NF-κB signaling in inflammation and cancer
Abstract
Since nuclear factor of κ-light chain of enhancer-activated B cells (NF-κB) was discovered in 1986, extraordinary efforts have been made to understand the function and regulating mechanism of NF-κB for 35 years, which lead to significant progress. Meanwhile, the molecular mechanisms regulating NF-κB activation have also been illuminated, the cascades of signaling events leading to NF-κB activity and key components of the NF-κB pathway are also identified. It has been suggested NF-κB plays an important role in human diseases, especially inflammation-related diseases. These studies make the NF-κB an attractive target for disease treatment. This review aims to summarize the knowledge of the family members of NF-κB, as well as the basic mechanisms of NF-κB signaling pathway activation. We will also review the effects of dysregulated NF-κB on inflammation, tumorigenesis, and tumor microenvironment. The progression of the translational study and drug development targeting NF-κB for inflammatory diseases and cancer treatment and the potential obstacles will be discussed. Further investigations on the precise functions of NF-κB in the physiological and pathological settings and underlying mechanisms are in the urgent need to develop drugs targeting NF-κB for inflammatory diseases and cancer treatment, with minimal side effects.
1 INTRODUCTION
A nuclear transcription factor is a type of protein that binds to a sequence of conserved nucleotides in the gene's promoter region to initiate the transcription of this gene. The nuclear factor of κ-light chain of enhancer-activated B cells (NF-κB) is one of the nuclear transcription factors with an extensive range of biological functions, which exists in almost all types of mammal cells. In 1986, Sen and Baltimore discovered NF-κB for the first time through its interaction with a defined site in the enhancer of the κ chain of immunoglobulin gene in B cells.1 Since then, intensive studies have established the critical roles of NF-κB on diverse biological processes, including cell proliferation, metastasis, response to DNA damage, apoptosis, and immune response through its vast target genes.2, 3 Therefore, NF-κB is tightly correlated with human diseases such as inflammation, cancer, and autoimmune diseases,4, 5 and understanding the regulating mechanism and function of the NF-κB signaling pathway is not only important for revealing the fundamental principles of cellular biology but also crucial to study the pathogenesis and treatment of many human diseases. In this review, we will summarize the progress of NF-κB study focusing on the crucial roles of this transcriptional factor family in many aspects of inflammation and cancers in the last 35 years, highlighting NF-κB as a potential therapeutic target for human inflammatory disease and cancer treatment.
2 THE NF-ΚB PATHWAY
2.1 NF-κB/Rel protein family
In humans, the NF-κB superfamily comprises five transcription factors: NF-κB1 (p50), NF-κB2 (p52), RelA (p65), RelB, and REL (c-Rel).6 These proteins all contain a Rel homology domain (RHD), a conserved N-terminal domain, which is very important for DNA binding, dimerization, and nuclear localization. According to the similarity of amino acid sequence within the RHD in the C-terminal, the NF-κB superfamily is generally divided into two subfamilies: NF-κB subfamily (p50 and p52) and Rel subfamily (Rel, RelA, and RelB). NF-κB1 (p50) and NF-κB2 (p52) are produced by the processing of protein precursor, p105 and p100, respectively, with ankyrin (ANK) repeat domains in the C-terminal, which form dimers with other NF-κB family members. The inhibitor of the NF-κB (IκB) protein family controls the activation process of NF-κB by interacting with transcriptional factors. The proteins bind and persist in the cytoplasm, while the Rel protein (Rel, RelA, RelB) has no protein precursor but a conserved transactivation domain in the C-terminal.7 These members of the NF-κB family share a highly conserved 3000-amino-acid RHD, which plays a crucial role in their function.8-10 In most cases, all five NF-κB proteins could form homodimers and heterodimers with each other to start gene transcription.11 However, RelB is a special exception, which only forms heterodimers. The most common NF-κB heterodimer is mainly composed of NF-κB1 (p50) and RelA (p65) (Figure 1). Whether NF-κB dimer activates transcription or inhibits transcription depends on the DNA regions it binds to and the interaction with other transcription factors.12, 13
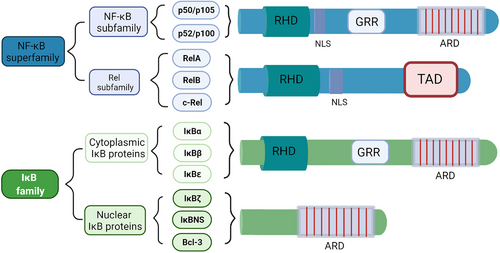
2.2 The IκB protein family
The activity of NF-κB dimer is regulated by the IκB protein. The IκB family is characterized by ANK repeats that interact with the RHD domain of NF-κB protein.9 The IκB protein family has eight members including IκBα, IκBβ, IκBɛ, IκBζ, IκBNS, Bcl-3, p100, and p105, and every member contains a series of ANK repeat domain (ARD)14 (Figure 1). The ARD of IκBs forms a slightly curved cylindrical structure, which contains amino acid residues that specifically recognize and bind to NF-κB dimers. These repetitive sequences can interact with RHD, allowing IκB to bind to NF-κB, preventing NF-κB from entering the nucleus.11, 15, 16 The activation of NF-κB relies on the degradation of IκB protein. Upon activation, IκBα is phosphorylated by IκB kinase (IKK) complex and ubiquitinated and degraded through the proteasome-dependent pathway, releasing NF-κB into the nucleus for transcription to activate target genes. NF-κB interacts with newly synthesized IκB in the nucleus and exits the nucleus into the cytoplasm, forming the cycle of a non-phosphorylated nuclear-cytoplasmic shuttling and inactivation.10, 16, 17 It should be noted that the C-terminal sequence of the precursor protein p100/p105 of p50/p52 also contains the ANK repeat sequence like IκB, which allows p100/p105 to inhibit the activity of NF-κB like IκB.18, 19
2.3 Activation of NF-κB
The NF-κB activation signaling pathways have been well studied. There are two types of NFκB activation signaling pathways: the canonical and the noncanonical pathways,20 relying on distinct molecular mechanisms to activate NF-κB, as well as the different sets of target genes involved in cell proliferation, differentiation, and immune response.16, 21
The IKKs complex is a large multi-component protein kinases complex, including two homologous catalytically active subunits IKKα (IKK1) and IKKβ (IKK2) and an auxiliary subunit IKKγ (NEMO, NF-kappaB essential modulator).22 IKK can be activated by various stimuli such as growth factors, cytokines, stress factors, and microbial components.17 The two catalytically active IKK subunits participate in different pathways. The noncanonical NF-κB activation pathway is mainly regulated by IKKα, while the regulation of the canonical NF-κB activation pathway induced by pro-inflammatory cytokines and various microbial products requires the participation of IKKβ. The oligomerization of IKKα/β/γ can affect the activity of IKKβ.17, 23, 24 Although IKKγ has no catalytic activity, it is necessary for the canonical pathway. IKKγ can form an IKK complex with other IKKs through its N-terminal, and its C-terminal can mediate the interaction with the upstream signal adaptor.16, 22, 25
In the canonical NFκB pathway, the key event is the phosphorylation of IκB protein mediated by IKKs (Figure 2). The adaptor molecule, ubiquitin ligase, and protein kinase activate the IKK complex at different levels.22, 26 The canonical activation pathway of NF-κB is stimulated by various factors, such as tumor necrosis factor receptor (TNFR) superfamily members, ligands of various cytokine receptors, pattern recognition receptors (PRRs, like Toll-like receptor (TLR) ligands), as well as B-cell receptor (BCR) and T-cell receptor (TCR).16, 27, 28 After stimulation and upstream signal transduction, IKKs phosphorylate IκBs, which in turn are ubiquitinated by ubiquitin ligase and degraded by 26S proteasome, losing the ability to bind to NF-κB. When IκB is degraded, NF-κB is dissociated from the NF-κB/IκBs complex and transferred into the nucleus, binds to the target gene promoter region on DNA, and initiate the transcription of the target gene.5, 11, 29 In this activation process, p50/RelA and p50/c-Rel have mainly involved dimers. In addition, in the canonical NF-κB pathway, one of the target genes activated is the gene encoding IκBα (Nfkbia), so IκBα is quickly re-synthesized after degradation, and the newly synthesized IκBα can directly bind to NF-κB in the nucleus. In this way, NF-κB is dissociated from the κB-binding site of DNA. The NF-κB/IκBs complex is exported back to the cytoplasm to keep the original latent state, fulfilling the cycle of NF-κB activation and inactivation. Therefore, the activation of the canonical NF-κB pathway is usually robust and transient.9 The canonical NF-κB pathway plays an important role in cell survival and proliferation, tumor cell epithelial to mesenchymal transformation (EMT), angiogenesis, cancer metastasis, and inflammation.
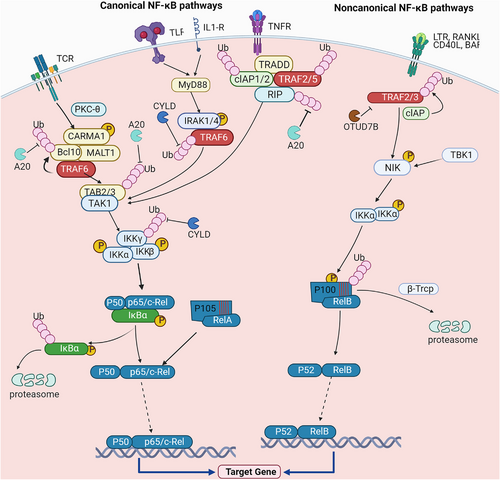
In the noncanonical NF-κB pathway, the key event is the processing of the precursor protein p100 of NF-κB2 rather than the degradation of IκBα (Figure 2). Compared with the canonical pathway with a wide variety of activators, the noncanonical pathway has relatively fewer activators. Noncanonical pathway selectively responds to specific stimuli, including ligands for part of TNF receptor family members, like lymphotoxin (LT) β receptor (LTβR), CD40, B-cell activation factor family (BAFF), and receptor activator of NF-κB (RANK).30-34 Under the action of stimuli, the corresponding receptor is activated, leading to degradation of TNF receptor-associated factor 3 (TRAF3). The protein level of NF-κB-induced kinase (NIK) is mediated by TRAF3-cellular inhibitor of apoptosis (cIAP) under the steady-state condition. It is currently believed that NIK and IKKα mediate the conversion of p100 to p52, which are the key components of the noncanonical NF-κB pathway.35 NF-κB2 exists in the form of precursor p100 under the non-stimulated condition. p100 functions as IκB protein, binding to RelB and retaining RelB in the cytoplasm.36 Together with IKKα, NIK mediates the phosphorylation of p100, which is further conjugated with ubiquitin chains mediated by β-transducin repeats-containing proteins (β-TrCP) E3 ligase. Ubiquitinated p100 is processed to generate p52, forming p52/RelB heterodimer.30, 32, 37
Two NF-κB pathways have shared characteristics: forming functional NF-κB dimer and translocating the dimer into nuclear. The difference between these two pathways is that the activation of the canonical pathway is to rely on the degradation of IκBα; meanwhile, in the noncanonical NF-κB pathway, processing of p100 into p52 does not only generate p52 but also liberate RelB from p100, forming p52/RelB dimer. The resynthesis of NIK is the key to start the downstream pathway, so the activating non-standard NF-κB pathway is much slower than the standard pathway.21 Optimizing target gene expression also requires the interaction of NF-κB with other transcription factors, such as activator protein 1 (AP1), signal transducer and activator of transcription (STAT) family members, and interferon regulatory factors (IRFs).38-40
2.4 Regulation of NF-κB pathway
As mentioned in the previous chapter 2.3, NF-κB is often blocked in the cytoplasm by IκBs, keeping the entire pathway silent. However, once activated by stimuli (regardless of the various stimuli in the canonical pathway or a subset of specific stimuli in the noncanonical pathway), NF-κB is activated to induce the production of pro-inflammatory mediators and molecules leading to inflammation and activation and differentiation of the immune cell.29 If the NF-κB activation is dysregulated, diseases such as chronic inflammation, tumors, and autoimmune diseases may occur. Therefore, NF-κB is strictly regulated to maintain homeostasis.
First of all, as an inhibitory protein of NF-κB, IκB plays a very important role in controlling the intensity and duration of NF-κB activity. The target genes of NF-κB include genes encoding IκB, such as Nfkbia (encoding IκBα) and Nfkbie (encoding IκBε). When the activated NF-κB dimer enters the nucleus to bind to the κB-binding site, target genes including Nfkbia are transcribed, and the newly generated IκBα and IκBε proteins bind and drive the NF-κB dimer from the nucleus to the cytoplasm. This dynamic negative feedback mechanism is critical for keeping the activation of NF-κB in check.41-43 Although both IκBα and IκBε have regulatory functions, they function in different ways. Compared with the rapid production and inhibition of IκBα, IκBε provides slower negative feedback regulation with delayed expression.44 In contrast, another member of the IκB family, IκBβ, directly binds to RelA and c-Rel in the nucleus to counteract the inhibitory function of IκBα. When the hypo-phosphorylated IκBβ binds to RelA and c-Rel, the inhibitory effect mediated by IκBα is impaired, and the continuous transcription of the target gene is maintained.24, 45 In addition to driving NF-κB back to the cytoplasm through the IκB protein, another way to downregulate NF-κB activation is to degrade NF-κB dimers in the nucleus directly. For example, elongin-B-elongin-C-cullin-SOCS1 (ECS) is a ubiquitin ligase complex that promotes ubiquitination and subsequent degradation of RelA in the nucleus.46-48 Studies have also reported that the E3 ubiquitin ligase post-synaptic density-95, disks-large, and zonula occludens-1 and Lin-11, Isl1 and Mec-3 (LIM) domain protein 2 directly remove RelA from the DNA binding site and mediate its degradation to suppress NF-κB transcription activity.49, 50 Protein inhibitor of activated STAT 1 (PIAS1) also moves to the promoter region of NF-κB target genes after phosphorylation of IKKα, inhibiting the binding of RelA-containing dimers to DNA.51-53
Secondly, the studies on NF-κB signaling pathways reveal that ubiquitination is essential for NF-κB activation. In the canonical NF-κB pathway, NF-κB activation mediated by multiple stimuli requires ubiquitination. For example, when interleukin-1 receptor (IL-1R) or TLR is activated, the ubiquitination of tumour necrosis factor receptor-associated factor 6 (TRAF6) requires TRAF6-regulated IKK activator 1 (TRIKA1, a dimeric ubiquitin-conjugating enzyme complex, composed of ubiquitin-conjugating enzyme 13 (Ubc13) and ubiquitin E2 variant 1Uev1A).54, 55 The function of TRIKA1 is to synthesize K63-linked polyubiquitin chains on IKKγ and TRAF6.54-56 TRAF6 requires TRIKA2 (a complex composed of TAK1, TAB1, and TAB2) to activate IKK, and the activation of TRIKA2 requires ubiquitination of the adaptor protein TAB2/3.55, 57, 58 Similarly, when stimulation goes through TNFR, the activation of IKK depends on K63-ubiquitination of receptor-interacting protein 1 (RIP1), and this process is mediated by cIAP1/2.59 In the noncanonical NF-κB pathway, p100 ubiquitination is the key event to regulate NF-κB activation. β-TrCP acts as a ubiquitin E3 ligase to mediate inducible p100 ubiquitination, another E3 ligase Fbxw7α requires glycogen synthase kinase 3 (GSK3)-mediated phosphorylation to mediate ubiquitination and degradation of p100.37, 60 Another molecule of interest is deubiquitinase (DUB) A20. A20 contains the DUB domain and the C2-C2 zinc finger E3 ubiquitin ligase domain, which inhibits K63 ubiquitination during the activation of NF-κB, leading to the decomposition of the IKK complex. A20 also mediates the K48 ubiquitination of RIP1 after inhibiting K63 ubiquitination, causing the degradation of RIP1 and suppressing the signaling pathway induced by TNFα.61-64 As a key enzyme that inhibits ubiquitination in the canonical NF-κB pathway, A20 regulates NF-κB activity by coordinating with another E3 lineage such as Itch.65 Meanwhile, the A20 encoding gene, Tnfaip3, is one of the NF-κB target genes to mediate the inactivation of NF-κB, suggestive of negative feedback regulation.66 Similar to A20, the tumor suppressor protein cylindromatosis (CYLD) is also a DUB involved in the regulation of NF-κB activity. Its function is to remove K63 ubiquitin chain of key molecules upstream of IKK, including TRAF2/6 and IKKγ.67-69 In noncanonical NF-κB pathway, ovarian tumor domain-containing protein 7B (OTUD7B) functions as the DUB of TRAF3 to stabilize TRAF3 protein upon stimulation.70 OTUD7B deficiency leads to enhanced noncanonical NF-κB activity. Additionally, OTUD 1 is also a DUB, which inhibits the ubiquitination of p100, leading to the stabilization of p100 under stimulation condition and steady state.71
Up to date, all the noncanonical NF-κB-activating stimuli activate NIK, which means that NIK is essential for noncanonical NF-κB activation.72 Considering the importance of NIK, the regulatory factors of NIK are also considered to play an important role in the regulation of NF-κB. As a negative regulator of NIK, TRAF3 binds to NIK through the N-terminal region causing NIK degradation in a ubiquitination-dependent way and keeping NIK protein at a very low level.73 This process also requires the participation of TRAF2 and ubiquitin E3 ligase cIAP1/2.74 This constitutive proteasome-mediated degradation regulated by TRAF2, TRAF3, and cIAP1/2 inhibits NIK.33, 74 NIK is also regulated by TBK1. TBK1 mediates the phosphorylation of NIK at Ser862, which is located in the degradation domain of NIK, making the phosphorylated NIK unstable.75, 76 Moreover, TBK1 forms a ternary complex with TRAF family member-associated NF-κB activator (TANK), and TRAF2 and plays a role upstream of the NIK and IKK complex, a substitute for the receptor signaling complex for TRAF-mediated NF-κB activation.77 Kinase inactive TBK1 inhibits TANK-mediated NF-κB activation but does not block TNFα, IL-1, or CD40-mediated NF-κB activation.77 IKKα also mediates the negative feedback regulation of NIK. IKKα phosphorylates the C-terminus of NIK and causes NIK degradation to prevent excessive accumulation of NIK.78
In summary, most of the regulating mechanisms of the NF-κB pathway are based on the regulation of key molecules or processes of this pathway, such as IKKs, NIK, ubiquitination. These mechanisms also indicate that the activation of NF-κB is strictly regulated at multiple layers. Due to various stimuli and target genes involved in the NF-κB pathway, the precise and comprehensive understanding of regulating mechanisms of the NF-κB pathway requires additional intensive studies in vivo and in vitro.
3 NF-ΚB AND INFLAMMATION
Inflammation is a protective response to infection and injury,4 which is usually beneficial and transient, but sometimes inflammation is also harmful. Excessive inflammation causes tissue damage and inflammation-related diseases. As the central activator of a variety of pro-inflammatory genes, NF-κB plays an important role in innate and adaptive immune cells and inflammation.5, 79 Due to the diversity of inflammatory factors, including infectious and non-infectious stimuli, the function of NF-κB in inflammation is complicated.
3.1 NF-κB regulates innate immune response and inflammation
The innate immune cells including macrophages, dendritic cells (DCs), and neutrophils, are required to produce inflammatory mediators and regulators to eliminate pathogens, while at the same time avoiding a sustained inflammatory response through negative feedback mechanisms.80 The PRRs expressed by these cells can detect various microbial components, so-called pathogen-associated molecular patterns (PAMPs). PRRs can also sense molecules released by necrotic cells and damaged tissues, called damage-associate molecular patterns (DAMPs).81, 82 The PRRs on innate immune cells induce the expression of pro-inflammatory cytokines such as TNF, IL-1, IL-6, IFN-I, chemokines, and antimicrobial proteins and mediate an inflammatory response to eliminate pathogens and repair damaged tissue.83, 84 Different PRRs families have different structural characteristics and respond to different PAMPs and DAMPs. Five PRR families have been found in mammals, including TLRs, NOD-like receptors (NLRs), RIG-I-like receptors (RLRs), C-type lectin receptors (CLRs), and cytosolic DNA sensors.83, 85-87 The activation of the canonical NF-κB pathway through these PRRs induces pro-inflammatory cytokines, chemokines, and other inflammatory mediators.82, 88 Moreover, NF-κB plays an important role in the signal transduction mediated by granulocyte-macrophage colony-stimulating factor (GM-CSF) and myeloid progenitor cell differentiation.89 The development of innate immune cells from myeloid progenitor cells is specifically affected by different members of the NF-κB transcription factor family.90
3.1.1 NF-κB functions in macrophage
Macrophages are the phagocytic innate immune cells against infection, and NF-κB is crucial to regulate macrophage function. Macrophages can be activated by many PAMPs and DAMPs and secrete cytokines and chemokines.4 Activated macrophages can differentiate into different phenotypes, including M1 and M2 macrophages.91 M1 macrophages are characterized by producing pro-inflammatory cytokines to promote inflammation, while M2 macrophages produce anti-inflammatory cytokines to inhibit inflammation.92, 93 NF-κB is a key transcription factor of M1 macrophages and is required for the expression of a large number of inflammatory genes.91 TLR signaling plays an important role in regulating the polarization of macrophages. A clear example is the TLR4 ligand lipopolysaccharide (LPS), which promotes the differentiation of macrophages to the M1 phenotype.94 Under LPS stimulation, TLR4 recruits toll-interleukin 1 receptor domain-containing adaptor protein (TIRAP) and Toll/IL-IR domain-containing adapter-inducing IFN-beta (TRIF)-related adaptor molecule (TRAM) and further recruits MyD88 and TRIF for downstream signaling.94, 95 The signal from MyD88 activates the IRAK family (IRAK1 and IRAK4), which in turn stimulates TRAF6 and activate TAK1.94, 96-98 Subsequently, TAK1 mediates the phosphorylation and activation of IKKs, which in turn phosphorylates IκBα, leading to ubiquitin-dependent IκBα degradation and NF-κB activation, and the expression of pro-inflammatory cytokines.56, 99, 100 TRIF-dependent signaling pathways can mediate inflammatory cytokines by recruiting TRAF6 and RIP1 to activate the canonical NF-κB pathway.28, 54, 96, 101 TRAF3 can also recruit TRIF-dependent signaling pathways, activate TBK1 and IKKɛ and phosphorylate IRF3, and then induce the dimerization of IRF3, leading to the transcription of pro-inflammatory cytokines and Type I IFNs.28, 91, 102 NF-κB can also regulate other pathways to regulate the inflammatory function of macrophages. IKKβ can inhibit the activation of STAT1 in macrophages and suppress its inflammatory function.103 In general, NF-κB is a key mediator of the inflammatory response of macrophages and mediates the pro-inflammatory signaling functions. It was found in mice that if both c-Rel and p50 proteins are defective, the innate immune response to bacterial sepsis will be impaired, and macrophages were able to exert normal immune functions.104
3.1.2 NF-κB regulates DC function
As primary antigen-presenting cells (APCs), DCs present antigens to T cells and activate the adaptive immune response as a bridge to link innate immunity with adaptive immunity.105 Under the stimulation of PRRs, DCs sense infection and tissue damage through the canonical NF-κB pathway and mature into APCs.106 DCs also express members of the TNFR superfamily such as CD40, LTβR, and RANK, which can stimulate the noncanonical NF-κB pathway.107 It has been found that both canonical and noncanonical NF-κB pathways regulated DC development and maturation.108 For example, the increase of RelB expression level is related to DC maturation, and RelB-deficient DCs cannot induce antigen-specific T-cell responses in vitro and in vivo.109, 110 A recent study found that RelB-deficient mice have spontaneous allergic airway inflammation, but the adoptive transfer of RelB-sufficient DCs can reverse this phenotype.111 RelB is considered a component of the noncanonical NF-κB transcription factor, but the canonical pathway NF-κB is also critical to the RelB activity in DCs112, 113 since RelB activity in DCs is negatively regulated by IκBα and IκBε.106 In addition to RelB, targeted deletion of IKKβ in DCs can prevent the accumulation of non-lymphoid tissue DCs in lymph nodes and impair the transformation of regulatory T cells.114 In short, it is clear that RelB plays an important role in the development and maturation of DCs, but it is necessary to explore the regulatory mechanism of other NF-κB pathway components in DCs.
3.2 Functions of NF-κB in adaptive immunity
Inflammation also involves adaptive immunity. After activation, T cells and B cells proliferate and differentiate into effector cells. These effector cells mediate different immune responses, including the secretion of cytokines, cytotoxic T lymphocyte response, and the production of antibodies by B cells.29 It is worthy of special attention that the activated CD4+ T cells can differentiate into effector T-cell subsets with different functions, including Th1, Th2, Th9, Th17, Tfh, and regulatory T (Treg) cells.115-117 The differentiation of CD4+ T cells is regulated not only by the cytokines secreted by APCs and other innate immune cells but also by T-cell intrinsic factors.4 Th1 cells produce pro-inflammatory cytokines IL-12 and Interferon-γ (IFN-γ) to activate macrophages and mediate the immune response to intracellular pathogens and participate in inflammation.115 Th2 cells release IL-4, IL-5, and IL-13 and stimulate the response of mast cells, eosinophils and basophils to pathogens.118, 119 Th17 cells can produce IL-17 and IL-22 to recruit neutrophils and monocytes to the site of inflammation and mediate immune responses against pathogens or autoantigens.117 Treg cells are produced during the intrathymic development and can produce cytokines, such as IL-10 and transforming growth factor-β (TGF-β), to suppress the immune response.115, 117, 120 Similar to CD4+ T cells, activated naive CD8+ T cells can also proliferate and differentiate into various effector and memory cell types, including T effector cells, T memory stem cells, and T central memory cells, which are responsible for the elimination of tumor cells and viral infections cells.121-123 While B lymphocytes develop in the bone marrow, they differentiate into plasma cells that can produce pathogen-specific antibodies after activation.124 Memory B cell is formed in the germinal center after the initial infection. In the case of re-infection, memory B cells quickly produce antibodies and play an important role in the secondary immune response.125
3.2.1 NF-κB in T cell
Many studies have proved that NF-κB is necessary for the differentiation of effector T cells and the recall response of memory T cells.126-129 The initial activation of primitive T cells through TCR and costimulatory signals depends on the canonical NF-κB pathway.130 TCR activates the canonical NF-κB pathway through the CARD-containing MAGUK protein 1 (CARMA1)/Bcl10/membrane-associated lymphoid tissue (MALT) 1 complex, which requires protein kinase C-θ-mediated phosphorylation of CARD-containing MAGUK protein 1 (CARMA1).131-133 After T cell activation, some TNFRs are induced to mediate the activation of the noncanonical NF-κB pathway.134 The noncanonical NF-κB pathway plays a role in regulating the development of natural killer T cells and γδT cells, and this function is mediated by medullary thymic epithelial cells.135-137
CD4+ T cells differentiate into different effector cells after stimulation, thereby participating in various immune responses. In mice, inhibiting the activation of NF-κB by expressing an anti-degradation IκBα in T cells can reduce the differentiation of Th1 cells.138 The generation of Th1 cells also requires c-Rel. The main function of c-Rel is to mediate Th1 polarization cytokines in APC. Mice with c-Rel deficiency have impaired Th1-mediated immune response and impaired IFN-γ production.139 The production of IFN-γ relies on RelA; and another family member, RelB, also plays an important role in Th1 differentiation through regulating T-bet.140 NF-κB synergized with the IL-4 to promote the development of Th2 cells by triggering the activation of the transcription factor STAT-6.141, 142
An initial study found that T-cell-specific IKKβ-deficient mice have impaired T-cell activation and are completely resistant to experimental autoimmune encephalomyelitis, a Th17-dependent autoimmune disease.143 More studies later proved that NF-κB regulated Th17 cells. For example, the defect of RelA in DCs results in reduced production of IL-1α, IL-1β, and IL-6 under LPS stimulation, which affects the Th17 differentiation.144, 145 In CD4+ T cells, c-Rel mediates the expression of IL-21, an important cytokine for Th17 and Tfh cell differentiation, upon TCR stimulation. Experiments have confirmed that c-Rel-deficient mice have defects in Th17 and Tfh differentiation.146 Another NF-κB family member, p52, can promote the pathological function of Th17 cells in neuroinflammation by regulating GM-CSF.147 In addition, as a key adaptor in TCR signaling, the lack of CARMA1 impairers Th17 development.145 The function of NF-κB on Th9 cell differentiation is less known. A study found that OX40, a member of the TNFR family, activated TRAF6 and NIK in CD4+ T cells, which further activated the noncanonical NF-κB pathway and promoted the production of Th9 cells.148
Tregs are crucial to prevent autoimmunity and chronic inflammation.149 Although NF-κB is proved to promote T-cell activation and effector T-cell differentiation, NF-κB is also involved in Treg generation. The Treg development in the thymus and the expression of the forkhead box P3 (Foxp3) depend on c-Rel.150-152 In addition, RelA and c-Rel, which are activated by canonical NF-κB signals, participate in mTEC differentiation by regulating the transcription of RelB and also regulate the negative selection of autoreactive T cells and development of regulatory T cells.153 p105 deficiency can also make CD4+ T cells more resistant to Treg-mediated suppression of inflammation.154 In the mice lacking canonical NF-kB pathway components (including CARMA1, IKK, BCL10, and TAK1), it was found that fewer Tregs were produced.155 A significant decrease in Tregs' development was also observed in mice with a deletion in CYLD, the negative regulator of IKKs.156 It is worth noting that Ubc13 maintains the immunosuppressive function of Tregs through the canonical NF-κB signaling pathway and prevents Tregs from acquiring an inflammatory phenotype.157 The development of Treg may also be affected by the ablation of non-canonical NF-kB signaling.158 For example, a study found a decrease of Treg in mice with NIK knockout.159
3.2.2 NF-κB and B cell
NF-κB is essential for the development, survival, and function of B cells.160, 161 The activation of NF-κB family members p52 and RelB and the upstream kinases NIK and IKKα can participate in the formation of germinal centers.162-166 The initiation and maintenance of germinal center (GC) require the cooperation of different cells, including B cells, Tfh cells, follicular regulatory T cells, macrophages and follicular DCs.167, 168 Under the stimulation of LTβR, the noncanonical NF-κB pathway in stromal cells mediate the production of chemokines, including CXCL13 and CCL21, to provide migration signals to B cells and promote GC formation.169 This process also promotes the B cells proliferation with high-affinity BCR and clearance of the low-affinity B cells.170, 171 These high-affinity B cells differentiate into plasma cells and memory B cells and initiate humoral immune responses.172 In RelB-deficient mice, the induction of CXCL13 and CCL21 is reduced, leading to defects in the microstructure of the spleen and defects in the development and structure of lymphatic organs.169 In addition, recent studies have shown that in NIK-knockout (KO) mice, the deficiency of NIK reduces the number of GC B cells and class-switching.173, 174 It was found that deleting nfkb2 and Relb genes in B cells of germinal centers would lead to the collapse of established germinal centers.163, 169, 175 In short, NF-κB plays an important role in regulating B-cell survival, differentiation, and maintenance of germinal centers.
3.3 NF-κB is involved in inflammatory diseases
3.3.1 Rheumatoid arthritis (RA)
RA is an autoimmune and inflammatory disease characterized by chronic inflammation caused by immune cells infiltrating into the synovium, which is associated with the destruction of cartilage and bone, and progressive joint destruction occurs over time.176, 177 Studies on animal models and human patients have confirmed that NF-κB is an important inflammatory mediator in RA.4 Studies have found that NF-κB is activated in the synovial tissue of a mouse arthritis model, and the activation of NF-κB increases as the disease progresses.178 Similarly, in the early studies, NF-κB activation was detected in the synovial tissue of RA patients, and it was determined that NF-κB plays an important role in joint inflammation.179-181 The pro-inflammatory effect of NF-κB in RA has long been recognized; both the canonical and the noncanonical pathways are involved in different aspects of the pathogenesis of RA.182, 183 For example, inflammatory bone loss in RA patients involves the abnormal generation and activation of osteoclasts, and the occurrence of osteoclasts requires RANK, which can stimulate the canonical and noncanonical NF-κB pathways in osteoclast precursor cells.184-186 In addition to the participation of osteoclasts, the pathogenesis of RA also involves many cell types, including innate immune cells, inflammatory T cells, B cells, and synovial fibroblasts.187 NF-κB mediates the production of pro-inflammatory cytokines (such as TNFα, IL-1, and IL-6) of innate immune cells, promotes the recruitment of inflammatory cells, and causes joint inflammation.188, 189 In addition, the excessive production of inflammatory cytokines and the induction of osteoclasts promote the destruction of bone and cartilage and aggravate disease progression.190-192 In particular, as a key component of noncanonical NF-κB pathways, NIK is highly expressed in synovial endothelial cells of RA patients, and NIK enhances CXCL12 expression in endothelial cells to promote pathogenic angiogenesis and synovial inflammation.193, 194 Moreover, the study also found that NIK-deficient mice have resistance to antigen-induced arthritis caused by T cell.195, 196 As mentioned earlier, T cells are also involved in the pathogenesis of RA, especially Th17 cells, which can recruit synovial tissues, release pro-inflammatory cytokines in synovial tissues, and induce synovitis.130, 176 The inflammatory factors required for Th17-cell differentiation (such as IL-1, IL-6, and IL-23) are induced by NF-κB.4, 176, 197 B cells are also involved in the pathogenesis of RA. In addition to producing autoantibodies, B cells regulate other immune cells and produce cytokines. Studies have found that the level of the B-cell-activating factor cloning to the tumor necrosis factor family (BAFF) in serum and synovial fluid of RA patients is usually increased, which is associated with the severity of the disease, while BAFF mainly activates noncanonical NF-κB pathway to facilitates survival and maturation of B cells.198, 199
Because NF-κB functions many aspects of RA, inhibiting NF-κB is a potential therapeutic target for RA.199, 200 It is well accepted that the biological agents such as anti-TNFα-neutralizing antibodies (etanercept, infliximab, and adalimumab, etc.) and anti-IL-6-neutralizing antibody (tocilizumab) target NF-κB pathway to prevent joint destruction of RA patients.201 Recent studies have found that iguratimod (IGU) is a potential treatment of RA. IGU is a new type of disease-modifying antirheumatic drug, which inhibits the production of immunoglobulin by inhibiting NF-κB without affecting the proliferation of B cells, the production of various inflammatory cytokines and osteoclasts.202, 203 In addition, salvianolic acid B and Ephedra gerardiana aqueous ethanolic extract have also been found to inhibit joint inflammation by suppressing NF-κB in animal models.204, 205 Drugs targeting NF-κB have been found to not only suppress inflammation but also effectively maintain bone mass and control the bone destruction of RA.176 Furthermore, the latest study tried to treat collagen-induced arthritis mice with an injection of β-arrestin-2 (βArr2) adenovirus and found that βArr2 effectively reduced ankle joint inflammation by inhibiting the NF-κB pathway and NLRP3 inflammasome.206 The latest clinical trials have also found that the activation of NF-κB in RA patients treated with β-d-mannuronic acid is significantly reduced, as well as the levels of IL-6 and TNFα in serum, reflecting the prospect of this treatment.207 The possibility of serious side effects caused by inhibiting NF-κB should be considered since serious adverse reactions such as embryonic death have been reported.208-211 We need to carry out further more basic and clinical research on the molecular mechanisms of RA and NF-κB to find the best drugs for RA treatment.
3.3.2 Inflammatory bowel disease (IBD)
IBD is a chronic, recurrent and non-infectious gastrointestinal (GI) disease, including ulcerative colitis (UC) and Crohn's disease, accompanied by long-term abdominal pain, diarrhea, and bloody stools.212-214 It is believed that the interaction between immunological, environmental, and genetic factors is regarded as the pathogenesis of IBD.215-219 In genetically susceptible individuals, when the balance of immune response to commensal bacteria is disturbed, the GI homeostasis is failed and the inflammation occurs.214 Both innate immunity and adaptive immunity play important roles in the pathogenesis of IBD; NF-κB is involved in both aspects of immunity as an important inflammatory signaling pathway in the pathogenesis of IBD.4, 215 Early studies have reported that constitutive NF-κB activation was found in the inflamed intestinal tissues of IBD patients.220, 221 In addition, NFKB1 genes encoding p105 and p50 were found to be associated with IBD.222-224 Mice carrying knock-in mutations of NFKB1 to block the production of p105 can develop IBD-like intestinal inflammation.154 Similarly, Nfkb2 also promotes the expression of RelA-driven pro-inflammatory genes in the intestinal epithelium and aggravates inflammatory cell infiltration and colon tissue damage.225 Consistent with these findings, decoy oligodeoxynucleotides targeting the DNA-binding activity of NF-κB showed potential therapeutic prospects in mice model.226 Genetic defects of negative regulators of NF-κB pathway can promote colon inflammation and even cancer. For example, in a colitis-related cancer model, compared with the control group, CYLD-deficient mice are more susceptible to colonic inflammation, and the incidence of tumors is significantly increased.227 Deletion of A20 in intestinal epithelial cells and myeloid cells induces ileitis and severe colitis.228 Although NF-κB participates in the pathogenesis of IBD, its functions in innate immune cells and epithelial cells are different. Loss of IKKβ in myeloid cells inhibits pro-inflammatory cytokines expression, attenuating colitis and colitis-related cancers.229 Contrary to the pro-inflammatory effect in myeloid cells, NF-κB has a protective effect in intestinal epithelial cells and is a key regulator of epithelial integrity and intestinal immune homeostasis.230 Using the conditional KO of IKKβ and IKKγ in intestinal epithelial cells, it shows the excessive and abnormal immune response in the intestine.229, 230 It has been confirmed that the IKKβ-dependent gene expression in the intestinal epithelium is essential for intestinal immune homeostasis by promoting mucosal immunity and limiting chronic inflammation.231 In the intestinal epithelium, NF-κB not only plays a protective role but also participates in the regulation of the intestinal tight junction barrier. The latest research shows that the destruction of matrix metalloproteinase-9 (MMP-9)-induced Caco-2 intestinal epithelial tight junction barrier is regulated by the NF-κB pathway.232 This finding suggests that the function of NF-κB in the intestinal epithelium is complex and to be further studied. As a mediator between the immune response and the intestinal commensal microbiota, TLRs also play a key role in maintaining intestinal homeostasis.233 The enhanced expression of TLRs leads to a hyper-activated downstream signal cascade including NF-κB and increased inflammatory cytokines and IBD.214, 233 Under normal physiological conditions, the expression level of TLR4 in the intestinal epithelium is low to maintain the integrity of the mucosa and protect against invading bacteria; however, its expression is upregulated in IBD, activating the downstream cascade and leading to inflammation.233, 234
The current treatment strategy for IBD is to control mucosal inflammation and inhibit overwhelming immune responses.235, 236 Commonly used drugs include 5-aminosalicylic acid, glucocorticoid, immune-suppressor, and biological agents.237 A biological agent that has attracted much attention is the anti-TNF antibody infliximab, which has shown good therapeutic effects in IBD.238, 239 The success of infliximab indicates that inhibiting the inflammatory target genes of NF-κB is one of the effective treatment strategies for IBD. In addition, for glucocorticosteroid treatment, the activity of NF-κB is decreased in UC patients who respond to the treatment, which may be due to the increase in the level of glucocorticoid receptors that regulate the activity of NF-κB.240 There are also some medicines in the development stages that show certain therapeutic prospects. A recent study found that butyrolactone-I reduces the production of IL-1, IL-6, and TNFα by inhibiting the TLR4/NF-κB and mitogen-activated protein kinases (MAPK) signaling pathways and reduces the inflammatory response of dextran sulfate sodium-induced colitis in mice.241 Another study found that a type of 2,3-dihydro-flavonoid has a beneficial effect on 2,4,6-trinitrobenzene sulfonic acid-induced colitis, possibly by inhibiting NF-κB p65 phosphorylation to reduce inflammatory mediators produce.242
3.3.3 Atherosclerosis
Atherosclerosis is a multi-step inflammatory process in the arterial wall, characterized by the accumulation of low-density lipoprotein (LDL) particles and immune cells in the subendothelial space. Both innate immunity and adaptive immunity are involved in this disease.243, 244 NF-κB regulates the expression of genes involved in the pathogenesis of atherosclerosis.245, 246 The first step in atherosclerosis is the injury and activation of endothelial cells. In endothelial cells, NF-κB mediates the expression of inflammatory cytokines, chemokines, and cell adhesion molecules and promotes the recruitment of monocytes to the arterial intima.4, 247, 248 Then, the recruited monocytes differentiate into macrophages, and after ingesting LDL particles, they will eventually become lipid-rich foam cells, which is a hallmark of the arterial lesion.245 In foam cells, NF-κB is activated, pro-inflammatory cytokines are secreted to enhance inflammation; the vascular smooth muscle cells are recruited to the inflamed sites, and finally atherosclerosis is formed.19, 245 Considering the pro-inflammatory function of NF-κB and inflammation play crucial roles in the process of atherosclerosis, inhibiting NF-κB may be a target for the prevention and treatment of atherosclerosis. Inhibition of NF-κB reduces the expression of inflammatory cytokines and chemokines and suppresses the induction of adhesion molecules in endothelial cells, to reduce the recruitment of macrophages to plaques and vascular inflammation. In an apolipoprotein E (ApoE)-deficient mouse model fed by a high-cholesterol diet, NF-κB was inhibited by ablation of IKKγ or increased expression of IκBα, and atherosclerotic plaque formation was significantly reduced.249 Studies have also found that in macrophages, the overexpression of trans-dominant and non-degradable forms of IκBα specifically inhibits NF-κB activation, which can reduce lipid load and foam cell formation.250 Similarly, one study has shown that the lack of IκBα in myeloid cells may promote atherosclerosis by reducing leukocyte recruitment to plaque.251 However, the role of macrophage-specific NF-κB in the development of atherosclerosis is still incompletely known.245
Targeting NF-κB-dependent inflammation is a very promising strategy for atherosclerosis treatment. A large clinical trial used anti-IL-1β antibody (canakinumab) for anti-inflammatory treatment in patients with atherosclerosis and previous myocardial infarction. The results showed that, compared with placebo, the recurrence rate of cardiovascular events was significantly reduced in the group with treatment.252 The results of this clinical trial demonstrate the effectiveness of anti-inflammatory treatments in the management of atherosclerotic diseases. Recent studies have also confirmed the therapeutic value of NF-κB as a target for atherosclerosis using animal models. The traditional Chinese medicine Qing-Xue-Xiao-Zhi formula inhibits TLR4-mediated NF-κB pathway, affects cholesterol metabolism and promotes lipid efflux, and inhibits macrophage-mediated inflammation, which has a therapeutic effect on atherosclerosis.253 Another clinical trial has also found that crocin may reduce the expression of lectin-like oxidized LDL receptor 1 and NF-κB by increasing expression of sirtuin 1 and 5′-adenosine monophosphate-activated protein kinase (AMPK), demonstrating the potential therapeutic value of coronary heart disease.254 The latest research has found that Paeonia lactiflora extract also exhibits a certain therapeutic potential for atherosclerosis. In vitro P. lactiflora extract can inhibit TNFα-induced nuclear translocation of NF-κB p65 from the cytoplasm and NF-κB activity; in vivo oral administration of P. lactiflora extract can improve TNFα-induced macrophages activation. The infiltration of immune cells to the vascular endothelium and the expression of Il6 and Tnfa in the mouse aorta contribute to the early stage of atherosclerosis.255
3.3.4 Corona virus disease 2019 (COVID-19)
In the past 2 years, COVID-19 has had a catastrophic impact on the health and lives worldwide. According to the current vaccination situation and drug development, this impact will continue for a certain time. COVID-19 patients show a wide range of clinical features, including cough and fever, and even some patients develop septic shock, acute respiratory distress syndromes, and multiple organ failure.256-258 Compared with asymptomatic patients or mildly symptomatic patients, the clinical manifestations of severe cases suggest excessive activation and imbalance of systemic inflammation.256, 259 In particular, cytokine storm syndrome (CSS) occurs in critically ill patients, with significantly increased cytokine and chemokine.260-262 The overwhelming production of these cytokines is related to the severity of COVID-19, and the NF-κB signaling pathway plays an important role in it.263, 264 Activated NF-κB upregulates the production of inflammatory cytokines (such as TNFα, IL-1β, IL-6, and IL-8), which is essential for a comprehensive cytokine storm.265, 266 Multiplication of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) promotes the production and accumulation of dsRNA.267 Protein kinase R (PKR) can trigger the innate immune response and terminate the translation process to prevent replication of the virus in infected cells. PKR combined with dsRNA can activate IKK, trigger the degradation of IκBα and IKKβ, and activate canonical NF-κB pathway.268, 269 SARS-CoV-2 spikes and nucleocapsid (N) protein induced NF-κB activation, which in turn significantly increased the expression of pro-inflammatory cytokines. The spike protein subunit 1 of SARS-CoV-2 has been identified as an effective cytokine storm inducer in COVID-19.270 This subunit has a high binding affinity to the angiotensin-converting enzyme 2 receptor and can activate NF-κB to produce cytokines.271 In addition, SARS-CoV-2 N protein can also promote NF-κB activation and increase the expression of cytokines by recruiting TAK1 and IKK complexes after binding to viral RNA.262 SARS-CoV-2 mediates inflammation by activating NF-κB, so the development of drugs that inhibit NF-κB is currently considered to be one of the potential treatment strategies for COVID-19.272 A clinical trial used the BTK inhibitor acalabrutinib to treat severe COVID-19 patients, and the result showed that C-reactive protein and IL-6 levels were reduced, and patients' oxygen saturation improved.273 Another study used diosmectite in the SARS-CoV-2 model, as diosmectite can bind to SARS-CoV-2 components and inhibit NF-κB activation and CXCL10 secretion and inhibit downstream inflammation, indicating the potential value of diosmectite for COVID-19-related diarrhea.274 It is worth noting that traditional Chinese medicine has shown considerable prospects in the treatment of COVID-19. A clinical study found that Yindan Jiedu granules may inhibit the production of inflammatory cytokines by targeting the NF-κB pathway, thereby shortening the course of COVID-19 and delaying its progression.275 In in vitro experiments, it was also found that another traditional Chinese medicine, Liu Shen capsule, can inhibit SARS-CoV-2 infection by downregulating cytokine-induced virus expression and regulating the activity of the NF-κB/MAPK signaling pathway.276 Despite the intensive efforts and large-scale drug screening, an effective and safe antiviral treatment plan has not been developed. Nucleotide analogs inhibit RNA-dependent RNA polymerase (RdRp) to suppress dsRNA-induced NF-κB activation and prevent virus replication. One example is remdesivir, which shows a certain clinical effect, compared to a placebo.277 In addition, the latest drug development is the oral antiviral drugs molnupiravir and paxlovid, which have shown good treatment efficiency in clinical tries.278, 279 As an important inflammation-related pathway, NF-κB is still a potential therapeutic target for COVID-19 treatment, especially for critically ill patients and CSS.
4 NF-ΚB AND CANCER
4.1 Activation of NF-κB in cancer
v-Rel is an oncogene of avian Rev-T retrovirus, isolated from a turkey liver lymphoma by Theilen and Robinson in 1958,280 which is the earliest evidence that NF-κB is related to cancer. However, the carcinogenicity of the rel gene is only found in birds, not in humans. Although the gene rel is not a bona fide oncogene, the constitutive-activated NF-κB has been examined in most tumors, which participates in a variety of cancer-related biological procedures.16
In most cancers, the activation of NF-κB is enhanced, and this enhancement in NF-κB activation is often due to increased stimuli of the NF-κB pathway, such as increased TNFα and IL-1 in the tumor microenvironment.281, 282 On the other hand, NF-κB has a certain tumor-suppressing function confirmed using tumor cell line and mouse models but not fully demonstrated in human cancers yet.283, 284 Mutations of NF-κB are found in many cancers, although the mutation frequency of RelA and RelB is much lower than that of REL, p50, and p52.7 It has been reported that REL gene amplification in lymphoma leads to an increased expression of REL protein, as well as a C-terminal truncated p100 protein that lacks the ANK repeat inhibitory sequence.285-287 In addition to NF-κB family proteins, mutations have been found in the core components and regulators of the NF-κB pathway, which affect both canonical and noncanonical NF-κB activation. For example, studies have identified a loss-of-function mutation of IκB family proteins in lymphoma, glioblastoma, and nasopharyngeal carcinoma.288-291 Meanwhile, studies have also reported that mutations of IKKα and IKKβ have been found in several cancers,292-294 although the mutation of IKK is relatively rare. The reason may be that IKK also participates in many other signaling pathways except for NF-κB.295 The functional versatility of IKK may reduce the possibility of mutations. Mutations in critical regulating molecules that affect the activation and function of NF-κB are identified in tumor cells. Considering NF-κB as a family of the conserved transcription factor, the most common mutations that enhance NF-κB signaling may occur in the upstream molecules and downstream target genes.7 In diffuse large B-cell lymphoma (DLBCL) and multiple myeloma (MM), proteins such as CD79 and MyD88 have been found to activate NF-κB through gain-of-function mutations. It was also found that loss-of-function mutations of CYLD, A20, TRAF3, and other negative regulators also cause abnormal activation of NF-κB.296-301 Similarly, TNFα coded by an NF-κB target gene TNFA acts as a strong activator of NF-κB, functions in many tumor cells with constitutive activation of NF-κB in an autocrine manner (usually stromal).301, 302 Taking specific tumor types as an example, DLBCL is the most studied malignant tumor with NF-κB mutation.297 Studies have shown that mutations in the three proteins (REL, IκB, p300) are involved in the NF-κB activation in human B-cell lymphoma cell line RC-K8.287, 288 Most B-cell malignancies not only have an oncogenic driving force activated by mutated NF-κB but also have mutations in many other pathways. The subtype of DLBCL lymphoma with the activation of the canonical NF-κB pathway is named by the activated B-cell (ABC) subtype. Meanwhile, the abnormal activation of the noncanonical NF-κB pathway is also detected more in other DLBCL subtypes.299, 300 The mutations in the NF-κB signaling pathway involved in cancers are summarized in Table 1.
| Cancer type | Protein | Gene | Mutation type | Effect | Ref. |
|---|---|---|---|---|---|
| Solid | |||||
| Bladder cancer | TRAF2/3 | TRAF2/3 | Mutations, deletions, amplifications | Decrease | 7, 426 |
| TRAF4 | TRAF4 | Mutations, amplifications | Increase | 7, 426 | |
| Breast cancer | TRAF4/5/6 | TRAF4/5/6 | Mutations, amplifications | Increase | 7, 426 |
| Cervical cancer | p50/p105 | NFKB1 | Point mutations | Increase | 427 |
| TRAF3 | TRAF3 | Mutations, deletions, amplifications | Decrease | 7, 426 | |
| Colon cancer | TRAF1 | TRAF1 | Point mutations | Increase | 428 |
| TRAF6 | TRAF6 | Mutations, amplifications | Increase | 7, 426 | |
| Cylindromatosis | CYLD | CYLD | Mutations, deletions | Decrease | 69 |
| Esophageal cancer | TRAF4/5/6 | TRAF4/5/6 | Mutations, amplifications | Increase | 7, 426 |
| Gastric cancer | p50/p105 | NFKB1 | Point mutations | Increase | 3 |
| MYD88 | MYD88 | Mutations, deletions | Increase | 299, 429 | |
| TRAF1 | TRAF1 | Point mutations | Increase | 7, 426 | |
| TRAF2/3 | TRAF2/3 | Mutations, deletions, amplifications | Decrease | 7, 426 | |
| TRAF6 | TRAF6 | Mutations, amplifications | Increase | 7, 426, 430 | |
| Glioblastoma | IκBα | NFKBIA | Mutations, deletions | Decrease | 290, 431 |
| Head and neck cancer | TRAF2/3 | TRAF2/3 | Mutations, deletions, amplifications | Decrease | 7, 426 |
| TRAF6 | TRAF6 | Mutations, amplifications | Increase | 7, 426 | |
| Liver cancer | p50/p105 | NFKB1 | Point mutations | Increase | 3 |
| TRAF5/6 | TRAF5/6 | Mutations, amplifications | Increase | 7, 426 | |
| Lung cancer | TRAF3 | TRAF3 | Mutations, deletions, amplifications | Decrease | 7, 426 |
| TRAF4/5/6 | TRAF4/5/6 | Mutations, amplifications | Increase | 7, 426 | |
| Melanoma | TRAF1 | TRAF1 | Point mutations | Increase | 426, 432 |
| TRAF2/3 | TRAF2/3 | Mutations, deletions, amplifications | Decrease | 7, 426 | |
| TRAF4/5 | TRAF4/5 | Mutations, amplifications | Increase | 7, 426 | |
| Nasopharyngeal carcinoma | IκBα | NFKBIA | Mutations, deletions | Decrease | 291 |
| A20 | TNFAIP3 | Point mutations | Decrease | 291 | |
| CYLD | CYLD | Mutations, deletions | Decrease | 69 | |
| TRAF3 | TRAF3 | Mutations, deletions, amplifications | Decrease | 7, 426 | |
| Ovarian cancer | p50/p105 | NFKB1 | Point mutations | Increase | 3 |
| TRAF2/3 | TRAF2/3 | Mutations, deletions, amplifications | Decrease | 7, 426 | |
| TRAF4/5/6 | TRAF4/5/6 | Mutations, amplifications | Increase | 7, 426 | |
| Pancreatic cancer | TRAF4 | TRAF4 | Mutations, amplifications | Increase | 7, 426 |
| Prostate cancer | IKKβ | IKBKB | Point mutations | Increase | 293 |
| TRAF2 | TRAF2 | Mutations | Decrease | 7, 426 | |
| TRAF5/6 | TRAF5/6 | Mutations, amplifications | Increase | 7, 426 | |
| Uterine cancer | TRAF2/3 | TRAF2/3 | Mutations, deletions, amplifications | Decrease | 7, 426 |
| TRAF4/5/6 | TRAF4/5/6 | Mutations, amplifications | Increase | 7, 426 | |
| Hematologic malignancy | |||||
| Chronic lymphocytic leukemia | IκBε | NFKBIE | Deletions, point mutations | Decrease | 433 |
| BCL3 | BCL3 | Translocations | Increase | 434 | |
| Chronic myelogenous leukemia | TRAF1 | TRAF1 | Point mutations | Increase | 435 |
| Diffuse large B-cell lymphoma | p52/p100 | NFKB2 | C-terminal truncations | Increase | 285 |
| REL | REL | Point mutations, amplifications, | Increase | 287 | |
| REL | REL | Truncations | Decrease | 287 | |
| IκBα | NFKBIA | Mutations, deletions | Decrease | 285 | |
| IKKβ | IKBKB | Point mutations | Increase | 293 | |
| CD79A/B | CD79A/B | Point mutations | Increase | 436 | |
| BCL10 | BCL10 | Point mutations, chromosomal translocations | Increase | 437 | |
| LUBAC | HOIP, HOIL, SHARPIN | Point mutations | Increase | 438 | |
| MALT1 | MALT1 | Chromosomal translocations, point mutations, amplifications | Increase | 439 | |
| A20 | TNFAIP3 | Point mutations | Decrease | 440 | |
| CARD11 | CARMA1 | Chromosomal translocation; point mutation | Increase | 441 | |
| p300 | EP300 | Deletions | Decrease | 442, 443 | |
| TRAF2 | TRAF2 | Mutations | Decrease | 444 | |
| TRAF3 | TRAF3 | Mutations, deletions, amplifications | Decrease | 7, 426 | |
| CBP | CREBBP | Deletions | Decrease | 442, 443 | |
| MYD88 | MYD88 | Mutations, deletions | Increase | 299 | |
| Hodgkin lymphoma | NIK | MAP3K14 | Gene fusion, point mutations | Increase | 31 |
| Leukemia | CARD11 | CARMA1 | Chromosomal translocation; point mutation | Increase | 441 |
| p300 | EP300 | Deletions | Decrease | 442, 443 | |
| CBP | CREBBP | Deletions | Decrease | 442, 443 | |
| Mantle cell lymphoma | TRAF2 | TRAF2 | Mutations | Decrease | 444 |
| Marginal zone lymphoma | TRAF3 | TRAF3 | Mutations, deletions, amplifications | Decrease | 7, 426 |
| Multiple myeloma | RELA (p65) | RELA | Point mutations | Increase | 445 |
| IκBβ | NFIKBB | Point mutations | Decrease | 446 | |
| IKKβ | IKBKB | Point mutations | Increase | 293 | |
| NIK | MAP3K14 | Gene fusion, point mutations | Increase | 446 | |
| CYLD | CYLD | Mutations, deletions | Decrease | 69 | |
| TRAF3 | TRAF3 | Mutations, deletions, amplifications | Decrease | 7, 426 | |
| B-cell lymphoma | CD79A/B | CD79A/B | Point mutations | Increase | 436 |
| p52/p100 | NFKB2 | C-terminal truncations | Increase | 285 | |
| BCL10 | BCL10 | Point mutations, chromosomal translocations | Increase | 437 | |
| MALT1 | MALT1 | Chromosomal translocations, point mutations, amplifications | Increase | 439 | |
| A20 | TNFAIP3 | Point mutations | Decrease | 440 | |
| CARD11 | CARMA1 | Chromosomal translocation; point mutation | Increase | 441 | |
| T-cell lymphoma | p52/p100 | NFKB2 | C-terminal truncations | Increase | 285 |
| Waldenström's macroglobulinemia | MYD88 | MYD88 | Mutations, deletions | Increase | 447 |
| TRAF3 | TRAF3 | Mutations, deletions, amplifications | Decrease | 7, 426 | |
- Abbreviations: Bcl3, B-cell leukemia/lymphoma 3; CARD11, caspase recruitment domain-containing protein 11; CARMA1, CARD-containing MAGUK protein 1.; CBP, CREB binding protein; CYLD, cylindromatosis; HOIL, heme-oxidized IRP2 ubiquitin ligase; HOIP, HOIL-1L-interacting protein; IKKβ, IκB kinase β; IκB, inhibitor of NF-κB; LUBAC, linea ubiquitin assembly complex; MALT1, mucosa-associated lymphoid tissue lymphoma translocation protein 1; MyD88, myeloid differentiation primary response gene 88; NIK, NF-κB-induced kinase; SHARPIN, shank-associated RH domain interactor; TRAF, TNF-R-associated factor.
4.2 NF-κB and cancer cell survival and proliferation
One important function of the NF-κB is to regulate cell survival. In tumor cells, the activation of NF-κB usually leads to impaired cell apoptosis.303 The deletion or inactivation of genes encoding key molecules in the NF-κB pathway promotes cell apoptosis. For example, inactivation of the v-Rel oncogene leads to apoptosis of transformed lymphocytes, and KO of the Rela gene leads to apoptosis of mouse fibroblasts and embryonic hepatocytes under the TNFα stimulation.210, 304 NF-κB target genes encode anti-apoptotic molecules such as Bcl2, Bcl-xL, and inhibitor of apoptosis (IAP). Upregulation of NF-κB activity has been detected in various tumor cells, and the expression of target genes of anti-apoptotic NF-κB is also increased.7 It is noteworthy that NF-κB is not only anti-apoptotic, the activation of NF-κB is also required for cell apoptosis. Studies have found that inhibition of NF-κB reduced the apoptosis induced by drugs in many tumor cells.305-307 Therefore, NF-κB may also be a cell type-specific repressor of anti-apoptotic genes or an activator of pro-apoptotic genes.308-310 In addition, the recent researches suggest that many molecules (such as various anti-cancer drugs, non-coding RNA, microRNA, etc.) regulate the apoptosis of cancer cell through the NF-κB pathway and other coordinated pathways (such as AMPK, AKT, glycogen synthase kinase 3, metabolism pathways).311-317
In addition to apoptosis, proliferation is also the fundamental cellular procedure. NF-κB activates genes that regulate cell proliferation, such as cyclin D1/D2/D3.318-320 In addition to cyclins, NF-κB also regulates cell proliferation by induction of critical enzymes. The expression of E3 ubiquitin ligase mouse double minute 2 protein is NF-κB-dependent, which affects the stability of p53 and cell proliferation.321 In inflammatory immune cells such as macrophages and neutrophils, the activation of NF-κB activates the expression of inflammatory cytokines such as TNFα, IL-1β, and IL-6, thereby promoting the proliferation of malignant cells and tumor stromal cells.16, 322, 323 Taken together, it has been well-accepted that NF-κB plays an important role in the regulation of tumor cell proliferation and apoptosis, and its functions and mechanisms are multi-faceted.
4.3 NF-κB and tumorigenesis
The journal from tumorigenesis to tumor progression is a long-term procedure controlled by multiple factors. Most tumors usually require multiple gene mutations.324 Inflammation and NF-κB affect the tumor occurrence by promoting the production of reactive oxygen species and reactive nitrogen species, leading to DNA damage and carcinogenic mutations.282 Chronic inflammation and NF-κB also cause chromosomal instability, aneuploidy, and epigenetic changes, resulting in the occurrence and progression of tumors.282 In addition, one of the mechanisms by which NF-κB promotes tumorigenesis is that when cells with damaged DNA strands enter the cell cycle, NF-κB activation integrates mutations into the two DNA strands and transmits them to daughter cells.325, 326 Another mechanism by which NF-κB stimulates tumorigenesis is to induce mutant-related enzymes such as activation-induced cytidine deaminase that deaminates cytosine residues and causes the conversion of cytosine to thymine, increasing mutations probability.327 Furthermore, by preventing p53-dependent apoptosis, NF-κB activation increases the number of DNA-damaged cells that accumulate oncogenic mutations.328 In addition to gene mutation, viral infection is the risk factor leading to tumorigenesis, such as hepatitis B virus (HBV), human papillomavirus, and Epstein–Barr virus (EBV), and so forth. Some viruses promote tumorigenesis through chronic NF-κB-dependent inflammation or the continuous activated transcriptional activity induced by viral genes. Viruses also directly encode NF-κB-stimulating factors. EBV that causes B-cell lymphoma and nasopharyngeal carcinoma encode LMP1 protein that functions as CD40 homolog to prevent apoptosis of EBV-infected B-cell by upregulating NF-κB activation.329 Kaposi's sarcoma-associated herpesvirus that causes sarcoma and lymphoma encodes viral FLICE inhibitory protein (vFLIP) that hijacks both canonical and noncanonical NF-κB pathways promoting cell survival and proliferation.329 Besides direct transcribing cell proliferation-related genes, NF-κB also induces the expression of proinflammatory cytokines such as IL-1β, IL-6, and TNFα, which play a key role in the NF-κB-dependent tumor cell proliferation.330 Meanwhile, NF-κB also regulates apoptosis of tumor cells. NF-κB blocks the death of tumor cells induced by the activation of oncogenes Ras.331 NF-κB-dependent Rac guanosine triphosphatase effectively inhibits the p53-independent apoptosis response induced by high levels of Ras activity. Rac mutants that could not activate NF-kB are defective in inhibiting Ras-induced apoptosis. In particular, under hypoxic conditions, NF-κB enhances the expression of hypoxia-inducible factor 1α, thereby enhancing the early survival of tumor cells.332, 333
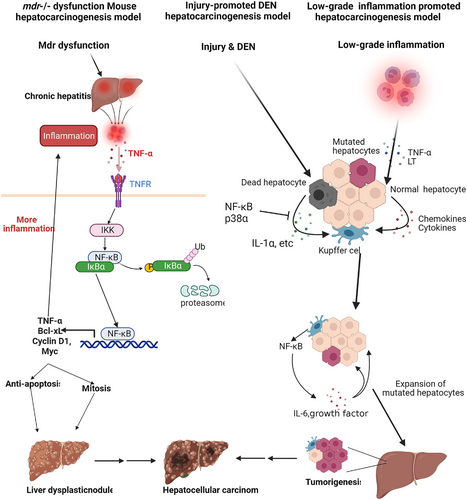
NF-κB is important for tumor angiogenesis.334 Among the singling pathways contributing to tumor angiogenesis, NF-κB is critical to activate angiogenesis-related genes. Study has confirmed that B7-H3 activates NF-κB pathway to upregulate the expression of vascular endothelial growth factor-A (VEGFA) in colorectal cancer and promotes angiogenesis.335 In contrast, NF-κB interacting long noncoding RNA (NKILA) was found to inhibit the IL-6 production and angiogenesis through NF-κB.336 NF-κB in cancer cells promotes EMT.337 The expression of major EMT molecules (including Twist, Zinc finger transcription factor Snail2 (Slug) and Smad-interacting protein1) is NF-κB-dependent, which initiate EMT and identify malignant phenotypes by enhancing the stemness and migration of cancer cells.338, 339 Additionally, NF-κB activation also promotes EMT through other mechanisms, such as the matrix-degrading enzyme.340 MMPs induced by NF-κB promote the release of TGF-β, EMT process, and hypoxia that contribute to metastatic dissemination.341-343 In addition, NF-κB and cytokines (such as VEGF and TGF-β) can directly stimulate the expression of metastasis-related genes and promote tumor metastasis, such as exercise-inducing factors and chemokines.344, 345 Inflammation and NF-κB can also directly stimulate metastatic dissemination through EMT, increase the extravasation of cancer cells into the blood and lymphatic vessels, and prevent the death of connective tissue tumor cells.346 Taking liver cancer as an example, the functions of NF-κB in tumorigenesis are schematically shown in Figure 3.
4.4 NF-κB and cancer stem cells (CSCs)
CSCs are malignant cells that have the ability to self-renew and differentiate into highly differentiated malignant cells. CSCs are the major reason for cancer recurrence, metastasis, and treatment resistance.347, 348 CSCs were first identified in leukemia and then isolated as CD34+CD38– cells in the 1990s.349, 350 The following studies indicate that in other hematologic malignancies and solid tumors, CSCs express other different surface markers (such as CD133, nestin, and CD44).351, 352 The activities of cancer stem cells are controlled by many intracellular and extracellular factors and various signaling pathways. The functions of NF-κB pathway in CSCs are complicated. NF-κB is constitutively activated in various CSCs (including leukemia, glioblastoma, prostate, ovary, breast, pancreatic, and colon cancer), which mediates inflammation, cell proliferation, survival, maintenance, and expansion.353 NF-κB could work alone or synergize with other signaling pathways to induce and promote the self-renewal, proliferation, and metastasis of CSCs by mediating the expression of stem-cell-related transcriptional factors and genes (such as Nanog, Sox2, Olig2, CD44, NKX3.1 and Krüppel-like factor 4 (KLF4)).354 In breast cancer, NF-κB activation causes CSC proliferation by activating Notch signaling in a cell-involuntary way.355 In addition, high levels of NIK also induce the activation of the noncanonical NF-κB pathway to regulate the self-renewal and metastasis of breast CSCs.356 Therefore, drugs targeting NF-κB pathway could be used to inhibit the proliferation and metastasis of cancer stem cells. The study has shown that in breast cancer stem cells, the anti-alcoholism drug disulfiram inhibits TGF-β through the extracellular regulated protein kinases(ERK)/NF-κB/Snail pathway to induce tumor metastasis.357 Sulforaphane also inhibits the self-renewal of triple-negative breast cancer stem cells by inhibiting NF-κB p65 subunit translocation and down-regulating p52 and its transcriptional activity.358 The canonical NF-κB pathway enhances the expression of the transcription factor Sry-related HMG box 9 (Sox9), which is associated with enhanced pancreatic CSCs and invasiveness.359 In ovarian cancer, CD44+ CSCs enhance self-renewal and metastasis by upregulating the expression of RelA, RelB, and IKKα and enhancing the activation of p50/RelA dimer.360 In colorectal cancer, the inflammatory mediator prostaglandin E2 activates NF-κB through prostaglandin E Receptor 4-phosphoinositide 3-kinase to promote the formation, maintenance, and metastasis of CSCs.361 The transcription factor Foxp3 also interacts with NF-κB, to inhibit the expression of the NF-κB target gene COX2, and affect the self-renewal and metastasis of colorectal CSCs.362
4.5 NF-κB and tumor microenvironment
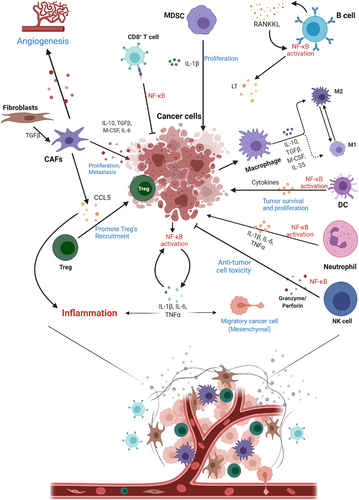
Tumorigenesis’ progress and metastasis rely on the environment where the tumor cells are located. The tumor microenvironment is composed of tumor cells, a variety of stromal cells, and immune cells, together with cytokines, chemokine, and other mediators, especially endothelial cells, cancer-associated fibroblasts (CAFs), myeloid-derived suppressor cells (MDSCs), and other numerous immune cells are critical for the tumor microenvironment.363-365 NF-κB functions as the key regulator in many types of cells to shape the tumor microenvironment.
Cytokines produced by stromal cells, cancer cells, and immune cells are the key soluble factors for tumorigenesis, metastasis, and inflammation.330 Tumorigenesis is associated with tumor-promoting cytokines, so it is important to understand the correlation between NF-κB and pro-tumorigenic cytokines. Tumor necrosis factor α (TNFα) is also one of the well-studied tumor-promoting cytokines, and its expression is enhanced in many cancers, which often indicates a poor prognosis.302, 366, 367 TNFα is mainly produced by activated neutrophils and macrophages, which induces other proinflammatory cytokines, including IL-6 and IL-1β, and accelerates tumorigenesis.302 Similar to TNFα, IL-6 is another important and abundant proinflammatory cytokine in the tumor microenvironment. The functions of this NF-κB-dependent cytokine on inflammation and tumorigenesis have been well studied.229, 367, 368 IL-6, mainly produced by malignant tumor cells and activated immune cells, initiates cancer-related inflammation and stem cell expansion in an autocrine manner.367, 369 In addition, IL-1α/β are also key proinflammatory cytokines produced by cancer cells and immune cells, which are NF-κB-dependent and promote the activation of NF-κB and MAPK pathways and tumorigenesis.370, 371 IL-17A activates NF-κB and MAPK signaling pathways, thereby promoting tumorigenesis.372-374 The other IL-1 family cytokine, IL-33 is mainly expressed by epithelial cells, fibroblasts, and tumor cells, with a crucial function in allergy, autoimmunity, inflammation, and cancer.375, 376 Another important cytokine is TGF-β, which is produced by a variety of cells, including fibroblasts, myeloid cells, T cells, and cancer cells. TGF-β is essential for the differentiation of Treg and TH17 cells, making it a powerful inducer of tumor invasion and metastasis.330, 343
NF-κB drives chemokine expression in tumor cells, stromal cells, and immune cells in the tumor microenvironment, especially CAFs.377-379 The activation of NF-κB and other transcription factors (such as AP1 and STAT3) induces the expression of chemokines, which recruit more immune cells and further aggravate the inflammatory response.380, 381 Meanwhile, chemokines are important to stimulate the growth and metastasis of primary tumors, synthesizing growth factors, and angiogenesis. Although the functions of chemokines are complicated and uncertain in tumorigenesis and metastasis, chemokines still are important targets for cancer immunotherapy.364, 382, 383 For example, chemokine (C-C motif) ligand 5 (CCL5) induces the formation of eukaryotic initiation factor 4F translation initiation complex in an mechanistic target of rapamycin (mTOR)-dependent way, which mediates the quick upregulation of cyclin D1, c-Myc, and defender against cell death-1 (Dad-1) protein expression to promote tumor cell proliferation in breast cancer.384 In addition, in human pancreatic cancer and mouse pancreatic tumor models (Pan02), the CCL5 level on tumor cells is elevated, while CD4+Foxp3– effector T cells preferentially express C-C chemokine receptor 5 (CCR5). When the CCR5/CCL5 signal is disturbed, either by inhibiting CCL5 expression on tumor cells or systemically administrating CCR5 inhibitors, the migration of Treg cells to the tumor microenvironment is reduced, which indicates that the chemokine CCL5 is required for Treg cells migration.385 Tumor-related cytokines are mainly expressed by inflammatory cells, such as tumor-associated macrophages (TAMs) and neutrophils. NF-κB is mainly activated in these cells to induce the expression of cytokines (TNFα, IL-1β, IL-6, etc.), thereby promoting tumor survival and proliferation.16, 323 As the most abundant immune cells in the microenvironment, macrophages produce inflammatory cytokines and chemokines and produce proteases such as cysteine cathepsins, involved in activating cytokines to promote tumor development.330, 365 M1 macrophages activated by IFN-γ and LPS can produce proinflammatory cytokines, chemokines, and enzymes to promote inflammation. In contrast, M2 macrophages induced by IL-4, IL-10, and IL-13 can inhibit inflammation by releasing anti-inflammatory mediators.92, 386, 387 M1 macrophages promote inflammation, while M2 macrophages create an immunosuppressive tumor microenvironment. The increase in p50 activity determines the M1 to M2- polarization of macrophages.387-389 Inhibiting NF-κB transforms M2 macrophages to M1 macrophages because the polarization of M1 macrophages through IL-1R and MyD88 into M2 macrophages requires IKKβ-mediated activation of NF-κB. Moreover, the impaired NF-κB activation in TAMs also promotes the tumor-killing activity of macrophages. When NF-κB signaling is inhibited in TAMs, they become M1 phenotype with anti-tumor cytotoxicity.390 NF-κB could be a target for manipulating the phenotype of macrophages in the tumor microenvironment.
DCs are also important immune cells modulating anti-tumor immunity in the tumor microenvironment. The canonical NF-κB pathway in DCs can be inhibited by signals from the immune checkpoint molecule programmed cell death protein 1 (PD-1), thereby inhibiting the production of cytokines.391 In contrast, the ligand of checkpoint like programmed cell death 1 ligand 1 (PD-L1) is an NF-κB target gene. The upregulation of PD-L1 expression in cancer cells relies on NF-κB activation triggered by many stimuli and activators, including oncogenes, stress, inflammatory cytokines, and chemotherapeutic drugs.392 In addition to macrophages and DCs, it has also been reported that IL-1β induces NF-κB activation in MDSCs to suppress the function of tumor microenvironment (TME), leading to tumor proliferation.393 In natural killer (NK) cells that directly kill tumor cells to exert anti-tumor activity, the expression of cytotoxic effector molecules (such as perforin and granzyme B) ia also affected by NF-κB.394-396 The activation of NF-κB in NK cells can be stimulated by exogenous anti-cancer drugs, like paclitaxel.397
As the important components of the tumor microenvironment, T cells and B cells in the tumor microenvironment could have tumor-promoting or anti-tumor functions.398 As mentioned above, the important stimuli of the NF-κB pathway include TCR and BCR. The activation of conventional T cells requires the participation of the canonical NF-κB pathway, which is required for CD8+ T cell proliferation and anti-tumor immune response.399, 400 The development of Treg cells requires the participation of p65 and Rel. Rel is not only essential for the optimal steady-state expansion of Treg cells in peripheral blood150 but also for the development of thymic Treg cells. p65 is crucial for Tregs maturation, and the maintenance of immune tolerance401 IKKβ-dependent NF-κB is activated in B cells that induce a cytokine LT, a heterotrimeric member of the TNF family that activates IKKα.402 The LT produced by B cells can activate IKKα in tumor cells. IKKα phosphorylates a site of the transcription factor E2F transcription factor 1 (E2F1) to promote E2F1 translocation and recruit to the target of the Bmi1 gene. The IKKα–E2F1–Bmi1 cascade activated by B cells controls prostate regeneration and tumor recurrence and regulates the renewal function of tumor stem cells.403
The component that cannot be ignored in the tumor microenvironment is fibroblasts. Normal fibroblasts undergo changes in a self-intrinsic way, and under the stimulation of tumor-induced alterations tissue structure, TGF-β, and hypoxia, they become tumor-associated fibroblasts (CAFs) and express a large number of inflammatory factors and chemokines.378, 379 For example, IL-1β is induced by the NF-κB signaling pathway to promote inflammation, cancer cell proliferation, angiogenesis, and tumor metastasis.404 For example, in pancreatic ductal adenocarcinoma, CAFs mediate the exosomal metastasis and paracrine of tumor cells through producing cytokines (such as GM-CSF and IL-6), and this process requires the participation of NF-κB. In breast cancer, locked nucleic acid (LNA)-i-miR-221 inhibits miR-221-mediated NF-κB activation to reduce the secretion of tumor-promoting cytokines of CAFs.405 In brief, NF-κB has complex functions on the different types of cells in the tumor microenvironment and might become a potentially effective therapeutic target. The function of the NF-κB in the tumor microenvironment is shown in Figure 4.
4.6 NF-κB and inflammation in cancer
The relationship between inflammation and tumor has become an important field of cancer research. It is well-studied that inflammation is associated with autoimmune diseases, infection, and cancers.5 The well-established examples of inflammation leading to cancer are HBV infection and hepatocellular carcinoma (HCC), and chronic Helicobacter pylori infection and mucous MALT lymphoma and gastric cancer.25, 330 NF-κB is essential for the activation, differentiation, and effector functions of inflammatory T cells and innate immune cells and participate in the regulation of inflammasomes.406
In addition to NF-κB, the activation of other transcription factors such as AP1 and STAT3 can also induce the expression of chemokines, which recruit more immune cells (including T cells, B cells, macrophages, neutrophils, etc.) to aggravate the inflammatory response further.380, 407 As early as 2004, two studies showed the key roles of NF-κB in inflammation-driven colitis-associated cancer and HCC.229, 408 These results indicate that tumorigenic pathogens cause chronic infection and inflammation, and chronic inflammation sequentially leads to malignant tumors by increasing cellular stress response and recruiting inflammatory immune cells.5, 409 However, chronic inflammation does not necessarily lead to cancer. As a chronic inflammatory disease, IBD is associated with colorectal cancer, but RA and psoriasis are chronic inflammatory diseases without obvious tumor outcomes.410 Another relevant evidence is that the loss of IKKβ in myeloid cells suppresses experimental colitis and colitis-related cancers.229 Another area worthy of attention is tertiary lymphoid tissues. Clinical studies have shown that there are tertiary lymphoid tissues in the tumor microenvironment, and the presence of tertiary lymphoid tissues suggests a better prognosis.411, 412 The formation of tertiary lymphoid tissues is achieved by LTβR-mediated noncanonical NF-κB activation pathway to induce the expression of adhesion molecules and chemokines (like CCL19, CCL21, CXCL12, and CXCL13).413, 414 In general, the relationship between the NF-κB signaling pathway and inflammation is profound and complex, and the precise mechanisms of NF-κB, inflammation, and cancer in the current context need to be further studied. The functions of NF-κB in the cross-talking between immune cells and tumor cells are shown in Figure 5.
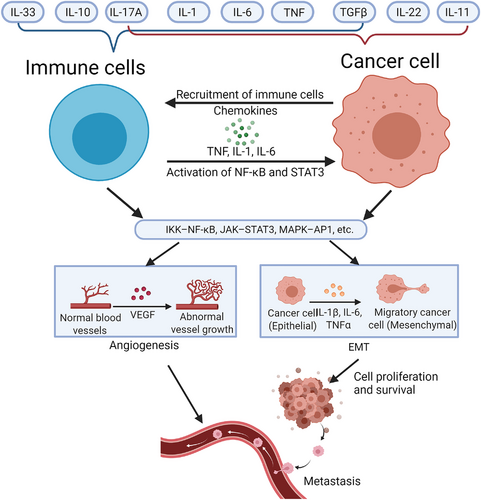
4.7 The therapeutic application of NF-κB in cancer
With emerging research on NF-κB and tumors, it is generally believed that NF-κB is a valuable target for human cancer treatment. Considering the tumor-promoting effects of NF-κB, the current therapeutic strategy is inhibiting the activation of NF-κB. These inhibitors include microbial and viral proteins, microRNA, non-coding RNA, antioxidants, engineered active peptides, and various natural products to downregulate the canonical and noncanonical NF-κB pathways.415 Due to the complexity of upstream stimulators and downstream target genes of NF-κB, more than 1000 inhibitors could block the NF-κB signaling pathway.416 Most of these inhibitors are found to have certain anti-tumor effects using tumor cell models or animal models; their effects on human cancer treatment are unknown. Efforts have been made to develop specific and effective inhibitors with few side effects. A good example is bortezomib, a proteasome inhibitor, which has shown the inhibitory effect in MM.417 As mentioned earlier, NF-κB is continuously activated in myeloma. Therefore, as a proteasome inhibitor, bortezomib was conceived to inhibit the degradation of ubiquitinated IκB, allowing IκB to bind to NF-κB dimers and stay in the cytoplasm to inhibit transcription factor activity. In addition to bortezomib, carfilzomib and ixazomib are also approved as proteasome inhibitors for MM treatment by inhibiting NF-κB.296 Two glucocorticoids prednisone and dexamethasone are also approved for the clinical treatment of MM. The treatment mechanism is to interfere with the phosphorylation of RNA polymerase II required for NF-κB-dependent transcription initiation.418 Except for inhibiting critical components of the NF-κB pathway, blocking its downstream target genes or upstream stimuli is also a practicable therapeutic strategy. For example, denosumab, a monoclonal antibody that inhibits RANK ligand, and immunomodulatory drugs thalidomide, lenalidomide, and pomalidomide, which inhibit TNFα and IL-1β, are also approved for the treatment of MM.419, 420 Similarly, in some DLBCL subtypes that exhibit continuous NF-κB activation, BTK inhibitor has also been shown to have therapeutic value as a key molecule for BCR to activate the NF-κB pathway.421 Other anti-TNFα antibodies, including infliximab, adalimumab, and golimumab, have also been found to improve the therapeutic effect in breast cancer patients.422
Considering that these drugs do not directly target the core molecules of the NF-κB pathway, but their upstream and downstream molecules, it is difficult to clarify how much the inhibitor functions on NF-κB per se. Except for MM and some DLBCL subtypes, the strategy of directly inhibiting NF-κB seems unsuccessful in other cancers. The success of the drugs mentioned above in MM and DLBCL cannot be replicated in other tumor treatments, suggesting NF-κB has universal and complicated functions that could not be a fixed therapeutic target like PD-1/PD-L. Inhibition of NF-κB may enhance the cancer treatment response to most traditional treatments and treatments developed in recent years such as immune checkpoint inhibitors; however, long-term inhibition of the NF-κB pathway perhaps causes serious side effects, especially impaired immune response and compensated anti-tumor immune function.423 Given that NF-κB regulates many physiological functions, the balance between the anti-cancer effect and the side effects that impair normal physiological functions should be considered. Moreover, under drug-mediated pressure, NF-κB might cooperate with other signaling pathways to regulate pro-survival genes (such as cyclin D1 and Bcl-2) and upregulate the transcription of the genes, which helps tumor cells to develop drug resistance. Therefore, inhibiting NF-κB alone without affecting other signaling pathways seems to be an unachievable presence.
One alternative strategy is to combine NF-κB inhibitors with other treatments (such as chemotherapy and radiotherapy). For example, pentoxifylline (an REL inhibitor) combined with PD-1 immunotherapy enhances the therapeutic effect.424 The combined usage of multiple NF-κB inhibitors is also one of the feasible strategies. The study has reported using multiple NF-κB inhibitors in combination and found that it improves the clinical treatment effect in MM.425 At present, there are many studies on NF-κB inhibitors, which will not be summarized and discussed in this review, but most of the studies are conducted on in vitro cell models and animal models, and their value of human cancer treatment warrants further investigation. Recent clinical trials of cancer treatment targeting the NF-κB signaling pathway are summarized in Table 2.
| Cancer type | Target | Main drug | Phase | NCT number | Enrollment | Ref |
|---|---|---|---|---|---|---|
| MM | 20S PI | Ixazomib | III | NCT01564537 | 722 | 425 |
| KRAS G12D-mutant/p53-deficient NSCLC | 26S PI | Bortezomib | II | NCT01833143 | 16 | 448 |
| Classic Hodgkin lymphoma | 26S PI | Bortezomib | II | NCT00967369 | 20 | / |
| Head and neck cancer | 26S PI | Bortezomib | I | NCT00011778 | 25 | / |
| MM | SINE+26S PI | Selinexor + bortezomib + dexamethasone | II | NCT02343042 | 42 | 449 |
| Head and neck adenoid cystic carcinoma | 26S PI | Bortezomib | II | NCT00077428 | 25 | 450 |
| Advanced oesophagogastric adenocarcinoma | 26S PI | Bortezomib | I | / | 18 | 451 |
| Advanced gastric adenocarcinoma | 26S PI | Bortezomib | II | / | 16 | 452 |
| Endocrine-resistant metastatic breast cancer | 26S PI | Bortezomib | II | / | 9 | 453 |
| Locally recurrent or metastatic squamous cell carcinoma of the head and neck | 26S PI | Bortezomib | II | / | 61 | 454 |
| Malignant gliomas | 26S PI + DNA alkylating agents | Bortezomib + Temozolomide | II | / | 10 | 455 |
| Plasma cell myeloma | 20S PI | Ixazomib | II | NCT02765854 | 90 | / |
| Waldenström's macroglobulinemia | 20S PI | Ixazomib | II | NCT02400437 | 26 | 456 |
| Waldenström's macroglobulinemia | 20S PI+BTK | Carfilzomib + ibrutinib | III | NCT04263480 | 184 | / |
| Advanced solid tumors | Na-K ATPase | PBI-05204 | I | / | 46 | 457 |
| CLL | BTK | Ibrutinib | II | NCT01500733 | 86 | 458 |
| Early-stage chronic lymphocytic leukemia | NF-κB inhibitor | Omega-3 fatty acids | II | NCT00899353 | 16 | 459 |
| Advanced solid tumors and lymphomas | IKK inhibitor | Bardoxolone methyl | I | / | 44 | 460 |
| Primary CNS lymphoma | BTK | Ibrutinib | I | NCT02315326 | 13 | 461 |
| Waldenström's macroglobulinemia | BTK | BGB-3111 | III | NCT03053440 | 229 | / |
| NSCLC | RANKL | Denosumab | III | NCT02129699 | 509 | 462 |
| Giant cell tumor of bone | RANKL | Denosumab | III | NCT03259152 | 30 | / |
| Urothelial carcinoma | RANKL | Denosumab | II | NCT03520231 | 50 | / |
| Melanoma | RANKL | Denosumab | I | NCT03161756 | 72 | / |
| MM | BCL-2 | Venetoclax | I/II | NCT01794520 | 51 | 463 |
| MM | IL-1R | Anakinra | I | NCT02492750 | 14 | / |
| ALL | Phosphodiesterase | Pentoxifylline | III | NCT02451774 | 44 | / |
| Triple negative breast cancer | CD40 | CDX-1140 | I | NCT05029999 | 45 | / |
| Metastatic melanoma | CD40 | APX005M | I | NCT03597282 | 22 | / |
| NSCLC | CD40 | APX005M | I | NCT03123783 | 400 | / |
| Soft tissue sarcoma | CD40 | APX005M | II | NCT03719430 | 27 | |
| Metastatic pancreatic adenocarcinoma | CD40 | APX005M | I | NCT03214250 | 129 | 464 |
| Melanoma | CD40 | SEA-CD40 | II | NCT04993677 | 200 | / |
| NSCLC | CD40 | SEA-CD40 | I | NCT02376699 | 159 | / |
| Melanoma | CD40 | CP-870,893 | I | NCT01103635 | 25 | / |
| DLBCL | CD40 | SGN-40 | II | NCT00529503 | 151 | / |
| Non-Hodgkin lymphoma, DLBCL | BAFF-R | VAY736 | I | NCT04903197 | 86 | / |
- Abbreviations: ALL, acute lymphoblastic leukemia; BTK, Bruton's tyrosine kinase; CLL, chronic lymphocytic leukemia; diffuse large B-cell lymphoma. All NCT numbers were obtained from https://clinicaltrials.gov/; IKK, IkappaB kinases; MM, multiple myeloma; NSCLC, non-small cell lung cancer; PI, proteasome inhibitor; RANKL, receptor activator of NF-κB ligand; SINE, selective inhibitor of nuclear export.
5 CONCLUSION
Since NF-κB was discovered in 1984, extraordinary efforts have been being made to understand the functions and regulating mechanisms of NF-κB for 35 years, leading to significant progress. There has been convincing evidence to support the connection between NF-κB, cancer, and inflammation, and it has been accepted that the NF-κB pathway plays a key role in immune homeostasis, chronic inflammation, tumorigenesis, and development. Based on the numerous upstream stimuli and downstream target genes of NF-κB currently known, we conclude that NF-κB has a wide range of functions, like a hub with a huge communication network. Nevertheless, there are still many unknowns about the comprehensive mechanisms and functions of NF-κB that we need to further explore. Recently, more and more drugs targeting NF-κB have been developed and examined. It should be noted that considering the diversity of upstream stimulus and downstream target genes of NF-κB, to complete inhibition of NF-κB as a therapeutic method might not be a practicable strategy. Future investigation on NF-κB as an anti-cancer target should focus on inhibiting its tumor-promoting effects caused by pathological NF-κB activation while avoiding affecting their normal physiological functions; meanwhile, the combination of multiple drugs targeting different key regulators of the NF-κB pathway, even multiple pathways, is also attractive.
ACKNOWLEDGMENTS
We wish to thank the timely help given by Dr. Yang Wang and Ms. Yueyi Li for composing the figures. All figures are created with BioRender.com.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
The authors declare that ethics approval was not needed for this study.
AUTHOR CONTRIBUTIONS
T.Z., H.Z., and H.H. conceived, wrote, and edited the manuscript; C.M. and Z.Z. provided significant assistance.
Open Research
DATA AVAILABILITY STATEMENT
Not applicable.




