Successful Clozapine Treatment for Treatment-Resistant Schizophrenia With Zinc Deficiency Severe Anemia: A Case Report
Funding: The authors received no specific funding for this work.
ABSTRACT
Introduction
Clozapine is an atypical antipsychotic drug approved for treatment-resistant schizophrenia (TRS). Despite its high efficacy for TRS, clozapine is associated with several serious adverse effects, such as neutropenia and diabetes, so it requires vigilant monitoring. Severe anemia has also been documented as a rare but serious complication with an unclear mechanism. We present a case report of severe anemia potentially associated with zinc deficiency during clozapine therapy.
Case Report
A 51-year-old woman was diagnosed with TRS without physical complications. Zinc deficiency was identified as a potential contributing factor. Zinc supplementation improved her hemoglobin levels, enabling the patient to continue clozapine at a therapeutic dose. The patient has remained stable, with no recurrence of anemia.
Discussion
Clozapine is a highly effective antipsychotic, despite side effects including blood dyscrasias. While zinc deficiency is most likely to be implicated in clozapine-induced anemia, the exact mechanism remains unclear. Further research is required to explore this relationship between clozapine and zinc decrement.
1 Introduction
Schizophrenia is a severe mental disorder that can cause significant disruption in patients’ lives due to various symptoms, such as hallucination, delusion, disorganized speech, grossly disorganized or catatonic behavior, and cognitive dysfunction [1]. Antipsychotics are commonly used to treat schizophrenia, but management is complicated in 20%–30% of patients because of resistance to treatment, a condition known as treatment-resistant schizophrenia (TRS) [2]. Clozapine is an atypical antipsychotic developed in 1959, which was temporarily withdrawn from the market due to adverse effects but reintroduced in 1989 and approved for TRS in Japan in 2009. Clozapine is thought to be superior to other antipsychotic drugs in the management of both positive and negative symptoms. In a network meta-analysis comparing 32 oral antipsychotics and a placebo [3], clozapine showed the best standardized mean difference from placebo (−0.89; 95% CI, −1.08 to −0.71), suggesting it to be the most effective agent. Clozapine is currently considered to be the gold standard for TRS treatment worldwide.
Clozapine is, however, associated with several notable adverse effects, including hematologic [4], metabolic, and cardiovascular symptoms [5]. Agranulocytosis, of most serious concern, requires frequent, vigilant blood monitoring [6]. Neutropenia is nonetheless a more common side effect of clozapine, with incidences of clozapine-induced neutropenia and agranulocytosis being 2.7% and 0.9%, respectively [7, 8]. Other hematologic side effects induced by clozapine are less common, particularly severe anemia (hemoglobin level < 8.0 g/dL). Severe anemia due to clozapine has been reported in a number of cases, attributed to erythroblastosis [9-11]; but the mechanism has been unclear.
Here, we present a case of successful clozapine treatment complicated by severe anemia, potentially related to zinc deficiency. This case report was prepared in accordance with procedures specified by the Wakayama Medical University Ethics Committee. Informed consent was obtained from the patient, and her anonymity has been preserved.
2 Case Report
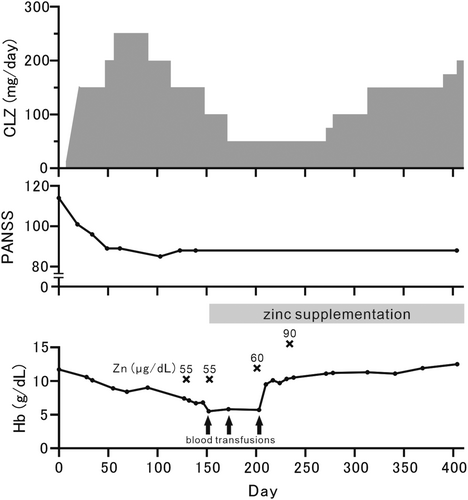
A 51-year-old Japanese woman was diagnosed with schizophrenia at the age of 25 without any physical complications. She had no alcohol use disorder, and her liver function and albumin level were generally normal. She had been hospitalized eight times due to worsening psychiatric symptoms, including severe auditory hallucinations and delusions, and increased impulsivity. She had been previously treated with multiple antipsychotics at adequate doses and durations, including risperidone, perospirone, paliperidone, asenapine, haloperidol, lurasidone, blonanserin, and brexpiprazole. However, all agents were ineffective, and there were remaining psychotic symptoms, leading to a diagnosis of TRS. Cognitive impairments in attention, in executive function, and in working memory were also observed, hindering her participation in outpatient occupational therapy. Also, lithium carbonate was ineffective in reducing impulsivity and stabilizing her emotional state, necessitating the use of an isolated room or medical restraint. Therefore, we initiated clozapine treatment as an alternative to lithium carbonate. The Positive and Negative Syndrome Scale (PANSS) before clozapine treatment was 114 points. It is noteworthy that she had a mild decrease in hemoglobin (Hb) level before administration (11.7 g/dL; normal range: 13–17 g/dL) with a normal serum iron level of 108 μg/dL (normal range: 40–188 μg/dL) and a normal ferritin level of 75 ng/dL (normal range: 5–152 ng/dL). The mild decline in Hb level was not progressive and did not require treatment. Clozapine treatment was initiated at 12.5 mg/day and gradually increased to 250 mg/day as per the regimen. However, over a nine-week period, her Hb level gradually decreased to 8.4 g/dL. Gastrointestinal endoscopy revealed no abnormalities, and examination by the hematology department ruled out myelodysplastic syndrome or any other blood disease, suggesting clozapine-induced anemia. Thus, we decided to reduce the clozapine dose from 250 mg/day back down to 150 mg/day. Although there was an improvement in her psychotic symptoms, reflected by a PANSS score of 88 points, the treatment was continued. However, the anemia progressed, reaching 6.7 g/dL at 19 weeks from the initiation of clozapine treatment, requiring multiple blood transfusions (a total of 6 units of red cell concentrate). Further reduction of the clozapine dose down to 50 mg/day did not improve the condition. Subsequent detailed blood tests revealed zinc deficiency at a level of 55 μg/dL (normal range: 80–130 μg/dL), while no abnormalities were found in other factors that could cause anemia, such as folic acid 4.2 ng/mL (normal range: 3.6–12.9 ng/mL) and vitamin B12 381 pg/mL (normal range: 233–914 pg/mL), prompting the administration of zinc acetate hydrate for supplementation at the hematologist's discretion.
Subsequently, serum zinc levels gradually increased, and her Hb level improved to 10.1 g/dL. Clozapine was titrated more slowly and cautiously than usual, up to 200 mg/day, stabilizing her psychiatric symptoms (PANSS: 88 points). Since transferring to outpatient care at our hospital after discharge, her mental condition has remained stable. In addition, despite the increase in clozapine dosage to 200 mg, there has been no further worsening of her anemia (Figure 1).
3 Discussion
This case report suggests that clozapine could lead to severe anemia, potentially associated with zinc deficiency. While clozapine demonstrated efficacy in improving psychiatric symptoms, as evidenced by the PANSS score reduction in our patient from 114 to 88, its use requires careful consideration due to potential adverse effects. Zinc supplementation improved hemoglobin levels, enabling the continuation of clozapine treatment and effective management of anemia.
Clozapine is a highly effective antipsychotic drug, although it has various side effects, including blood dyscrasias. Neutropenia is a common side effect which is related to clozapine. In a nationwide cohort and case–control study, the risk of agranulocytosis by clozapine is much higher, especially in 6 months from clozapine initiation, compared with other antipsychotics [12]. Anemia is a relatively uncommon side effect of clozapine but there are several reported cases of clozapine-induced anemia [9, 11]. Similar to our patient, a male patient with TRS reportedly developed severe anemia, which manifested as a gradual decrease in Hb levels following the initiation of clozapine [9]. Another case report highlighted clozapine-induced anemia and leucopenia in a female with schizophrenia [11]. Clozapine was implicated in both of these cases, but without understanding of the mechanism of anemia. We now report severe anemia with zinc deficiency requiring blood transfusions during clozapine treatment, which we think, for the first time, suggests a mechanism for clozapine-induced anemia. Research has suggested that smoking reduces clozapine blood concentrations, with non-smokers more likely to develop anemia [13]. In our case, the patient was a non-smoker, perhaps a contributing factor to the development of clozapine-induced anemia. Conversely, research on serum trace elements and treatment with anti-psychotic drugs reported that clozapine treatment does not affect serum zinc levels [14]. The mechanism of clozapine-induced anemia thus requires further elucidation and clarification.
Zinc is the second most abundant element in living organisms after iron and is one of the most crucial trace elements in humans, functioning as a catalyst, structural component, and regulatory ion. Although iron is the most common trace element related to anemia, zinc also plays a critical role in its development. Many studies, especially in women of reproductive age [15, 16] and preschool-aged children [17], have shown that zinc deficiency is associated with iron deficiency anemia. Several experiments in rats have revealed that coexisting zinc and iron deficiency caused anemia, whereas zinc deficiency alone does not [18, 19]. However, a few reports about zinc deficiency anemia without iron deficiency suggest that zinc deficiency alone could cause anemia, as seen in our current case [20-22]. Several animal studies indicate that zinc is a key element for erythropoiesis, a red blood cell production process by stem cells in the bone marrow [23]. In a case report on clozapine-induced bicytopenia affecting both white and red blood cells, a bone marrow biopsy suggested depressed erythropoiesis with hypoplastic anemia [7], raising the possibility that a similar mechanism of anemia might be present in our case. Nevertheless, the exact mechanism by which clozapine induces zinc deficiency remains unclear and requires further investigation.
A systematic review showed that individuals with schizophrenia tend to have an altered dietary pattern, consume a poor and unbalanced diet, leading to metabolic abnormalities [24]. Zinc dyshomeostasis has also been suggested to be related to schizophrenia itself, as indicated by a meta-analysis that reported that the mean serum zinc concentration was 12.81 μg/dL lower in individuals with schizophrenia than in healthy controls [25]. This effect was more pronounced among hospitalized patients. However, the most significant reduction in serum zinc levels was observed in drug-naïve patients compared with healthy controls. In contrast, no significant reduction was found in patients treated with antipsychotics [25]. Regarding our case, the patient was hospitalized and treated with multiple antipsychotic medications. Furthermore, the absence of progressive anemia prior to initiation of clozapine supports the hypothesis that the reduction in zinc levels was attributable to clozapine rather than to schizophrenia itself. A large cross-sectional study found no differences in cognitive performance, which is associated with disease severity, between schizophrenia patients with and without anemia [26]. However, few studies have explored this relationship in depth, highlighting the need for further investigation into the interplay among anemia, zinc levels, and disease severity.
There are a few limitations to this report. First, as a single case report, the association between clozapine and zinc deficiency anemia cannot be generalized and epidemiological studies on clozapine and reduced zinc levels are required. Second, we have not demonstrated a causal relationship between clozapine and decreased zinc levels, and there may be other contributing factors. Fundamental level research is required to examine the effects of clozapine on zinc, the effects of clozapine on zinc metabolism, and to clarify the mechanisms underlying zinc depletion associated with this medication.
In conclusion, our case report raises the possibility of zinc deficiency as a contributing factor in clozapine-induced anemia. Regular monitoring of serum zinc levels may help identify at-risk patients and optimize clozapine therapy.
Author Contributions
K.M.-Y., S.U., Y.I., S.Y., Y.K., and S.K. were involved in the patient's treatment K.M.-Y., S.U., and K.O. wrote the manuscript with input from all authors.
Acknowledgments
We thank all the medical staff involved in the patient's treatment at Wakayama Medical University and Hidaka Hospital. We also acknowledge proofreading and editing by Benjamin Phillis at the Clinical Study Support Center at Wakayama Medical University.
Ethics Statement
This case report was prepared in accordance with procedures specified by the Wakayama Medical University Ethics Committee.
Consent
Informed consent was obtained from the patient, and her anonymity has been preserved.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
All data supporting the findings of this case report are included in the main text of the article. No additional datasets were generated or analyzed during the preparation of this report.