. Interventions included: offering virtual pump education, providing pump education with Spanish translation, adding additional classes, educating providers regarding implicit bias, increasing patient access to pump information material, and including questions about interest in insulin pump on the clinic intake form.
Results: As of June 2023, the percentage of public insured children with T1D utilizing an insulin pump increased from 30% in April 2022 to 42% in June 2023 (exceeding our goal of 40%); (Figure 1.)
Conclusions: Continued follow-up of this population will help identify barriers to insulin pump access and the interventions with the most impact. New strategies to address inequities and improve technology use in TID are needed.
Abstract #30 Using quality improvement to reduce loss-to-follow-up in pediatric patients with type 1 diabetes
Meenal Gupta*, Yasi Mohsenian, Alissa Roberts, Faisal Malik
*Seattle Children's Hospital/University of Washington, Seattle, WA, USA
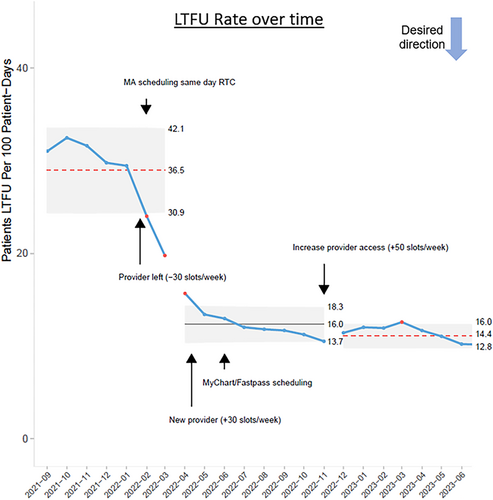
Background/Objective: Regular ambulatory diabetes clinic visits offer opportunities for individualized education and development of tailored treatment plans to support the management of type 1 diabetes (T1D). Higher rates of clinic visit attendance is associated with lower HbA1c levels. We aimed to reduce the mean loss-to-follow-up (LTFU) rate for our pediatric patients with T1D to 20% from a baseline of approximately 35% in 18 months.
Methods: A multidisciplinary team developed and tested quality improvement (QI) interventions to improve clinic visit attendance: (1) Training medical assistants to schedule return-to-clinic appointments by the end of the patient's diabetes clinic visit; (2) Offering visit scheduling to patients via Epic MyChart and FastPass; the latter enabled patients with existing appointments to get on a waitlist for an earlier appointment; (3) Adding a new diabetes provider to our team to improve access and availability of clinic visit slots. LTFU was defined as having their last clinic visit >6 months ago. Several Plan-Do-Study-Act cycles were conducted for each intervention. Rates of LTFU were analyzed monthly via statistical process control charts (p-charts) to identify special cause variation.
Results: Our baseline LTFU rate was 35% (Figure). Following QI interventions, our LTFU rate demonstrated a downward trend beginning in October 2022 with eight out of the nine next data points below the mean. Special cause variation was identified in May and June 2023 with LTFU rates outside of the control limits.
Conclusion: By improving scheduling processes and visit access using QI methodology, we successfully reduced mean LTFU rate.
Abstract #31 Screening for social determinants of health in adults with diabetes
Ruth S. Weinstock1, Emilie Hess; Beth Wells; Jamie Romeiser
1SUNY Upstate Medical University, Syracuse NY, USA
Objective: To evaluate adults with type 1 (T1D) and type 2 (T2D) diabetes for social determinants of health (SDOH) and acceptance of social work (SW) referrals.
Methods: Food, housing, transportation insecurities and financial resource strain were assessed in adults with T1D and T2D from August 2022 to April 2023. If a need was identified, referral to SW was offered. Exploratory multivariable logistic regression was used to assess for predictors of positive SDOH screening and SW referral acceptance.
Results: Of 4704 adults with diabetes, 83.2% (n = 3912) were screened for SDOH (T1D n = 1434, T2D n = 2478). T1D vs T2D adults were younger (mean 41 vs 63 years), mostly White (90.0% vs 73.0%), and had more private insurance (57.9% vs 28.5%): all p < 0.0001. Overall, 13.4% T1D vs 16.0% T2D adults screened positive (p = 0.03); for food insecurity 5.4% vs 7.5% p = 0.01; transportation needs 3.8% vs 4.1% p = NS and financial resource strain 9.7% vs 11.4% p = NS. Adults who screened positive were more likely to be Black vs non-Hispanic White, the majority had >1 material need, and for T1D were more likely to have Medicaid/Medicare and less likely to be using an insulin pump. Of those who screened positive, 25.5% of T1D and 25.3% of T2D accepted SW referrals (p = NS). Those T2D who were White had lower odds of accepting SW referral. Every additional positive insecurity increased the odds of accepting SW referral (T1D OR = 1.39, T2D OR = 1.5).
Conclusions: Material needs are common in adults with diabetes. Interventions are needed to address these needs and improve diabetes care.
Keywords: Social determinants of health, type 1 diabetes, type 2 diabetes, social work
Abstract #32 Higher anxiety scores associated with glycemic outcomes
Margaret Gillis1; Emma Ospelt1; Saketh Rompicherla1; Ann Mungmode1; Nicole Rioles1; Alissa Roberts2; Caleb Schmid3; Tamara Hannon4; G. Todd Alonso5; Osagie Ebekozien1,6
1T1D Exchange, Boston, MA, USA; 2Seattle Children's Hospital, Seattle, WA, USA; 3Oregon Health and Sciences University, Portland, OR, USA; 4University of Indiana School of Medicine, Indianapolis, IN, USA; 5University of Colorado, Barbara Davis Center, Aurora, CO, USA; 6University of Mississippi School of Population Health, Jackson, T1D Exchange, Boston, Massachusetts, USA
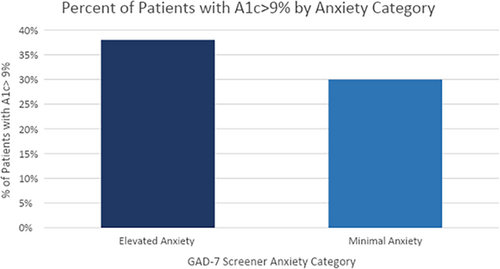
Background/Objective: The goal of this study was to look at how anxiety may impact A1c levels. The GAD-7 is a seven-question anxiety screener scored from 0 to 21. These scores are broken down into four categories: minimal, mild, moderate, and severe. For this analysis, we combine mild, moderate, and severe.1
Methods: This study analyzed EMR data from patients who completed the GAD-7 screener from April 2017 to June 2023. The population of interest consisted of 693 patients from 9 clinics between 12 and 75 years. We combined anxiety categories mild to severe as elevated anxiety levels and compared that to minimal anxiety with chi-square or fisher exact tests. The anxiety levels were analyzed into subcategories to compare based on gender, race/ethnicity, insurance type, and A1c outcomes.2 Similar analysis was performed on the population with A1c > 9%.
Results: There was a significant difference (p = 0.04) between individuals with A1c > 9%, 38% in the elevated anxiety group and 30% in the minimal anxiety group (Figure). In the A1c > 9% group, there was a significantly higher (p = 0.004) female population in the elevated group at 66% compared to the minimal group at 48%. There were no significant differences found in race/ethnicity or insurance type.
Conclusions: This data shows elevated anxiety has a higher percentage of its population with A1c > 9%. In addition, within the population with A1c > 9%, a significantly higher percentage of females have elevated anxiety levels.
Keywords: Anxiety, Glycated Hemoglobin, Patient Health Questionnaire
- Sapra A, Bhandari P, Sharma S, Chanpura T, Lopp L. Using generalized anxiety disorder-2 (GAD-2) and GAD-7 in a primary care setting. Cureus. 2020 12(5):e8224. doi: 10.7759/cureus.8224
- Herzer M, Hood KK. Anxiety symptoms in adolescents with type 1 diabetes: association with blood glucose monitoring and glycemic control. J Pediatr Psychol. 2010 35(4):415–425. doi: 10.1093/jpepsy/jsp063
Abstract #33 Increasing documented transition plans across three sites in the T1D exchange learning collaborative
Trevon Wright1; Ori Odugbesan1; Donna S. Eng2; Britni A. Schipper3; Jeniece Ilkowitz4; Emily Dewit5; Osagie Ebekozien1,6
1T1D Exchange; 2Spectrum Health, Helen Devos; 3NYU Langone; 4Children's Mercy Hospital T1D Exchange, Inc. Boston, Massachusetts, USA
Background: Transition planning improves the quality of care for adolescents and young adults living with type 1 diabetes (T1D) as they move from pediatric to adult diabetes healthcare providers. Our aim was to increase documented transition planning at sites in the T1D Exchange Quality Improvement Collaborative (T1DX-QI).
- Each provider was paired with a Medical Assistant (MA) and a CDCES. In this process, the MA identifies and flags patients eligible for READDY assessment. Integrated the READDY tool into the Electronic Medical Record.
- Utilized RedCap to generate a QR code to send to patients ahead of visit.
- Collaborated with adult clinics to discuss use of the READDY assessment.
- Use of a multidisciplinary team approach including dieticians, social workers, CDCES, and providers and reviewing reports at least quarterly.
Abstract #34 Engaging people with diabetes in quality improvement clinical projects: Insights from the T1D exchange quality improvement collaborative
Nicole Rioles1,2, Holly Hardison1,2, Margaret Gillis1, Amy Ohmer2, Marissa Town2,3, Neilly Ricketts2,4, Britaney Spartz2,5, Amy Grant6, Jeniece Ilkowitz2,7, and Osagie Ebekozien1,8
1T1D Exchange, 2T1D Exchange PPAC, 3Children With Diabetes, 4NYU Langone, 5Children's Mercy Hospital, 6Cincinnati Children's Hospital Medical Center, 7Hassenfeld Children's Hospital at NYU Langone, 8University of Mississippi School of Population Health, Jackson
Background: Engaging People with Diabetes (PWD) in clinical care can lead to improved processes, but there are challenges in how to effectively engage them. T1D Exchange Quality Improvement Collaborative (T1DX-QI) wanted to learn from its member clinics that are collaborating with PWD to gain insights into how we can support stakeholder engagement (SE) in more clinical centers.
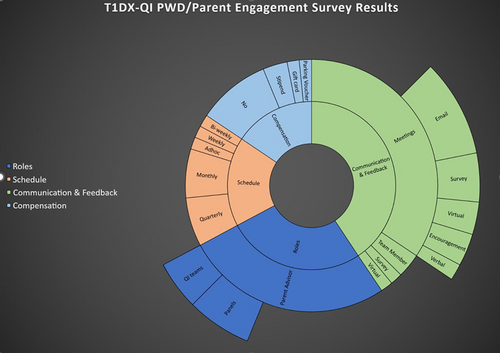
Methods: In 2022, T1DX-QI surveyed 11 clinics with active PWD stakeholders to learn about their approaches. T1DX-QI asked additional survey questions to eight clinics that responded asking how they include PWD in their quality improvement work and how they communicate, elicit feedback, and collaborate.
Results: Of the eight that responded to additional SE survey questions; all had at least one PWD advisor engaged with their team; four (50%) had PWD advisory panels; and four (50%) invited PWD to join QI process teams. Stakeholders were a heterogenous range of PWD including adolescents, young adults, and older adults as well as parents. Eight clinics engage PWD in meetings; seven (88%) used surveys and/or email; and two (25%) reported that their PWD advisors were “part of the team.” Four clinics (50%) offered compensation using stipends or gift cards. Two clinics (25%) provided food and/or parking vouchers. Figure 1 shows how the clinics engage PWD in their multidisciplinary teams.
Abstract #35 Leveraging EMR data to enable remote patient monitoring in the ROCKET T1D program
Daniel J. DeSalvo; Rona Sonabend; David D. Schwartz; Kelly Timmons; Sarah Lyons
Baylor College of Medicine/Texas Children's Hospital, Houston, TX, USA
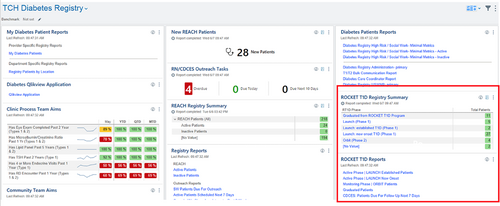
Background/Objective: ROCKET T1D (Remote Outreach & Care for Kids' Empowerment and Technology use in T1D) is a remote patient monitoring (RPM) program at Texas Children's Hospital supported by diabetes educators. ROCKET T1D includes a proactive “Launch Phase” with frequent virtual touchpoints for education and insulin therapy adjustments over a 1–3 month period, followed by an “Orbit Phase” with monthly data review and therapy adjustments over 3–6 months.
Methods: We developed an Epic EMR-based diabetes registry with reports to enable visualization of a validated diabetes ketoacidosis (DKA) risk score and clinical data (e.g., pump/CGM use, HbA1C, etc.) to quickly assess clinical progress and facilitate targeted outreach. Patients are added to the ROCKET T1D registry via a flowsheet entry, which allows visualization of progress through the Launch and Orbit Phases in the dashboard. We have incorporated weekly ROCKET T1D Mission Control meetings and utilize Glooko Population Health tracker to access remote data on-demand as interactive reports to facilitate insulin adjustments.
Results: The ROCKET T1D RPM program went live in October 2022 with an initial target population of patients with established T1D with moderate-to-high risk for DKA, recent hospitalization, and/or starting new diabetes devices. In April 2023, we expanded the program to include new onset T1D patients, and as of May 2023, we have enrolled ~30 new onset patients.
Conclusion: Inclusion of new onset T1D patients will enable proactive outreach at a pivotal time in the diabetes journey, with goals of optimizing diabetes self-management habits and glycemic outcomes.
Abstract #36 REACH registry: Using electronic medical record-based tools to improve outreach services
Selorm Dei-Tutu, Rebecca Butler, Amelia Martinez, Kelly Timmons, Meghan Craven
Baylor College of Medicine/Texas Children's Hospital, Houston, TX, USA
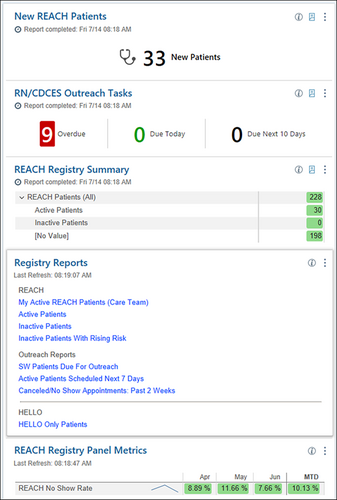
Background/Objectives: Supporting children who are at high risk of diabetes ketoacidosis (DKA) and other complications of Type 1 Diabetes (T1D) is a core goal of our diabetes program. Currently, children are identified using a custom risk score for DKA. A social worker and nurse team provide extra services to these children. Work was previously organized on spreadsheets; however, this limited the ease of tracking patients, sharing information, and gathering data. We aimed to leverage electronic medical record tools to facilitate this work.
Methods: We developed an EPIC EMR based registry, a custom intake form and dashboard to facilitate our work with the REACH (REsources And Care to improve Health outcomes) cohort. Variables, which populate the registry, include a custom DKA risk score and number of DKA events in the past year. The work the nurse and social worker do is documented in the intake form, including reminders for follow-up, which then populate the dashboard.
Results: The EPIC EMR based registry and documentation tools were debuted in April 2023 at the main campus. There are currently 30 active patients in the REACH cohort. Having a specific documentation template has streamlined documentation and enhanced reporting capabilities.
Conclusions: Creating an EPIC EMR based registry and documentation template streamlines workflow aimed at improving the care of children at high-risk of adverse events from T1D. Next steps include expanding workflow to satellite campuses.
Abstract #37 Improving diabetes self-management habits with remote patient monitoring in the ROCKET T1D program
Guido Alarcon; Don Buckingham; Rona Sonabend; David D. Schwartz; Sarah Lyons; Daniel J. DeSalvo
Baylor College of Medicine/Texas Children's Hospital, Houston, TX, USA
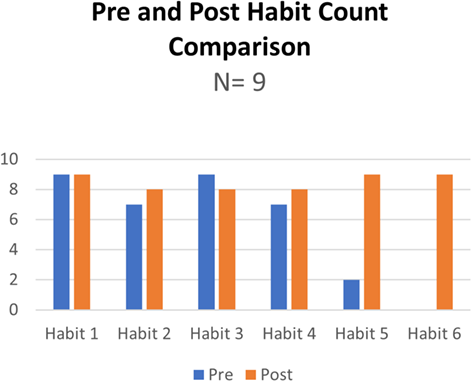
Background/Objective: Performing the 6 diabetes self-management habits to optimize glucose monitoring, insulin delivery, and use of diabetes data has been associated with lower HbA1c and increased time in range (Lee, 2021). We developed the ROCKET T1D (Remote Outreach & Care for Kids' Empowerment and Technology use in T1D) remote patient monitoring program to optimize diabetes management. We aimed to increase the use of the 6 diabetes self-management habits by at least 2 habits from baseline in >80% of youth with T1D enrolled in the initial “Launch phase”, which focuses on tailored support provided by Certified Diabetes Care and Education Specialists (CDCESs).
Methods: Youth enrolled in the ROCKET T1D program have a baseline assessment of the 6 habits, tracked by CDCES EMR-based flowsheet entry, and have weekly virtual visits using a “flight manual” with educational resources pertaining to each habit to target gap areas. Upon completion of the 1 to 3-month Launch Phase, the 6 Habits are reassessed and recorded via flowsheet.
Results: To date, 36 patients have entered the Launch Phase and 9 patients with established T1D have completed the program. Upon completion, the mean cumulative habit score increased from 3.7 to 5.7, and 100% of patients increased their habit score by at least 2 habits from baseline. The most substantial increases were in habit 5 (reviewing data) and 6 (adjusting insulin dose).
Conclusion: Providing remote, tailored support to families of youth with T1D is effective in improving diabetes self-management habits, which should lead to improved clinical outcomes.
Keywords: Diabetes Self-management education (DSME), Electronic Medical Record (EMR), Remote Patient Monitoring (RPM), Type 1 Diabetes
Reference:
Abstract #38 Improving diabetes retinopathy screening and documentation in youth with diabetes
Isabella Niu*; Fatema S. Abdulhussein*; Priya Srivastava; Tina Y. Hu; Barbara Liepman; Jenise C. Wong
*Co-first authors
Division of Endocrinology, Department of Pediatrics, University of California, San Francisco, San Francisco, CA, USA
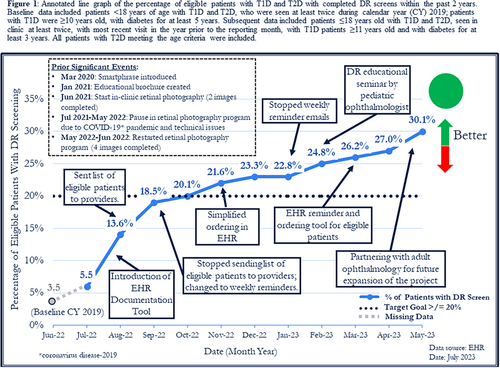
Background/Objective: Despite practice guidelines recommending screening for diabetes retinopathy (DR), pediatric screening rates remain low. In 2019, the DR screening rate of children with type 1 (T1D) and type 2 diabetes (T2D) δ18 years seen at UCSF Benioff Children's Hospital San Francisco Pediatric Diabetes Clinic was 3.5%. Our goal was to increase the DR screening rate to ε20% by June 2023.
Methods: We assessed barriers and root causes for low DR screening rates using quality improvement methodology and identified three areas of focus: (1) set up a non-mydriatic retinal camera in the pediatric diabetes clinic, (2) educate patients and diabetes providers about DR, and (3) improve DR screening documentation in the electronic health record (EHR).
Results: A teleretinal screening protocol was developed by a multidisciplinary team of endocrinologists, ophthalmologists, information technology analysts, medical assistants, and clinic administrators, using an in-clinic retinal camera. An educational brochure including DR screening was created for patients, a Smartphrase was developed for providers, and a DR seminar was presented to providers by pediatric ophthalmology. New EHR tools included a flowsheet with a dedicated field for documentation of external retinal exams and a reminder tool showing when eligible patients are due for retinal exams linked to EHR orders. Eligible patients who completed DR screenings increased to 30.1% by May 2023.
Conclusions: Access to DR screening in clinic, education of patients and providers, and improving data collection and EHR tools increased DR screening rates. Future interventions will expand screening to adults and further reduce barriers to screening.
Abstract #39 Advancing equity in technology usage for patients with diabetes
Janine Sanchez; Veronica Figueredo; Mariaester Makacio Morillo; Mariana Nunez Stosic; Patricia Gomez
University of Miami/Jackson Memorial Hospital, Miami, Florida, USA
Background/Objective: Technology has had a profound benefit in the management of patients with T1D. Despite the availability of technology through most third-party payers, racial and ethnic disparities have been reported.
Methods: In our pediatric T1D clinic, approximately half of our patients are Hispanic or Black. Half of our patients are insured by Medicaid. We found disparities in technology use with greater utilization among white patients. To rectify this, we introduced a protocol designed to ensure that all our patients receive advantages of technology. All patients were prescribed glucose sensors at diagnosis. Established patients who did not use a sensor were strongly encouraged to use one with sensor placement at the visit. Smart pen usage was recommended for all patients soon after diagnosis. Insulin pump was encouraged 6 months after diagnosis for patients proficient in carbohydrate counting.
Results: Since the protocol introduction, 95% of our patients with T1D use a glucose sensor and 53% use an insulin pump. Transition to a greater use of technology was facilitated by directly addressing patient concerns about visibility of devices and out of pocket expenses. We also found an easier transition to technology when our team helped patients navigate dealing with insurance, pharmacies, and schools.
Conclusion: Transition to a greater use of technology can be facilitated when there is a strong emphasis on its use at the time of diagnosis and at each visit. Anticipating and addressing all the patients' concerns also plays an important role in the transition to greater technology use.
Keywords: Barriers, health disparities, technology use, type 1 diabetes
Abstract #40 Identifying barriers for smart insulin pen connectivity in patients with poor glycemic outcomes
Veronica Figueredo1; Ori Odugbesan2, Janine Sanchez1
1Jackson Memorial Hospital, University of Miami, Miami, Florida, USA; 2T1D Exchange, Boston, Massachusetts, USA
Objective: Smart insulin pens (SIPs) offer remote monitoring capability with the potential to improve glycemic management and outcomes. This project aimed to identify barriers for successful SIPs sharing data with medical providers in our high-risk patients with T1D.
Methods: We identified patients using SIPs with A1c >8%. We reviewed how often patients were sharing SIPs reports between visits compared with our recommendation to send monthly. Interventions were tested in several PDSA cycles include: reminders during visits, follow up CDE visits, questionnaire to screen for data sharing barriers.
Results: We identified 29 patients with A1c >8%. 43% of these patients shared reports monthly as recommended. Twenty-one families completed SIP questionnaire. Seven patients with A1c >12% were selected to meet with CDE, 43% missed visit. All patients reported they knew how to share report but not all patients were reporting data. 33% use SIP to calculate dose but forget to save, 24% only use SIP occasionally, 19% forget to refresh report before sending, 19% lost SIP or said SIP not working, 10% embarrassed to share data, 5% not interested in sharing data with doctor or parents. 24% reported no problems.
Conclusion: We learned that reminding patients at visits about sending reports or scheduling CDE visits was not sufficient. We identified specific difficulties patients were experiencing and addressed barriers during visits. Longer follow up is needed to determine if addressing barriers will facilitate data transmission between clinic visits and improvement in glucose management.
Keywords: Barriers, Smart Insulin pen, T1D
Abstract #41 Increasing pump therapy adoption in patients with type 1 diabetes
Allison Smego1; Fadi Asfour2; Janet Sirstins3, Corinne Loizos3, Megan CounterW3, Billie Whitaker3, Stacey Bjerregaard2, Tina Wadhwa2, LeAnn Gubler3, Vandana Raman1
1Division of Endocrinology, University of Utah, Salt Lake City, UT, USA; 2Primary Children's Hospital; 3Primary Children's Hospital Pediatrics Diabetes Program
Background: Insulin pump therapy improves glycemic outcomes and quality of life in pediatric patients with type 1 diabetes (T1D). As a center with relatively high insulin pump utilization, we aimed to further increase pump adoption among our patients to improve glycemic outcomes.
Methods: This quality improvement project was conducted in a large, pediatric diabetes center by a multidisciplinary team of clinicians, educators, a social worker, a medical assistant, and a parent advocate. Quality improvement methodology informed the design and iterative testing of interventions including removing clinic-imposed barriers to pump initiation, improving access to pump education, assessing patient barriers to pump therapy, and improving staff knowledge about pump therapy.
Results: Baseline data from January to July 2022 revealed that 69.6% of our patients with T1D utilized insulin pump therapy. We worked to disseminate a new pump introduction self-learning packet and virtual pump classes. After PDSA cycles, the percentage of eligible patients receiving this information increased from 32% in January 2023 to 60.7% in June 2023. The percentage of insulin pump users in our clinic increased to 81.1% by June 2023.
Conclusion: Adapting our pump process to a more patient and family-centered approach has helped to increase the percentage of patients adopting pump therapy.
Abstract #42 Implementing patient-reported intake forms to integrate clinic efficiency with patient-centered care
Rachel Fenske1,2, Whitney N. Beaton1, M. Tracy Bekx1, Elizabeth A. Mann1
1University of Wisconsin—School of Medicine and Public Health, UW Health Kids, Madison, Wisconsin, USA; 2Department of Clinical Nutrition, UW Health, Madison, Wisconsin, USA
Background/Objective: Patient-centered care and education in pediatric diabetes clinics requires significant data collection and synthesis. Currently, Registered Nurses (RNs) are responsible for gathering this data from patients, documenting it in the electronic medical record, and from this, identifying priority topics to address. To mitigate potential team bias, accurately capture patient/family visit priorities, while increasing clinic efficiency, we proposed use of a patient-reported intake form (PRIF).
Methods: A single page, double-sided PRIF was developed to gather clinical and diabetes self-management data previously collected verbally by RNs. Two open-ended, goal-setting questions were included to allow patients/families to identify visit priorities. Patients/families were provided the PRIF at check-in and asked to complete it prior to rooming. Qualitative feedback from both clinic staff and patient/families were gathered and PRIFs were reviewed.
Results: In total, 45 patients/families completed PRIFs from April to May 2023. On average, 82% of the PRIF was completed. ~40% of patients completed the 2 open-ended questions about visit priorities. Common priorities noted by families included diabetes technology and blood sugar pattern review. RNs reported PRIFs allowed for more focused educational time. Patients/families reported appreciating the opportunity to mentally plan for the visit while completing the form and found the new workflow acceptable.
Conclusions: Use of a PRIF in pediatric diabetes clinic visits was acceptable by both team members and patients/families, and increased RN-reported efficiency. Offering prompts for open-ended goal setting questions may increase response rate and aid families in identifying visit priorities.
Keywords: Adolescent, Child, Patient-Centered Care, Type 1 Diabetes
Abstract #43 Transitioning children and adolescents with type 1 diabetes onto hybrid closed loop systems
Emily Coppedge; Isabel Reckson
Weill Cornell Medicine, New York, NY, USA
Background/Objective: In children and adolescents with Type 1 Diabetes (T1D), use of Hyrid Closed Loop Systems (HCLS) are associated with increased time in range (TIR), reductions in HbA1c, and decreased rates of hypoglycemia. To improve clinical outcomes, we implemented a quality improvement initiative to increase patients on HCLS.
Methods: Baseline data of patients with T1D on HCLS was obtained from August 2021 to February 2022. The initiative began in February 2022 with increased education on HCLS for both providers and patients. Patients were then trained and transitioned to HCLS by our team. Intervention data was collected from January to June 2023. Due to challenges with separating HCLS data, median HbA1c and TIR data was collected for all patients with T1D.
Results: The percentage of patients on pumps utilizing HCLS increased from 14% at baseline to 80% by June 2023. The median HbA1c at baseline data collection and during the intervention was 8.2% and 7.5%, respectively. Of patients wearing continuous glucose monitors, TIR above 50% improved from 40% to 51% during this time.
Conclusions: Our data shows a significant increase in HCLS across our practice from February 2022 to June 2023, with meaningful practice-wide improvements in HbA1c and TIR. We are associating this change in HbA1c and TIR with HCLS technology, as this was the only clinical intervention implemented during this period. Increasing access to and utilization of HCLS is integral to improving diabetes outcomes.
Keywords: Diabetes Mellitus Type 1, Insulin Infusion Systems, Glycated Hemoglobin A
Abstract #44 Patient involvement to improve new onset type 1 diabetes education
Isabel Reckson; Alyson Weiner; Elizabeth Gunckle
Weill Cornell Medicine, New York, NY, USA
Background/Objective: Little research exists examining the transition from inpatient to outpatient care, specifically for children and adolescents with recently diagnosed Type 1 Diabetes (T1D). Concerns arose in our clinic regarding inconsistent inpatient diabetes education and lack of family confidence upon discharge. We hypothesized a need for improved focus on the inpatient to outpatient transition for families with a child newly diagnosed with T1D.
Methods: Two Qualtrics surveys were developed and distributed to better understand knowledge gaps; one to the entire pediatric endocrinology division, and the other to families with a child diagnosed with T1D in the last 12 months. Both surveys assessed perceived challenges from the time of hospital admission to the first outpatient visit.
Results: Preliminary data shows discrepancies between patient and staff perspectives. The division members perceived educational gaps in the treatment of hypoglycemia, along with the timing and dosing of insulin for blood glucose corrections. While patients also listed timing and dosing of insulin as a key topic to be reinforced, there was also emphasis on carbohydrate counting and return to “day-to-day life.”
Conclusions: Survey data emphasizes the need for streamlined diabetes education, as well as the importance of patient involvement and perspective. Our team will continue to collect survey data to better understand topics of confusion and implement appropriate intervention. Next steps include developing diabetes educational videos, as well as a family focus group to involve families in diabetes practice initiatives and decisions.
Keywords: Diabetes Mellitus Type 1, Pediatrics, Patient Advocacy, Patient Discharge
Abstract #45 DiabetesWise Pro diabetes device digital platform
Korey K. Hood
Stanford University School of Medicine, Stanford, CA, USA; Stanford Diabetes Research Center, Stanford, CA, USA
Background: DiabetesWise Pro is a digital platform for healthcare professionals (HCPs) that aims to (1) increase Awareness about diabetes devices, (2) provide Education about matching devices to patient preferences and needs, and (3) simplify the Prescription process. The primary purpose of presenting at the November Learning Session of the T1D Exchange is to identify potential partners interested in testing DiabetesWise Pro in their clinical settings. Given the robust QI Collaborative, there may be opportunities to submit DiabetesWise Pro to the QI process to optimize its use in practice.
Methods: Both digital platforms are funded through grants from the Helmsley Charitable Trust, which allows DiabetesWise to be free, unbranded, and unbiased. DiabetesWise features a device check-up, device finder, wisdom, and other resources for people living with diabetes. The patient (or person) facing website launched in June 2019. DiabetesWise Pro was built and launched in February 2023.
Results: The features on the Pro website include a device library, comparison tools, myth-busting resources, and a prescription tool. The prescription tool is the core component of the Pro site that aims to simplify the prescription process for HCPs. Only 3 inputs are needed—device type, location, and insurance plan—to produce critical outputs which give HCPs access to coverage details, prior authorization forms, pharmacy/DME information, and policy documents for all FDA-approved devices.
Conclusions: This work has the potential to optimize diabetes device prescribing, enhance patient understanding and adherence, and ultimately improve diabetes management outcomes in real world primary care/family practice settings.
Keywords: DiabetesWise, diabetes devices, CGM, insulin pump, automated insulin delivery