Blockchain + Radiotherapy: The Scenarios of the 5G-Enabled Smart Radiotherapy Era
Abstract
In cancer radiotherapy (RT), each step can be digitalized, from CT simulation, planning, dose verification, and image guidance to treatment delivery. Therefore, RT may be the most digitized discipline in the field of internal medicine. Then, questions arise. What potential development opportunities does the development of network transmission technologies, such as blockchain and 5G, provide to promote the progress of tumor RT? What will the future of smart RT (SART) look like? The purpose of this article is to introduce briefly the main characteristics of blockchain and 5G transmission technologies and share ideas to imagine the “tomorrow” of smart RT, hoping to provide a more accurate, safe, and comfortable RT experience for patients in the future.
1 BLOCKCHAIN SUPPORTS CROSS-PLATFORM SAFE SHARING OF RADIOTHERAPY RESOURCES
1.1 Radiotherapy resources must be shared safely across platforms
RT has the characteristics of a long treatment course and re-irradiation on recurrence. Therefore, one patient may be treated at different RT centers. In particular, with the increasing application of proton, heavy ion, and boron neutron capture therapy, it may become a new standard for patients to receive particle treatment in different centers when undergoing recurrence. Taking head and neck tumors, for which proton RT has the most indications, as an example, the literature has shown that, despite continuous improvement in treatment levels, 15%–50% of patients with head and neck tumors still experience local recurrence.1, 2 Furthermore, a risk (as much as 40%) of secondary primary head and neck cancers exists among survivors because of an “in-field cancerization” of the upper aero-digestive tract,3 and these patients will need to receive particle RT.
Confronted with the aforementioned scenario, the typical approach entails the following steps. The RT department of the receiving hospital looks through the previous RT plan and understands the individual dose volume indicators of the targets and organs at risk through the two-dimensional dose volume histogram. In this method, it is difficult to display the dose 3D distribution fully and accurately, which impedes the formulation of a novel radiotherapeutic regimen. The precise replication of RT medical records necessitates a meticulous portrayal of the three-dimensional spatial allocation of the dose, accompanied by an exacting record of the executed fractionations. RT centers during medical alliances can employ cloud technology to achieve remote access and collaborative support for target delineation and planning. However, on the one hand, this initiative requires supplementary capital investment, and, on the other hand, it is limited to localized implementation within a limited scope by qualified and capable centers, which affects wider promotion. Alternatively, after packaging the images (with contours) and planning data from the previous RT course, they can be circulated through third-party servers, such as emails and network disks, and then downloaded and interpreted by the subsequent RT center. This is a feasible solution but also has the lowest level of data security. Upon transmitting the data onto the public network servers, it is difficult to guarantee that the data will not be destroyed, tampered with, or even lost, and the accuracy of the previous RT log records cannot be guaranteed. Furthermore, without authorization from the patient and the previous center, the patient data will not be downloaded on any station outside of the original treatment center.
1.2 Blockchain establishment for a secure transmission infrastructure
The concept of a blockchain was first proposed in 2008. It is an accounting technology jointly maintained by multiple parties and uses cryptography to ensure transmission and access security, thereby enabling consistent data storage, difficulty in tampering, and nonrepudiation prevention. This innovation is also referred to as “distributed ledger technology”.4 From a trading platform supporting virtual currency, it has gradually entered the v3.0 era, which covers all aspects of social life, and its applications are spread across various fields, such as justice, logistics, and medical care.5
According to the application scenarios, blockchains are usually divided into public and consortium blockchains, the latter of which is more suitable for the interconnection and data sharing of RT centers (alliance members). Therefore, based on the application scenario of the consortium blockchain, an example is proposed to illustrate how the blockchain works. Tom from the same village (alliance) borrowed money from Dick, which was recorded in the account book of the witness Harry as a transaction. In the future, once the account book is lost or broken by Tom and Harry, the existence and authenticity of the transaction cannot be verified. This is a disadvantage of the current data storage management model with single bookkeeping or central-node bookkeeping. For the same transaction, if Dick broadcast it to the entire village (all alliance member nodes) and asked the entire village to keep accounts together, data security would be considerably improved. Furthermore, all similar loan transactions among the villagers were recorded by several villagers diligently, and the ledgers of the villagers who did not take the initiative to record them were updated synchronously in a very short period, making it difficult to tamper with similar transactions. Even if Tom tampers with individual ledgers, it is very improbable for a significant proportion, exceeding 51% of the villagers' ledgers, to undergo alterations in a short period of time (as short as a few seconds).
The above example shows that the blockchain network architecture has the characteristics of single-point initiation, networkwide broadcasting, cross-checking, and collective bookkeeping for each transaction. The “transaction” here, placed in the scenario of safe sharing of RT data, is the record of “sending or receiving RT data behavior.”
1.3 Blockchain + radiotherapy
The blockchain used for RT data transmission between centers (alliance members) can be called a “radiotherapy consortium blockchain” (RTBC). On this platform, when patient P completes the first RT course at Hospital A and wishes to go to Hospital B for the secondary course, the workflow scene is as shown in Figure 1.
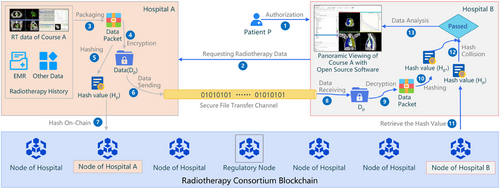
- Step I, establishment of business contact: (1) Patient P authorizes Hospital B to request his or her RT history data in Hospital A during a period of authorized time (during the RT course in B). (2) B sends the request to A through the RTBC's user interface (however, the request action is recorded in the blockchain as a transaction). After verifying the identity of B, A establishes a unique point-to-point channel with B.
- Step II, data sending: Hospital A sends Patient P's RT data (including images, RTStructure, RTPlan, RTDose, and fractionation) and medical record historical data to the blockchain platform following these steps: (3) packaging by formatting and encapsulation in a certain format, (4) encrypting the package with a public key, and (5) generating a unique hash value Hp for the encryption package. The “hash value” is the unique number string mapped by the hash function for a set of data, for which any character in this set of data is changed, and its corresponding hash value is compulsorily changed. Therefore, the hash value is a unique code for identifying whether data have changed. (6) The packaged and encrypted data DP are transmitted through the “file transfer layer”. (7) Meanwhile, the blockchain layer only transmits HP, the hash value of DP, ensuring the efficiency of the blockchain operation.
- Step III, data receiving: (8) Hospital B receives Patient P's data DP from the file transfer layer and (9) decrypts them into a data package with a private key authorized by P. (10) The hash value Hp* is created from the decrypted package. (11) The original Hp is read from the blockchain node. (12) Through hash collision, Hp* and Hp are compared to make sure the data transmission is secure without any tampering.
- Step IV, visualization: (13) After the hash collision, the package can be loaded by any open-source applications (such as 3DSlicer, a free open-source software platform for biomedical research) to show the panoramic viewing of Patient P's RT plan (including contours, field parameters, dose distribution, and DVHs) in Hospital A. Furthermore, to protect the ownership of the previous RT data, it may be withdrawn after being presented in order to avoid being downloaded by Hospital B.
The above scenario describes the data sharing model in the era of “blockchain + radiotherapy.” While ensuring security, this model is independent of commercial platforms and is more easily promoted among RT units. The above-mentioned RTBC and the expected “image chain,” which aims to share diagnostic images among centers, are pioneering theories for the application of block chain technology in the medical field, which benefits patients, facilitates medical resource sharing, and promotes the development of corresponding industries.
The possible problems and difficulties encountered in the implementation and promotion of the RTBC may be related to the discipline of network connections from different centers. Intercenter data transmission may require the blockchain nodes to be connected via the Internet. To ensure the safety of the RT area network in each center, bastion host can be enrolled to meet the requirements and used to separate the internal RT area network from the public transmission network.
2 5G EMPOWERS THE SMART RADIOTHERAPY SCENE WITH THE “INTERNET OF EVERYTHING”
2.1 5G network empowers the Internet of everything
The 5G network is the fifth-generation mobile communication network. Its transmission speed is more than 10 times that of the 4G network. Notably, its connection density (the number of nodes that can access the Internet in a unit space) is 100 times higher than that of a 4G network, which provides technical support for the Internet of Things (IoT) era of the Internet of Everything.
The concept of the IoT was formally proposed by the International Telecommunication Union6 in 2005. It encompasses the real-time aggregation of data from objects or processes that require monitoring, connectivity, and interaction. This aggregation is facilitated by a spectrum of devices and technologies, including information sensors, radio frequency identification systems, global positioning systems, infrared sensors, and laser scanners. This comprehensive data gathering spans diverse informational facets, encompassing sound, light, heat, electricity, mechanics, chemistry, biology, and geographical location. By leveraging an array of potential network entry points, it achieves an all-encompassing interconnection between entities and individuals, thereby enabling the intelligent perception, recognition, and management of objects and processes.
2.2 Interconnectivity of all things in the radiotherapy scenario
Within the context of RT regimens, a multitude of devices involved in treatment can be interconnected, including imaging equipment, treatment planning systems, linear accelerators (LINACs), and particle therapy systems, as well as peripheral devices such as lasers, image guidance systems, optical positioning systems, respiratory motion management systems, and quality control measures. Even elements within the treatment room, such as brightness, background music, height of treatment beds, and immobilization devices, can be interconnected to establish a “local-area web of things” for RT clinical practice. To meet the patient's requirement between centers, the web of things can be interconnected to be IoTs through blockchain technology. This interconnection, built upon secure data transmission, enables alliance members to cooperate deeply, including in patient referrals, remote medical consultations, multi-diciplinary team conferences, and remote equipment quality control.
- • Establishing a Private Cloud for Digital Twins: During the RT course in Hospital A, when the monitoring system in the treatment room captures the entrance of Patient P at each fraction, the intelligent system records all the treatment parameters for this patient, including images, plans, image-guided radiotherapy (IGRT) online images, couch shifts, couch position and angles, treatment execution dynamic log files, and even the environment light and background music. All the parameters are bound together with P's facial features and are used to establish a personalized model for P. Subsequently, this model is encapsulated in a formatted and encrypted manner as a data entity, Dp, and then saved in P's private cloud Cp.
- • Different Centers with Familiar Treatment Scenarios: When Patient P decides to have another RT course in Hospital B with P's authorization, B securely accesses Cp and downloads the personalized data entity Dp from P's private cloud through the blockchain platform. Referring to Dp, B designs a P-specific treatment scheme for his or her subsequent course. When P walks into B's RT treatment room again, B's instant monitoring system captures P's entrance. Then, the familiar environment lighting, background music, suitable bed height, specific immobilization device, and initial bed settlement value—all P-specific preferences—are automatically initiated and loaded.
In these scenarios, with the help of the IoT and digital twin technology, the equipment in the RT process has become the “external organs” of the patient. It not only creates a “warm” smart RT scene for patients, improves the patient's RT experience, and relieves the fear of pediatric RT patients, but it also substantially reduces the risk of human errors by technicians, provides truly individually customized RT, and promotes each center to achieve standardization and homogeneity.
2.3 AI+AR-driven smart radiation therapy
Artificial Intelligence (AI) has introduced an elevated focus on the quality of RT. The adoption of AI-driven processes, such as automatic target delineation,7 organ delineation,8 treatment planning,9 and AI-based automated physics quality control,10 has progressively played a significant role in the field of RT. These applications free clinicians and physicists from repetitive tasks, enabling them to redirect their efforts toward scrutinizing AI-generated outcomes, ensuring precision through quality control, and providing personalized patient care. As a result, it can reduce human error, compensate for the lack of experience of low-seniority personnel, and heighten standardization across primary RT facilities11.
Furthermore, in cases where the anatomical structures, such as the centers of growth in the pediatric skeleton12 and hippocampal tissues,13 are anatomically difficult to distinguish and conventional methods struggle to outline and evaluate these challenging organs, AI-assisted delineation can offer more tissue sparing, enhance patient quality of life, and subsequently elevate the benefits of RT.
Augmented Reality (AR) makes it possible to make visible X-rays strike visible tumors. AR technology connects a wearable device (AR glasses) to the private cloud of each patient. After reading the patient's image, contours, and plan parameters from the private cloud, the personalized virtual character and all visible elements can be shown in the AR lens. When the AR equipment enters the RT room, the position of the accelerator's isocenter and the coordinates of the AR equipment can be bound together using the spatial coordinate positioning technology. From different angles and distances, anyone who takes the AR lens can see both real and virtual elements in the room, including the surrounding environment, the LINAC with the treatment couch, the virtual patient body with the tumor and surrounding organs, the virtual radiation plan beams, the virtual planned gantry rotating trail, and even the expected virtual in vivo dose distributions simultaneously14. Figure 2 shows a scene with AR glasses in the LINAC treatment room.
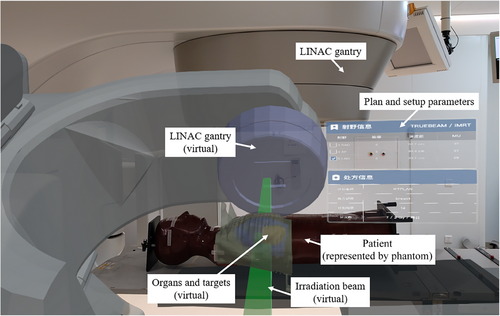
For patients, this technology can be used for first-time treatment education, improve patient compliance, and reduce children's fear of unfamiliar RT environments. For RT therapists, this technology can be used to identify incorrect immobilization facilities and patient positioning parameters to reduce artificial errors. For physicians, AR technology can be combined with voice transmission, electronic signatures, and other interactive functions for remote positioning and remote IGRT, which may reduce movements from inpatient wards to the treatment area while participating in the entire treatment course.
Based on the previously mentioned private cloud and AI+AR technologies, under the condition that the patient is authorized and conforms to the legal and ethical norms, the patient's anatomy (including static information, such as organ position and shape, and dynamic information, such as respiration and gastrointestinal peristalsis), physiology, biochemistry, metabolism, diagnosis, radiobiological effects, complications caused by previous treatment, and other information can all be described digitally by modeling. Thus, at different dimensions, a digital twin of the patient can be established, and the space in which it exists is “the metaverse.” It can be assumed that, after the level of digitalization and modeling gradually improves in the future, medical workers (such as RT physicians, physicists, and RT technicians) can interact with the patient's digital twin in this virtual space, simulate the benefits, risks, and rehabilitation processes brought to patients by different treatment schemes, and optimize treatment decisions to guide the treatment of patients in the real world, improve efficacy, and reduce risks.
In conclusion, the proliferation and application of innovative information technologies, such as blockchain, 5G, AI, and AR, have provided the field of RT with a more accessible and expansive platform for development. Given this opportunity, it is necessary to consider how to make good use of these new technologies and platforms in various research fields, such as basic, transformational, clinical, and physical technology, to promote the standardization and homogeneity of RT.
ACKNOWLEDGMENTS
This work was supported by the National Natural Science Foundation of China (82172072), Natural Science Foundation of Shandong Province, China (ZR2020LZL001), and Foundation of Taishan Scholars, China (tsqn201909140).
CONFLICTS OF INTEREST STATEMENT
The author declares no conflicts of interest.