Bronchoscopy in severe childhood asthma: Irresponsible or irreplaceable?
Megan N. Januska MD
Department of Pediatrics, Icahn School of Medicine at Mount Sinai, New York, New York
Search for more papers by this authorDavid L. Goldman MD
Department of Pediatrics, Children's Hospital at Montefiore, Bronx, New York
Search for more papers by this authorWilmore Webley PhD
Microbiology Department, University of Massachusetts Amherst, Amherst, Massachusetts
Search for more papers by this authorW. Gerald Teague MD
Department of Pediatrics, University of Virginia School of Medicine, Charlottesville, Virginia
Search for more papers by this authorRobyn T. Cohen MD
Boston University School of Medicine, Boston, Massachusetts
Search for more papers by this authorSupinda Bunyavanich MD
Department of Pediatrics, Icahn School of Medicine at Mount Sinai, New York, New York
Department of Genetics and Genomic Sciences, Ichan School of Medicine at Mount Sinai, New York, New York
Search for more papers by this authorCorresponding Author
Alfin G. Vicencio MD
Department of Pediatrics, Icahn School of Medicine at Mount Sinai, New York, New York
Correspondence Alfin G. Vicencio, Professor of Pediatrics, Mount Sinai Kravis Children's Hospital, Icahn School of Medicine at Mount Sinai, One Gustave L. Levy Place, #1202B, New York, NY 10029.
Email: [email protected]
Search for more papers by this authorMegan N. Januska MD
Department of Pediatrics, Icahn School of Medicine at Mount Sinai, New York, New York
Search for more papers by this authorDavid L. Goldman MD
Department of Pediatrics, Children's Hospital at Montefiore, Bronx, New York
Search for more papers by this authorWilmore Webley PhD
Microbiology Department, University of Massachusetts Amherst, Amherst, Massachusetts
Search for more papers by this authorW. Gerald Teague MD
Department of Pediatrics, University of Virginia School of Medicine, Charlottesville, Virginia
Search for more papers by this authorRobyn T. Cohen MD
Boston University School of Medicine, Boston, Massachusetts
Search for more papers by this authorSupinda Bunyavanich MD
Department of Pediatrics, Icahn School of Medicine at Mount Sinai, New York, New York
Department of Genetics and Genomic Sciences, Ichan School of Medicine at Mount Sinai, New York, New York
Search for more papers by this authorCorresponding Author
Alfin G. Vicencio MD
Department of Pediatrics, Icahn School of Medicine at Mount Sinai, New York, New York
Correspondence Alfin G. Vicencio, Professor of Pediatrics, Mount Sinai Kravis Children's Hospital, Icahn School of Medicine at Mount Sinai, One Gustave L. Levy Place, #1202B, New York, NY 10029.
Email: [email protected]
Search for more papers by this authorAbstract
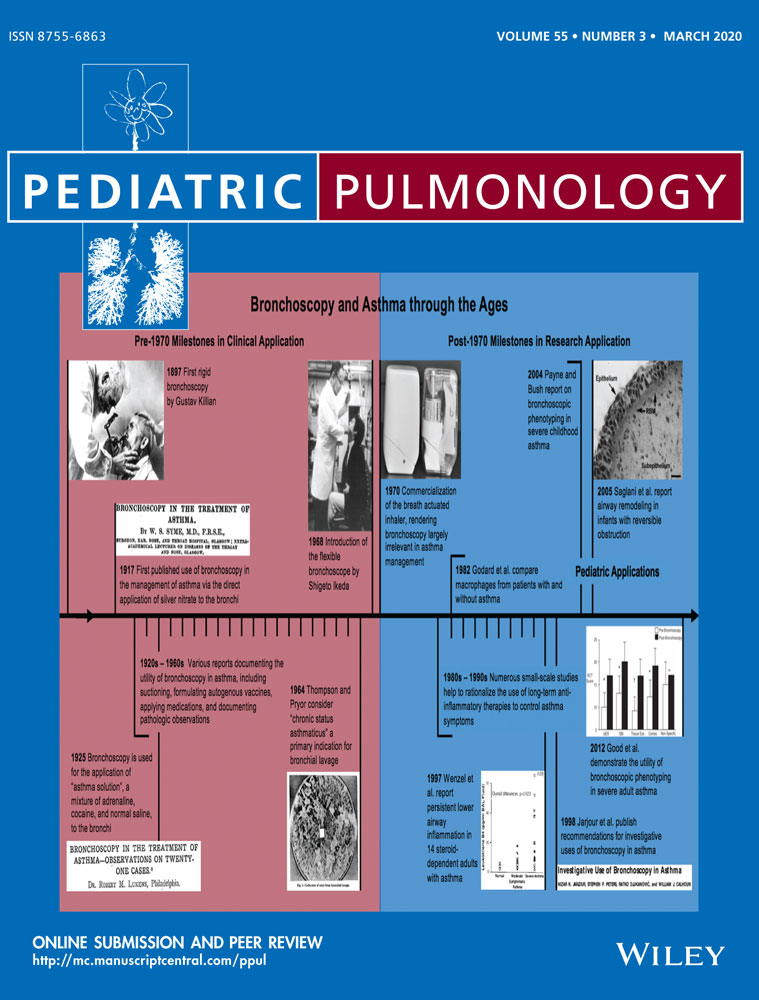
For children with severe asthma, guideline-based management focuses on the escalation of anti-inflammatory and bronchodilatory medications while addressing comorbid conditions. Bronchoscopy, in this context, has been relegated to ruling out asthma mimickers. More recently, however, there have been questions surrounding the clinical utility of bronchoscopy in severe childhood asthma. In this solicited lecture summary, we discuss the past, present, and potential future applications of bronchoscopy in severe childhood asthma.
REFERENCES
- 1Syme WS. Bronchoscopy in the treatment of asthma. BMJ. 1917; 1(2948): 868-869.
- 2Evans EH. Bronchoscopy in asthma and other cases. Ind Med Gaz. 1933; 68(11): 627-628.
- 3Thompson HT, Pryor WJ. Bronchial lavage in the treatment of obstructive lung disease. The Lancet. 1964; 284(7349): 8-10.
10.1016/S0140-6736(64)90004-2 Google Scholar
- 4Lukens RM. Bronchoscopy in the treatment of asthma—observations on twenty-one cases. Laryngoscope. 1925; 35(3): 227-234.
10.1288/00005537-192503000-00009 Google Scholar
- 5Stein SW, Thiel CG. The history of therapeutic aerosols: a chronological review. J Aerosol Med Pulm Drug Delivery. 2017; 30(1): 20-41.
- 6Maguire A, Gopalakaje S, Eastham K. All that wheezes is not asthma: a 6-year-old with foreign body aspiration and no suggestive history. Case Reports. 2012; 2012. bcr2012006640
- 7Weinberger M, Abu-Hasan M. Pseudo-asthma: when cough, wheezing, and dyspnea are not asthma. Pediatrics. 2007; 120(4): 855-864.
- 8Koul PA, Khan UH, Shah TH, Dar AM. All that wheezes is not asthma. Case Reports. 2014; 2014. bcr2013202369.
- 9Keng LT, Chang CJ. All that wheezes is not asthma: adult tracheomalacia resulting from innominate artery compression. Postgrad Med J. 2017; 93(1095): 54-55.
- 10Lee P, Tan ZY, Pham T. All that wheezes is not asthma. Thorax. 2018; 73(8): 792.
- 11 National Asthma Education and Prevention Program, Third Expert Panel on the Diagnosis and Management of Asthma. Expert panel report 3: guidelines for the diagnosis and management of asthma. Clinical Practice Guidelines. Bethesda, MD: National Heart, Lung, and Blood Institute; 2007.
- 12 Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2019. Available from: www.ginasthma.org
- 13Faro A, Wood RE, Schechter MS, et al. Official American Thoracic Society technical standards: flexible airway endoscopy in children. Am J Respir Crit Care Med. 2015; 191(9): 1066-1080.
- 14Eber E, Antón-Pacheco JL, de Blic J, et al. ERS statement: interventional bronchoscopy in children. Eur Respir J. 2017; 50(6):1700901.
- 15Ikeda S, Yanai N, Ishikawa S. Flexible bronchofiberscope. Keio J Med. 1968; 17(1): 1-16.
- 16Reynolds HY, Newball HH. Analysis of proteins and respiratory cells obtained from human lungs by bronchial lavage. J Lab Clin Med. 1974; 84(4): 559-573.
- 17Godard P, Chaintreuil J, Damon M, et al. Functional assessment of alveolar macrophages: comparison of cells from asthmatics and normal subjects. J Allergy Clin Immunol. 1982; 70(2): 88-93.
- 18Djukanovic R, Roche WR, Wilson JW, et al. Mucosal inflammation in asthma. Am Rev Respir Dis. 1990; 142(2): 434-457.
- 19Jarjour NN, Peters SP, Djukanovic R, Calhoun WJ. Investigative use of bronchoscopy in asthma. Am J Respir Crit Care Med. 1998; 157(3): 692-697.
- 20Wenzel SE, Szefler SJ, Leung DY, Sloan SI, Rex MD, Martin RJ. Bronchoscopic evaluation of severe asthma: persistent inflammation associated with high dose glucocorticoids. Am J Respir Crit Care Med. 1997; 156(3): 737-743.
- 21Good JT, Kolakowski CA, Groshong SD, Murphy JR, Martin RJ. Refractory asthma. Chest. 2012; 141(3): 599-606.
- 22Payne D, Bush A. Phenotype-specific treatment of difficult asthma in children. Paediatr Respir Rev. 2004; 5(2): 116-123.
- 23Cokugras H, Akcakaya N, Seckin I, Camcioglu Y, Sarimurat N, Aksoy F. Ultrastructural examination of bronchial biopsy specimens from children with moderate asthma. Thorax. 2001; 56(1): 25-29.
- 24Payne DN, Rogers AV, Adelroth E, et al. Early thickening of the reticular basement membrane in children with difficult asthma. Am J Respir Crit Care Med. 2003; 167(1): 78-82.
- 25Barbato A, Turato G, Baraldo S, et al. Airway inflammation in childhood asthma. Am J Respir Crit Care Med. 2003; 168(7): 798-803.
- 26Jenkins HA, Cool C, Szefler SJ, et al. Histopathology of severe childhood asthma. Chest. 2003; 124(1): 32-41.
- 27Saglani S, Malmström K, Pelkonen AS, et al. Airway remodeling and inflammation in symptomatic infants with reversible airflow obstruction. Am J Respir Crit Care Med. 2005; 171(7): 722-727.
- 28Andersson CK, Adams A, Nagakumar P, et al. Intraepithelial neutrophils in pediatric severe asthma are associated with better lung function. J Allergy Clin Immunol. 2017; 139(6): 1819-1829.e11.
- 29Grunwell JR, Stephenson ST, Tirouvanziam R, Brown LAS, Brown MR, Fitzpatrick AM. Children with neutrophil-predominant severe asthma have proinflammatory neutrophils with enhanced survival and impaired clearance. J Allergy Clin Immunol Pract. 2019; 7(2): 516-525.e6.
- 30Robinson PFM, Pattaroni C, Cook J, et al. Lower airway microbiota associates with inflammatory phenotype in severe preschool wheeze. J Allergy Clin Immunol. 2019; 143(4): 1607-1610.e3.
- 31Teague WG, Lawrence MG, Shirley DAT, et al. Lung lavage granulocyte patterns and clinical phenotypes in children with severe, therapy-resistant asthma. J Allergy Clin Immunol Pract. 2019; 7(6): 1803-1812.e10.
- 32Payne D, McKenzie SA, Stacey S, Misra D, Haxby E, Bush A. Safety and ethics of bronchoscopy and endobronchial biopsy in difficult asthma. Arch Dis Child. 2001; 84(5): 423-426.
- 33Webley WC, Salva PS, Andrzejewski C, et al. The bronchial lavage of pediatric patients with asthma contains infectious chlamydia. Am J Respir Crit Care Med. 2005; 171(10): 1083-1088.
- 34Patel KK, Vicencio AG, Du Z, Tsirilakis K, Salva PS, Webley WC. Infectious chlamydia pneumoniae is associated with elevated interleukin-8 and airway neutrophilia in children with refractory asthma. Pediatr Infect Dis J. 2010; 29(12): 1093-1098.
- 35Patel KK, Webley WC. Respiratory chlamydia infection induce release of hepoxilin A3 and histamine production by airway neutrophils. Front Immunol. 2018; 9: 2357.
- 36Xu X, Zhang D, Zhang H, et al. Neutrophil histamine contributes to inflammation in Mycoplasma pneumonia. J Exp Med. 2006; 203(13): 2907-2917.
- 37Kraft M, Cassell GH, Pak J, Martin RJ. Mycoplasma pneumoniae and chlamydia pneumoniae in asthma. Chest. 2002; 121(6): 1782-1788.
- 38Sutherland ER, King TS, Icitovic N, et al. A trial of clarithromycin for the treatment of suboptimally controlled asthma. J Allergy Clin Immunol. 2010; 126(4): 747-753.
- 39Wise F, Sulzberger MB. Urticaria and hay-fever due to trichophytin (epidermophyton interdigitale). JAMA. 1930; 95: 1504.
- 40Denning DW, O'Driscoll BR, Powell G, et al. Randomized controlled trial of oral antifungal treatment for severe asthma with fungal sensitization: the fungal asthma sensitization trial (FAST) study. Am J Respir Crit Care Med. 2009; 179(1): 11-18.
- 41Vicencio AG, Muzumdar H, Tsirilakis K, Kessel A, Nandalike K, Goldman DL. Severe asthma with fungal sensitization in a child: response to itraconazole therapy. Pediatrics. 2010; 125(5): e1255-e1258.
- 42Vicencio AG, Chupp GL, Tsirilakis K, et al. CHIT1 mutations: genetic risk factor for severe asthma with fungal sensitization? Pediatrics. 2010; 126(4): e982-e985.
- 43Goldman DL, Vicencio AG. The chitin connection. mBio. 2012; 3(2). e00056-12
- 44Moss RB. Treatment options in severe fungal asthma and allergic bronchopulmonary aspergillosis. Eur Respir J. 2014; 43(5): 1487-1500.
- 45Vicencio AG, Santiago MT, Tsirilakis K, et al. Fungal sensitization in childhood persistent asthma is associated with disease severity. Pediatr Pulmonol. 2014; 49(1): 8-14.
- 46Goldman DL, Chen Z, Shankar V, Tyberg M, Vicencio A, Burk R. Lower airway microbiota and mycobiota in children with severe asthma. J Allergy Clin Immunol. 2018; 141(2): 808-811.e7.
- 47Swain SD, Meissner N, Han S, Harmsen A. Pneumocystis infection in an immunocompetent host can promote collateral sensitization to respiratory antigens. Infect Immun. 2011; 79(5): 1905-1914.
- 48Swain SD, Meissner N, Siemsen DW, McInnerney K, Harmsen AG. Pneumocystis elicits a STAT6-dependent, strain-specific innate immune response and airway hyperresponsiveness. Am J Respir Cell Mol Biol. 2012; 46(3): 290-298.
- 49Schnipper S, Small CB, Lehach J, et al. Pneumocystis carinii pneumonia presenting as asthma: increased bronchial hyperresponsiveness in Pneumocystis carinii pneumonia. Ann Allergy. 1993; 70(2): 141-146.
- 50Gingo MR, Wenzel SE, Steele C, et al. Asthma diagnosis and airway bronchodilator response in HIV-infected patients. J Allergy Clin Immunol. 2012; 129(3): 708-714.e8.
- 51Eddens T, Campfield BT, Serody K, et al. A novel CD4(+) T cell-dependent murine model of Pneumocystis-driven asthma-like pathology. Am J Respir Crit Care Med. 2016; 194(7): 807-820.
- 52Syk J, Malinovschi A, Johansson G, et al. Anti-inflammatory treatment of atopic asthma guided by exhaled nitric oxide: a randomized, controlled trial. J Allergy Clin Immunol Pract. 2013; 1(6): 639-648.
- 53Petsky HL, Kew KM, Chang AB. Exhaled nitric oxide levels to guide treatment for children with asthma. Cochrane Database Syst Rev. 2016; 11. CD011439.
- 54Bjerregaard A, Laing IA, Backer V, et al. High fractional exhaled nitric oxide and sputum eosinophils are associated with an increased risk of future virus-induced exacerbations: a prospective cohort study. Clin Exp Allergy. 2017; 47(8): 1007-1013.
- 55Ullmann N, Bossley CJ, Fleming L, Silvestri M, Bush A, Saglani S. Blood eosinophil counts rarely reflect airway eosinophilia in children with severe asthma. Allergy. 2013; 68(3): 402-406.
- 56Ribeiro V, Andrade J, Rose S, Spencer C, Vicencio A, Bunyavanich S. Children with severe persistent asthma have disparate peripheral blood and lower airway eosinophil levels. J Allergy Clin Immunol Pract. 2019; 7(7): 2494-2496.
- 57Anderson WC 3rd, Apter AJ, Dutmer CM, Searing DA, Szefler SJ. Advances in asthma in 2016: designing individualized approaches to management. J Allergy Clin Immunol. 2017; 140(3): 671-680.
- 58Lezmi G, Deschildre A, Abou Taam R, et al. Remodelling and inflammation in preschoolers with severe recurrent wheeze and asthma outcome at school age. Clin Exp Allergy. 2018; 48(7): 806-813.
- 59Spencer CY, Millman J, Veiga K, Vicencio AG. Airway autoimmune inflammatory response (AAIR) syndrome: an asthma-autoimmune overlap disorder? Pediatrics. 2018; 141(3). e20170138
- 60Wenzel SE, Vitari CA, Shende M, Strollo DC, Larkin A, Yousem SA. Asthmatic granulomatosis: a novel disease with asthmatic and granulomatous features. Am J Respir Crit Care Med. 2012; 186(6): 501-507.
- 61 US Food and Drug Administration. FDA drug safety communication: FDA review results in new warnings about using general anesthetics and sedation drugs in young children and pregnant women. Available at: https://www.fda.gov/Drugs/DrugSafety/ucm532356.htm