Possible association between photic sneeze syndrome and migraine and psychological distress
Abstract
Background
Photic sneeze syndrome (PSS) is a condition that causes sneezing when the eye is exposed to sudden bright light. Because alterations in the parasympathetic and trigeminal nerve systems have been implicated in PSS, and such systems are involved in migraine and stress-related disorders, we examined the possible associations of PSS with migraine and psychological distress.
Methods
The presence of PSS and migraine was examined in 11 840 participants from the general population using a self-report questionnaire. Psychological distress was assessed by the 6-item Kessler Psychological Distress Scale (K6).
Results
The overall prevalence of PSS was 3.1%. Individuals with PSS were more likely to suffer from migraine (odds ratio = 1.97, P = 2.18 × 10–9), clinically relevant psychological distress (K6 score ≥ 5: odds ratio = 1.40, P = 0.00143), and severe psychological distress (K6 score ≥ 13: odds ratio = 1.49, P = 0.0486). Overall, K6 scores were significantly higher in those with PSS than in those without (P = 0.000013). Analysis controlling for sex and the presence of migraine showed that PSS was associated with higher K6 scores irrespective of sex or the presence of migraine.
Conclusions
The low prevalence of PSS identified in the present study may be due to the inadequate ability of the self-report questionnaire to identify PSS. Despite such limitation, the present study suggests that individuals with PSS are more likely to suffer from migraine and psychological distress than those without PSS. PSS may be a potential target for the research of migraine and stress-related disorders.
1 INTRODUCTION
Photic sneeze syndrome (PSS), also known as autosomal dominant compelling helio-ophthalmic outburst (ACHOO) syndrome, is a condition that causes sneezing when the eye is exposed to sudden bright light. PSS prevalence varies among racial and ethnic groups. For instance, Everett1 reported a prevalence of 23.1% and 2.3% in white and black students, respectively, while Semes et al2 reported a prevalence of 38.2% in white populations and 8.2% in black populations. PSS often occurs within families and is considered a hereditary condition.3 Accordingly, genome-wide association studies (GWASs), including our own, have identified several single nucleotide polymorphisms associated with PSS.4-6
Although the precise mechanism by which light triggers the sneeze reflex is unknown, Everett1 has proposed two hypotheses. According to the parasympathetic generalization hypothesis, when a light stimulus excites a specific branch of the parasympathetic nervous system, it activates other branches, resulting in nasal secretion and a tickling sensation in the nasal mucosa, which in turn induces the sneeze reflex. The optic-trigeminal summation hypothesis postulates that, during light stimulation, the activated optic nerve pathways cross-activate the trigeminal nerve pathways in the upper mesencephalic-diencephalic junction where the two pathways converge.7 Such cross-activation results in sensations in the nose, which is innervated by the second division of the trigeminal nerve. In support of the second hypothesis, a recent study reported that hypersensitivity of the trigeminal nerve is involved in PSS and that the light-induced electrical activity in the optic pathways travels directly to the trigeminal nucleus to trigger the sneeze reflex.8
In addition to the sneeze reflex, acute exposure to bright light is known to elicit pain in certain individuals. Such intolerance to light, commonly known as photophobia, is thought to result from light-induced activation of the trigeminal nerve system,9 in a manner similar to the PSS mechanism proposed in the optic-trigeminal summation hypothesis. The link between intolerance to light and the trigeminal nerve system is supported by functional magnetic resonance imaging studies that show activation of the trigeminal nerve system at the level of the trigeminal ganglion during the photophobic response.10
Photophobia is a common symptom of migraine.11 Rather unsurprisingly then, activation of the trigeminal nerves, which innervate cranial blood vessels, has been implicated in the pathophysiology of migraine.12 Given the commonalities in the mechanisms underlying PSS, photophobia, and migraine, we hypothesized that hypersensitivity of the trigeminal system in individuals with PSS could confer susceptibility to migraine.
The hypersensitivity of the trigeminal nerve postulated in PSS might also underlie the possible link between PSS and mood dysregulation.13 Trigeminal nerve stimulation (TNS) is thought to have neuromodulatory effects on cortical and subcortical regions associated with neuropsychiatric disorders. Studies have shown that TNS may have therapeutic effects on various neuropsychiatric conditions, such as drug-resistant epilepsy,14, 15 post-traumatic distress syndrome,16, 17 depression,18 and the negative symptoms of schizophrenia.19 Thus, hypersensitivity of the trigeminal nerve, which possibly underlies PSS, may also be involved in the emotional regulatory aspects of these neuropsychiatric conditions. Therefore, we further hypothesized that PSS may be associated with emotional instability and psychological distress.
The current study investigated the relationship between PSS, migraine, and psychological distress.
2 METHODS
2.1 Participants
Study participants were recruited from 11 922 Japanese individuals who participated in our previous GWAS on PSS.6 The participants were individuals who participated in the Health Data Lab project administered by Yahoo! Japan Corporation (Tokyo, Japan). Only participants who resided in Japan and were ≥18 years old were included. The participants answered a questionnaire survey via the Internet.
The study was approved by the Ethics Review Committees of GeneQuest Inc. and the National Center of Neurology and Psychiatry, Japan. All participants gave written consent for the use of their survey responses for research purposes. Those who opted out during the 2-week period after they were informed of the present study were excluded from the study. All data were anonymized prior to analyses.
2.2 Phenotypes
Phenotype data were acquired from a survey questionnaire administered to the participants via the Internet. The participants were shown a list of medical conditions/diseases and were asked to check the medical conditions/ diseases that applied to them currently or previously. Those who checked “light sneeze reflex” were treated as PSS cases, and those who checked “migraine” were treated as migraine cases.
2.3 The Kessler Psychological Distress Scale (K6)
Current psychological distress was assessed using the Kessler Psychological Distress Scale (K6). The K6 is a self-reported measure of psychological distress that includes six questions about one's emotional state; respondents rate how often they felt so sad that nothing could cheer them up, how often they felt that everything was an effort, and how often they felt nervous, hopeless, restless/fidgety, and worthless within a 30-day reference period. K6 has shown to be effective at discriminating cases of any psychiatric disorder from mentally healthy individuals.20 A previous study showed that the screening performance of the Japanese version of K6 for mood and anxiety disorders was equally high compared to K10, the longer version of Kessler Psychological Distress Scale.21 Therefore, the Japanese version of K6 was used in the present study to assess psychological distress. The participants were asked to answer each of the 6 questions based on a scale of 0 (none of the time) to 4 (all of the time). Kessler et al20 proposed a cutoff point of ≥13 for serious mental illness. A cutoff point of ≥5 has been proposed for less severe mental distress in the United States22 as well as in Japanese populations21. In the present study, a K6 score of ≥5 was used as a criterion for less severe, but clinically relevant psychological distress and a K6 score ≥ 13 as a criterion for severe psychological distress.
2.4 Statistical analysis
Differences in continuous variables between participants with and without PSS were assessed by the Mann-Whitney U test or unpaired Student's t test, depending on the data distribution. The chi-squared test was used to compare the frequencies of categorical variables. Because migraine itself could cause severe psychological distress, two-way factorial analysis of variance (ANOVA) was performed with migraine and PSS as fixed factors and the transformed K6 total score as the dependent variable to detect interaction effects between PSS and migraine on psychological distress. The aligned rank transformation method was used to transform the K6 score prior to conducting an ANOVA23. To examine the interaction effects of sex, three-way factorial ANOVA with migraine, PSS, and sex as fixed factors was also performed. Effect sizes were estimated by calculating partial eta squared (η2). The above analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 21.0 (IBM Corp, Armonk, New York, U.S.) and R Project for Statistical Computing version 3.4.1.24
3 RESULTS
A total of 11 840 participants responded to the online K6 questionnaire and were eligible for analyses. Participant demographics, K6 scores, and other participant characteristics are shown in Table 1. PSS was present in 3.1% of the participants. No significant difference in sex distribution was found between individuals with and without PSS, whereas the mean age was significantly lower in the former group than in the latter group. PSS was significantly associated with migraine (odds ratio [OR] = 1.97, 95% confidence interval [95% CI] = 1.57-2.48, χ2 = 35.8, df = 1, P = 2.18 × 10–9). PSS was also associated with clinically relevant psychological distress (K6 score ≥ 5: OR = 1.40, 95% CI = 1.14-2.72, χ2 = 10.2, df = 1, P = 0.00143) and severe psychological distress (K6 score ≥ 13: OR = 1.49, 95% CI = 1.00-2.23, χ2 = 3.89, df = 1, P = 0.0486). Figure 1 shows the proportion of individuals with migraine, clinically relevant psychological distress, and severe psychological distress in those with and without PSS. The total K6 score was significantly higher in women than in men (U = 14 713 131.5, Z = 15.04, P < 0.000001) and was significantly negatively correlated with age (Spearman's rho = −0.25, P = 5.58 × 10–162). The total K6 score was significantly higher in individuals with PSS than in those without PSS (U = 1 846 827.5, Z = 4.36, P = 0.000013), and a significant difference was observed at the nominal P < 0.05 level for each K6 item except for “hopeless.”
| Photic sneeze syndrome | No photic sneeze syndrome | Statistics | P value | |
|---|---|---|---|---|
| n | 371 | 11 469 | ||
| Age [y]a | 46.29 (12.71) | 49.92 (13.3) | df = 11 834, t = −5.18 | 2.14E-07 |
| %women | 50.9 | 47.7 | df = 1, χ2 = 1.51 | 0.22 |
| %migraine | 30.2 | 18.0 | df = 1, χ2 = 35.8 | <0.0001 |
| Total K6 score | 5.03 (4.38) | 4.20 (4.18) | U = 1 846 827.5, Z = 4.36 | <0.0001 |
| Nervous | 0.81 (0.93) | 0.67 (0.89) | U = 1 938 132.5, Z = 3.24 | 0.0012 |
| Hopeless | 0.55 (0.88) | 0.48 (0.80) | U = 2 046 690.5, Z = 1.50 | 0.13 |
| Restless | 0.78 (0.84) | 0.66 (0.81) | U = 1 943 621.5, Z = 3.13 | 0.0018 |
| Sad | 0.89 (0.98) | 0.76 (0.89) | U = 1 989 579.0, Z = 2.31 | 0.021 |
| Effort | 1.25 (1.03) | 1.01 (0.95) | U = 1 845 724.5, Z = 4.63 | <0.0001 |
| Worthless | 0.74 (1.04) | 0.61 (0.95) | U = 1 982 307.5, Z = 2.58 | 0.010 |
- Age and K6 scores are shown as mean (standard deviation).
- Abbreviations: BMI, body mass index; K6, Kessler Psychological Distress Scale.
- a Age data were missing for four subjects.
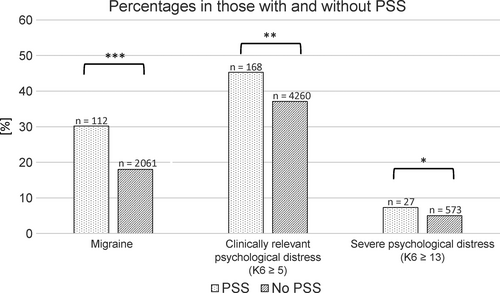
The mean total K6 scores in individuals with and without PSS are shown in Figure 2, which is stratified by the presence of migraine. Two-way factorial ANOVA showed that migraine and PSS were both associated with higher K6 total scores (migraine: df = 1, F = 47.26, P = 6.53 × 10–12, partial η2 = 0.0040; PSS: df = 1, F = 18.05, P = 2.17 × 10–5, partial η2 = 0.0015). The interaction effect between migraine and PSS was not significant (df = 1, F = 2.94, P = 0.086, partial η2 = 0.00025). A Mann-Whitney U test showed that PSS was significantly associated with higher K6 total scores in the nonmigraine group (U = 1 057 694.5, Z = 3.65, P = 0.000258).
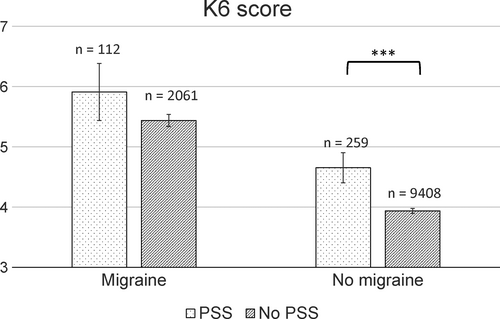
Three-way factorial ANOVA with PSS, migraine, and sex as the fixed factors also showed that migraine and PSS were both associated with higher K6 total scores (migraine: df = 1, F = 27.77, P = 1.39 × 10–7, partial η2 = 0.0023; PSS: df = 1, F = 21.80, P = 3.05 × 10–6, partial η2 = 0.0018; sex: df = 1, F = 33.70, P = 6.59 × 10–9, partial η2 = 0.0028). No significant primary or secondary interaction effects between these factors were observed (all P > 0.1).
4 DISCUSSION
The present study showed, for the first time to our knowledge, that individuals with PSS are more likely to suffer from migraine and increased psychological distress. Consistent with previous studies,25, 26 our findings demonstrate increased psychological distress in patients with migraine than in those without. We further showed that migraine and PSS were independently associated with psychological distress.
Consistent with a previous study conducted in Japan by Kuriyama et al27, K6 scores were higher in women than in men. Kuriyama et al (2009) showed that psychological distress decreased with age, with a nadir in the late 60s, but was increased in those aged above 70 years. Given that over 95% of participants in the present study were below 70 years of age, our finding that age was negatively correlated with the total K6 score is in line with Kuriyama et al27. However, the total K6 score was higher in participants with PSS, despite older age in this group. Therefore, it is unlikely that the significant association observed between PSS and psychological distress is attributable to the effect of age.
The present results support our hypothesis that hypersensitivity of the trigeminal nerve in individuals with PSS may play a role in psychological distress and migraine. However, our study design does not explain how the trigeminal nerve is involved in PSS and neuropsychiatric conditions. Precise mechanisms remain to be investigated in future studies. Considering the relatively small effect size reported in this study, the clinical implications of PSS remain unclear. However, the statistically significant associations between PSS and migraine and psychological distress were robust, and thus, the present results raise the possibility that a common mechanism exists within these conditions. In this respect, the mechanism underlying PSS may be a potential target for future investigations in neuropsychiatric research. For example, genetic variations identified in PSS may serve as candidate genes for migraine and depressive disorders. However, other interpretations may also be possible. For example, lifestyle changes due to PSS or some kind of physical damage caused by repeated sneezing may have influenced the predisposition to migraine or psychological distress.
The primary limitation of the present study was that PSS, migraine, and psychological distress were determined based on a self-reported survey. Photic sneeze reflexes may only be recognized in self-observant individuals. Furthermore, some may have been unfamiliar with the term “light sneeze reflex” used in the questionnaire. The relatively low prevalence of PSS in a Japanese population revealed in this study suggests that a substantial proportion of individuals with PSS did not report as having PSS in our survey. However, our previous GWAS, which involved the same participants as the present study, successfully replicated the SNP reported to be associated with photic sneeze reflex in a Caucasian population, indicating that our survey correctly identified individuals with PSS to some extent. Independent PSS evaluation in future studies is necessary to verify the prevalence of PSS in Japanese individuals. Another limitation of the present study was the cross-sectional design of the study, which did not allow inference of causality. Although genetically determined PSS would not occur as a result of psychological distress or migraine, it is unknown whether every PSS is a genetically determined trait. We should not rule out the presence of a subset of PSS with a low genetic contribution that is induced by migraine attacks, migraine therapy, or psychological distress. Still, another limitation was that the present study did not evaluate the participants’ trigeminal hypersensitivity. Further studies are required to draw any conclusion regarding the involvement of hypersensitivity of the trigeminal system in migraine, psychological distress, and PSS.
In conclusion, the present study showed that PSS was associated with migraine and higher psychological distress. Our findings suggest that PSS could be an important potential target for the research of migraine and stress-related disorders. Future studies are warranted to investigate the common mechanism underlying PSS, migraine, and psychological distress.
ACKNOWLEDGMENTS
This work was supported by internal funding from GeneQuest Inc. and an NCNP Intramural Research Grant for Neurological and Psychiatric Disorders (H.K., grant number 27-1). These sources provided financial support only.
CONFLICT OF INTEREST
K.S. and S.T. are board members, and S.A. and S.N. are employees of GeneQuest Inc. The authors declare no conflict of interest for this article.
AUTHOR CONTRIBUTIONS
D.S. and H.K. designed the study, and D.S. wrote the draft of the manuscript. K.S., S.T., S.A., and S.N. provided the questionnaire response data used in the present study. S.A., S.N., and D.S. performed statistical analyses. H.K. supervised the data analysis and writing of the paper. K.S. and S.T. also supervised the writing of the paper and gave critical comments on the manuscript. All authors contributed to and have approved the final manuscript.
DATA REPOSITORY
The data that support the findings of this study were from GeneQuest Inc., but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data may, however, be available from the authors upon reasonable request and with permission of GeneQuest Inc.
APPROVAL OF THE RESEARCH PROTOCOL BY AN INSTITUTIONAL REVIEWER BOARD
The study was approved by the Ethics Review Committees of GeneQuest Inc. and the National Center of Neurology and Psychiatry, Japan.
INFORMED CONSENT
All participants gave written consent for the use of their survey responses for research purposes. Those who opted out during the 2-week period after they were informed of the present study were excluded from the study.