Nanotechnology connecting copper metabolism and tumor therapy
Abstract
Copper (Cu) is an essential trace element in the human body that is involved in the formation of several natural enzymes, such as superoxide dismutase and cyclooxygenase. Due to the high density of the outer electron cloud of Cu, which allows the transfer of multiple electrons, Cu is often used as the catalytic center in various metabolic enzymes. However, both deficiency and excessive accumulation of Cu can result in irreversible damage to cells. Therefore, strategies to regulate Cu metabolism, such as Cu exhaustion and Cu supplementation, have emerged as attractive approaches in anticancer therapy, due to the potential damages caused by Cu metabolism disorders. Notably, recent advancements in nanotechnology have enabled the development of nanomaterials that can regulate Cu metabolism, making this therapy applicable in vivo. In this review, we provide a systematic discussion of the physical and chemical properties of Cu and summarize the applications of nanotechnology in Cu metabolism-based antitumor therapy. Finally, we outline the future directions and challenges of nano-Cu therapy, emphasizing the scientific problems and technical bottlenecks that need to be addressed for successful clinical translation.
1 INTRODUCTION
Copper (element symbol: Cu) is a chemical element located in the IB group with atomic number 29. It is one of the earliest transition metals discovered by human beings. As the best pure metal, Cu is extremely hard, wear-resistant, with good ductility, thermal conductivity, and electrical conductivity. Cu is a crucial micronutrient for human health since it plays an important role in the growth and maintenance of central nervous system, blood, brain, liver, skin, hair, bone tissues, as well as other internal organs.1-3 The amount of Cu is approximately 100–150 mg in the human body. It participates in the assembly of various enzymes, such as superoxide dismutase 1 (SOD1) and cyclooxygenase (COX).4, 5 However, recent research suggests that copper ions also mediate to the growth and spread of cancer cells. The density of the outer electron cloud of Cu is high, which can accommodate the transfer of multiple electrons.6 Therefore, Cu is the catalytic center of a variety of metabolic enzymes, including monoamine oxidase, superoxide dismutase, and ceruloplasmin.7-16 Cu has a significant role in electron transfer, protein synthesis, purine metabolism, lipid and neuron development, as well as the activation of hemoglobin synthesis and the promotion of iron uptake and use.17-33
According to several studies, different malignant tumors have higher Cu contents than normal tissues.34 Cu can stimulate angiogenesis,35 which is necessary for the growth and metastasis of tumors, by activating angiogenic proteins like angiopoietin (Ang), vascular endothelial growth factor (VEGF),36-39 fibroblast growth factor 1 (FGF1),40 and interleukin-1 (IL-1), and promote angiogenesis.41-44 Therefore, Cu- exhaustion-related cancer therapy emerges at the historic moment. However, with the deepening of research, researchers have shown that Cu buildup can potentially result in cell death or irreversible harm to cells, such as cuproptosis,45-47 apoptosis,48, 49 pyroptosis,50, 51 and ferroptosis.52, 53 In addition, the transformation of Cu2+ and Cu+ sensitizes Fenton-like reaction and consumes glutathione (GSH), promoting intracellular oxidative stress.54-63 All of these suggest that Cu ion interference therapy containing Cu exhaustion as well as Cu supplementation has become an attractive therapeutic strategy in anticancer therapy.64-66 It is true that life is Cu and death is Cu. Cu therapy gradually becomes a research hotspot and has potential prospect.67, 68
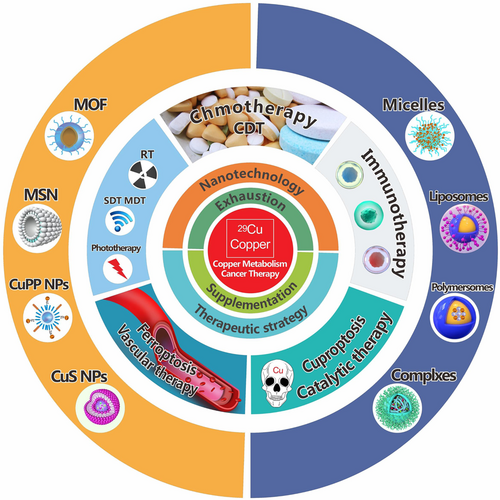
In the past decades, Cu has been used clinically to treat diseases such as metal toxicity and Wilson Disease (WD).69-74 Cu is also only used as computed tomography (CT) imaging and magnetic resonance imaging (MRI) contrast agent.75-78 Until the 21st century, they are used as antitumor drugs in clinical trials,79 such as tetrathiomolybdate (TTM) and methionine derivative copper complexes (Cu(CMQA)(H2O)). However, these molecules have strong cytotoxicity in tumor cells and normal cells, resulting in inevitable side effects in antitumor therapy. The development of nanotechnology connects Cu metabolism and tumor therapy in vivo, such as micelles, polymersomes, metal organic framework (MOF) and so on (Figure 1).80-83 In this review, we will systematically discuss the physical and chemical properties of Cu, summarize the application of nanotechnology connecting Cu metabolism-based antitumor therapy, expound the new visions and challenges of nano-Cu therapy, and emphasize the pivotal scientific issues and technical application bottlenecks, hoping to provide a general guidance for its clinical translation.
2 Cu METABOLISM IN HUMAN BODY
2.1 Absorption and transport of Cu in vivo
The source of Cu for the human body is mainly daily food and water. Radioisotope studies have shown that Cu begins to be absorbed in the stomach after entering the digestive tract, but the mainly in the duodenum and the front of the small intestine. Some Cu can also be absorbed in the distal part of the small intestine. Elemental Cu cannot be absorbed because it is insoluble in water. Most Cu in food is absorbed as soluble chelates rather than ions. The mechanisms of Cu absorption are saturated active transport and unsaturated diffusion. The transport of copper in the human body is influenced by the amount of copper present in the diet. When the dietary copper content is low, copper is primarily transported through the saturated active pathway. Conversely, when the dietary copper content is high, diffusion plays a dominant role in copper transport. Copper in the diet is transported to the intestinal mucosa with the help of various complexing agents, such as amino acids. Among the amino acids that bind to copper, L-histidine is the most predominant, followed by threonine, glutamic acid, cystine, and cysteine.84 After being absorbed, copper is first transported into intestinal mucosal cells in the form of metallothionein bound to macromolecular proteins. It then enters the bloodstream through the basolateral membrane of intestinal mucosal cells, where it undergoes phosphorylated adenosine triphosphatase (p-ATPase)-mediated copper transport.
2.2 Intracellular Cu uptake
After entering the blood, most Cu binds with albumin, while a few combine with small molecular components such as amino acids to form loose compounds, which can benefit its further absorption and utilization in other tissues.85, 86 The main modes of cellular uptake of Cu are mainly ceruloplasmin transmitter and free cupric pathway. Plasma ceruloplasmin complexes contain approximately 75%–95% of the Cu present in the plasma. Each molecule of ceruloplasmin binds 6–7 copper ions at different sites, enabling it to transfer copper to cells and intracellular proteins via receptors.87, 88 Studies have shown that leukocytes have the highest number of receptors for Cu. Once plasma ceruloplasmin binds to the receptor on the cell membrane, the copper ions are reduced from Cu2+ to Cu+ and separated from ceruloplasmin. This process allows the copper ions to enter the cell and be utilized for various intracellular functions. The other is the free cupric pathway, in which Cu first enters the histidine-rich (N)-terminal Cu binding site in plasma albumin, combines with the free histidine, and transports to the metal ionophores in cell membranes of liver cells and fibroblasts.89, 90 The Cu-binding ionophores then transfer the Cu to intracellular Cu-binding protein. Cu from the free cupric pathway is also reduced to Cu+ before entering the cell.
2.3 Extracellular Cu efflux
The efflux of Cu is accomplished by a protein called P type of ATPase (P2-ATPase), which is a transmembrane single-chain polypeptide. The N-terminal metal binding site of the protein is composed of Cu binding sites, halogen transport sites, and phosphorylation sites. In the role of ATPase, an aspartate amino acid residue in the phosphorylated region of P2-ATPase is phosphorylated, which changes the conformation of the protein, and transfers Cu to the center of the enzyme. Then dephosphorylation of P2-ATPase results in the efflux of Cu to extracellular.91, 92
3 Cu EXHAUSTION THERAPEUTIC STRATEGY
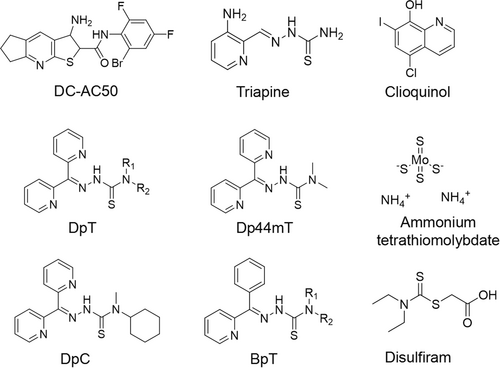
It was found that reducing the copper content of tumor would have a significant inhibitory effect on tumor. Due to the importance of copper on tumor, especially on tumor neovascularization, the development of copper ligand drugs with high anticancer ability has attracted clinical attention. The exhaustion of Cu mainly includes Cu chelation (penicillamine [B-dimethylcysteine], Dp44mT, thiosemicarbazones, triethylene tetramine dihydrochloride [trientine], tetraethylenepentamine [TEPA], tetrathiomolybdate, disulfiram, clioquinol, A TN-224, CDM and other newer chelators) and Cu transport inhibition (DC-AC50, siSLC31A1, and other inhibitors) (Figure 2). It should be noted that chelators used for copper ion interference therapy are not specific to copper ions, as they can also chelate other metal ions, such as calcium, zinc, and others. These chelators have also been used for interference therapy with other metal ions.
While copper ions are an essential physiological element, the systemic administration of copper ligand drugs without selective targeting can lead to unintended side effects, such as erythema, optic neuritis, vomiting, and leukopenia. To address this issue, the development of an intelligent drug delivery system capable of specifically targeting the delivery of copper ligand drugs to the tumor site is necessary. By specifically chelating copper ions at the tumor site, the trend of tumor neovascularization can be reduced, which can lead to a slowing down of tumor evolution or synergistic therapy with other drugs. The combination of cytotoxic drugs and anti-neovascular drugs is a common strategy for clinical chemotherapy of tumor patients, such as bevacizumab/5-fluorouracil combination for colon cancer and trastuzumab/paclitaxel combination for breast cancer. Cytotoxic drugs directly kill tumor cells, while anti-neovascularization drugs reduce neovascularization to achieve synergistic antitumor effect. However, the novel strategy of codelivering cytotoxic drugs and copper chelators to achieve tumor combination therapy is still full of challenges.
Therefore, Jiang et al. constructed a tumor targeting micellar system based on amphitropic polypeptides, which could cocarry doxorubicin (DOX), a first-line drug for triple-negative breast cancer (TNBC), and a chelating agent X that can specifically recognize copper ion, and target to TNBC tumor neovascularization through cRGD-mediated targeting (Figure 3A). Once the chelating agent X was successfully loaded with copper ions, it could also emit near-infrared fluorescence to achieve the purpose of integrated diagnosis and treatment. After treatment, it was found that the content of Cu ion in tumor was significantly reduced, and the content of neovascularization was reduced. Combined with DOX, a good combination therapy effect was achieved, and systemic toxicity was reduced. The combination of cupric chelating agent and chemotherapeutic drug in this study is expected to be a new strategy for tumor treatment.93 In another research, a mitochondria-targeted, Cu-exhausted nanoparticle (CDN) was created by Rao et al. to combat TNBC.94 They found that CDN targeted in mitochondria and locally exhausted Cu, resulting in mitochondrial oxidative phosphorylation (OXPHOS) activity inhibited and metabolism switched to glycolysis with ATP decreased. Simultaneously, decreased mitochondrial membrane potential and increased oxidative stress were observed in TNBC cells not healthy cells (Figure 3B). The significant antitumor effect and survival rate in three murine TNBC models suggested the potential clinical application prospect of this method. However, the applications of Cu chelating agents in clinical practice can lead to low Cu concentration, which disrupts other normal physiological processes requiring Cu and finally causes severe side effects. Additionally, the potential side effects and toxicity may also be caused by the nonspecific binding of Cu-chelators with other metal cations. Further research is still needed to focus on the specific control of Cu concentration in the lesions.
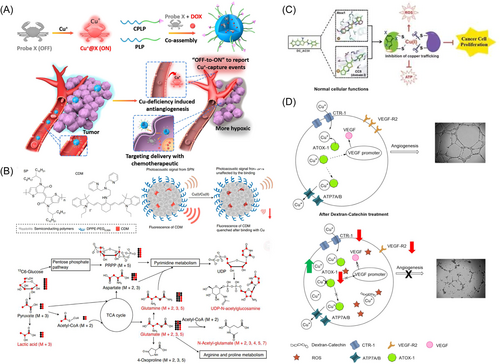
Transport is another important procedure for the Cu concentration. Jiang et al. found the small molecule inhibitor of copper chaperone for the first time by using theoretical simulation, chemical biology, and pharmacological experimental verification strategies. DC-AC50 blocked the intracellular transport of copper ions by combining the copper transport interface of antioxidant 1 copper chaperone (Atox1) and copper chaperone for superoxide (CCS), and specifically inhibited the proliferation of tumor cells without affecting the survival of normal somatic cells (Figure 3C). Studies on the mechanism of action showed that the compound inhibited the activity of Cu/Zn superoxide dismutase SOD1 with copper ion as a cofactor, increased the level of ROS in tumor cells, affected mitochondrial function and reduced the production of ATP, blocking the proliferation of tumor cells in both ways. The challenge of designing inhibitors related to copper regulatory processes is that they do not affect copper function in normal cells. DC-AC50 did not directly interact with copper while blocking the function of copper metal-chaperone. As the first member of this new class of inhibitors, the discovery of DC-AC50 provided a new way to intervene and overcome copper transport disorders. This study not only provided an efficient and low-toxicity lead compound for the targeted therapy of tumor, opening up a new field for antitumor research, but also lay a solid foundation for the study of the chemical regulatory mechanism of copper ion in vivo. Not alone, but with a good prototype, Orazio et al. showed that exhausted the copper importer copper transporter-1 (CTR-1) and copper trafficking Atox1 via Dextran-Catechin nanoparticles exhibited prominent antiangiogenic activity and antitumor activity in vitro and in vivo (Figure 3D).95 Compared with metal chelating agents, targeted Cu chaperones regulate the concentration and distribution of intracellular Cu more specifically and precisely, so as to achieve therapeutic effects while reducing toxic side effects. This study provides an efficient and low-toxicity compound for targeted antitumor therapy, opening a new field for antitumor research and laying a solid foundation for the study of the chemical regulatory mechanism of Cu in vivo.
4 Cu SUPPLEMENTATION THERAPEUTIC STRATEGY
As we all know, Cu-based nanomaterials were frequently used as drug delivery carriers at the beginning. In this section, we focus on the functional Cu nanoparticles, in which Cu can also play a therapeutic role (Table 1). Such as (1) Cu and chemotherapy; (2) Cu and radiotherapy; (3) Cu and phototherapy; (4) Cu and chemodynamic therapy (CDT); (5) Cu and sonodynamic therapy (SDT); (6) Cu and microwave dynamic therapy (MDT); (7) Cu and catalytic therapy; (8) Cu and ferroptosis; (9) Cu and vascular therapy; (10) cuproptosis; (11) Cu and immunotherapy. The intrinsic mechanism of Cu based on chemotherapy such as CDT, SDT, MDT, catalytic therapy, is based on electron transfer in the outer orbital of copper, which forms a catalytic center. These centers primarily consist of Cu1+ and Cu0. Conversely, phototherapy, cuproptosis, and immunotherapy mainly rely on the physical properties of copper itself and its accumulation, enabling the utilization of copper ions in various oxidation states, including Cu1+, Cu2+, and Cu0 for these therapies.
| Cu-based NMs | Cu type | Role | Functionalities | References |
|---|---|---|---|---|
| GOx@[Cu(tz)] | Cu(NO3)2·3H2O | Therapeutic agent | Increase the level of Cu, Induce cuproptosis | [65] |
| DOX-ProbeX | ProbeX | Chelator/tracer | Antineoangiogenesis, removal Cu+ | [93] |
| CDN | CDM | Therapeutic agent | Mitochondria-targeted, Cu-exhausted | [94] |
| PEG/Cu-HMSNs | Cu[NO3]2·3H2O | Therapeutic agent | Released Cu2+, Fenton-like reactions, reactive oxygen species (ROS) generated | [96] |
| G5. NHAc-Pyr/Cu(II) | CuCl2 | Therapeutic agent | MRI, chemotherapy | [97] |
| CSA | Cu2−xSe | Therapeutic agent | Photothermal therapy (PTT), radiotherapy, multimodal imaging | [98] |
| 64Cu- W-GA-PEG CPN | 64Cu | Therapeutic agent | Radiotherapy, positron emission tomography (PET) imaging, rapid renal clearance | [99] |
| CuS-BSA NPs | CuS | Carrier agent | Drug delivery, photothermal agents | [100] |
| CuS NCs | CuS | Therapeutic agent | Generate high levels of ROS, photodynamic therapy (PDT) | [101] |
| CuTz-1-O2@F127 | CuI | Therapeutic agent | Overcoming intracellular hypoxia, reducing glutathione (GSH) levels in the tumor | [102] |
| d-Cu-LDH/ICG NPs | Cu(OH)2 | Therapeutic agent | Improve PTT efficiency, singlet oxygen (1O2) generation | [103] |
| Cu-Cys NPs | CuCl2 | Therapeutic agent | Induce GSH depletion, tumor-cellapoptosis | [104] |
| MSN | Cu(NO3)2·3H2O | Therapeutic agent | Augmenting the intracellular levels of cytotoxic ROS | [105] |
| HA@Cy-Cu NPs | CuCl2 | Therapeutic agent | Enhanced photostability, transform H2O2 to •OH | [106] |
| Cu@PAA NCs | Cu(NO3)2·3H2O | Therapeutic agent | Achieve high spatiotemporal catalytic efficacy, photoacoustic imaging | [107] |
| Cu(II)NS | CuCl2 | Sonosensitizer | Enhance tumor accumulation, increase the effect of SDT | [108] |
| RBC-Zr@APC/C NPs | CuO | Therapeutic agent | Raise the generation of ROS, improve the efficacy of MDT | [109] |
| CuCy-pHLIP | CuCy | Therapeutic agent/sensitizer | Produce ROS, induce PDT | [110] |
| Cu SAZs | CuO | Therapeutic agent | Achieve self-enhanced NCT | [111] |
| Cu-HNCS | Cu(OAc)2·H2O | Catalyst | Enhance tumor growth inhibitory effect | [112] |
| CPNs | CuO | Therapeutic agent | Aggravate the oxidative damage and lipid peroxidation buildup in cells | [113] |
| GCT@CM NPs | CuCl2·2H2O | Therapeutic agent | Cause tumor cell apoptosis and immunogenic cell death (ICD) | [116] |
| CuS-RNP@PEI NPs | CuS | Therapeutic agent | Antitumor efficacy, induce ICD | [117] |
| Cu-DON | CuCl2 | Carrier/therapeutic agent | Amplify oxidative stress, induce ICD | [118] |
| CuPP | CuP | Therapeutic agent | Overcome tumor hypoxia, tumor immunotherapy | [119] |
| CuS NPs | CuS | Therapeutic agent | Elevated ROS level, overcome gefitinib resistance | [120] |
4.1 Chemotherapy based on Cu nanoparticles
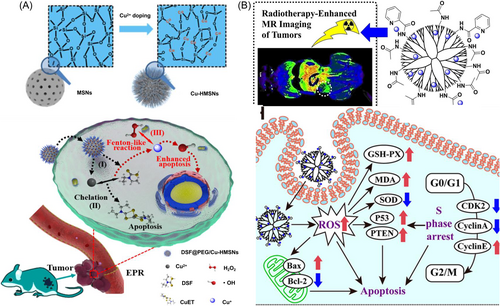
The latest research found that the traditional abstinence drug disulfiram (DSF), which was metabolized to dithiocarbamate (DTC) by the stomach and blood in the human body, exhibited a certain antitumor effect. DTC could form a complex with Cu in the form of DTC-Cu2+ chelation (CuET) in vivo. CuET interferes with ubiquitination protein degradation system, which makes tumor cells unable to timely clean up “garbage” proteins, resulting in metabolic disorders of tumor cells, and eventually death. Herein, Shi et al. reported a tumor microenvironment (TME) responsive PEGylated Cu2+ doped with hollow mesoporous silica nanoparticles loaded with DSF (PEG/Cu-HMSNs).96 Once internalized into tumor cells, the weak acid environment can lead to its rapid biodegradation and accelerated DSF release. Then the toxic CuETs and Fenton-like reaction synergistically enhanced DSF-based chemotherapy (Figure 4A). In another work, Shi et al. reported a pyridine (Pyr)-functionalized generation 5 (G5) poly(amidoamine) (PAMAM) dendrimers complexed with Cu(II) for MRI-guided radio-chemotherapy (Figure 4B).97 Results demonstrated that the G5.NHAc-Pyr/Cu(II) complexes effectively inhibited the proliferation of different tumor cells, promoted the production of intracellular reactive oxygen species (ROS), blocked the cell cycle, and ultimately led to apoptosis. In this study, dendritic polymer monodisperse nanostructure and modified surface were utilized to construct dendritic macromolecule Cu complex as an integrated diagnosis and treatment nanoplatform for tumor MRI and chemotherapy. The research thus provides a new design for the construction of novel diagnostic and treatment integrated nanomaterials. At the same time, enhanced diagnosis and treatment effect is achieved through combined radiotherapy or ultrasound technology, providing theoretical guidance and direction Cu-assisted combination therapy without systemic toxicity.
4.2 Cu and radiotherapy (RT)
Cu has 29 isotopes, including 64Cu,67Cu,62Cu,61Cu, and 60Cu. Cu isotopes can easily accumulate in cancer cells and release β-rays and γ-rays for cancer diagnosis and treatment. Moreover, the long half-life of Cu isotopes allows their clinical application. However, the small difference between the sensitivity of tumor tissue and normal tissue to radiation limits the antitumor effect of RT. To maximize the radiosensitivity, high atomic number nanomaterials like gold, bismuth, tungsten, and platinum are frequently employed in RT. Through the enhanced permeability and retention (EPR) effect, they can be augmented at the tumor sites and become diagnostic and therapeutic probes integrating multimodal imaging (CTI, PAI, and MRI) and multimodal therapy (PTT and RT). Recently, Li et al. reported that the PEGylated Cu2−xSe nanoparticles can be used as a highly effective radiosensitizer.98 They also found that W-GA-PEG CPN can greatly improve the effect of RT.99 These studies propose the application of Cu in tumor RT, which is expected to be further developed in clinical practice. However, the optimal Cu isotopes in RT is needed.
On the contrary, the disturbances of copper metabolism can also lead to radiotherapy resistance. For example, liver cancer cells are often accompanied by the loss of endogenous copper metabolisation-related protein COMMD10, which intensifies the accumulation of Cu in cells, thus further aggravating the radiotherapy resistance of liver cancer. Copper chelating agent can reverse the above effect of radiotherapy resistance. It was found that the accumulation of Cu caused by COMMD10 low expression could inhibit the ubiquitination degradation of hypoxia inducible factor-1α (HIF-1α), promote the nuclear translocation of HIF-1α and increase the transcription and translation of ceruloplasmin, thus forming a positive feedback regulatory loop of HIF-1α/Ceruloplasmin and inhibiting the cell ferroptosis, resulting in the radiotherapy resistance.
4.3 Phototherapy based on Cu nanoparticles
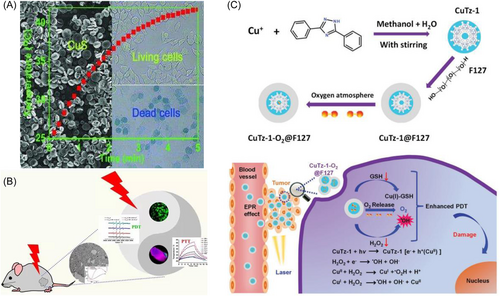
With d-d electron transition, copper sulfide (CuS) nanoparticles show significant near-infrared absorption regardless of size or form, with good photothermal properties. Additionally, the simple preparation of CuS nanoparticles and adjustable size promise their application in photothermal therapy (PTT). Li et al. first modified CuS with mercaptoacetic acid for PTT. To enhance the photothermal conversion efficiency of CuS, Tian et al. prepared a flower-like CuS with a superlattice structure.100 However, due to the large size, its application in vivo was limited (Figure 5A). Dai et al. prepared a disk mounted Cu9S5 for PTT. Surprisingly, Liu et al. found that the better significant killing efficiency of CuS than that of precious metal nanomaterials, such as gold nanoparticles. Due to its low cost and high photothermal conversion efficiency, CuS nanoparticles had attracted extensive attention in the field of PTT. Besides PTT, the researchers observed that these CuS nanoparticles also had intrinsic near-infrared photodynamic properties, which produced high concentrations of ROS to kill tumor cells in one collaborative study. They found that under near-infrared light irradiation, Cu+ released from the CuS nanocrystals interacted with the surrounding biological environment to generate redox reactions, resulting in electron transfer, which reflected the characteristics of photodynamic therapy (PDT) (Figure 5B).101 Moreover, Lin et al. found that Cu+ directly activated hydroxyl radical (•OH), through the hydrogen or electron transfer process, realizing PDT (Figure 5C).102 All the results revealed the dual antitumor mechanism of Cu-based nanoparticles-PDT and PTT.
4.4 CDT based on Cu nanoparticles
The important progress of CDT is Fenton or Fenton-like reactions to produce highly cytotoxic hydroxyl radicals. Some Fenton catalysts have been used in tumor CDT, mainly by converting the endogenous hydrogen peroxide of cancer cells into free radicals. Cu+-based Fenton-like reactions can occur effectively even under weak acidic and neutral conditions, reaching 160 times fold in comparison to Fe2+-based Fenton reactions. But because of the low redox potential of Cu2+/Cu+ (~0.16 V), Cu+ is very easy to be oxidized to Cu2+, which makes the Fenton-like reaction difficult to occur in vivo. Therefore, using specific molecules in the TME to control the production of Cu+ in tumor tissue for the Fenton-like reaction can be ingenious and crucial. For example, Xu et al. developed multifunctional copper doped hydrotalcite nanoparticles with artificial surface defects (d-Cu LDH) to improve its photothermal conversion efficiency (PTT) and singlet oxygen (1O2) generation (PDT). At the same time, hyperthermia led to the dissolution and release of Cu+ (CDT).103 Similarly, GSH can also convert Cu2+ to Cu+ for further CDT. Li et al. designed a self-assembled copper-amino acid nanoparticle (Cu-Cys NP) for in situ GSH “AND” H2O2 sequentially triggered CDT.104 Chen et al. demonstrated Janus-type nanoarchitectures, Cu-Fe-MSNs for CDT.105 Moreover, Peng et al. constructed an organic nanotherapeutic agent based on cyanine and Cu2+ for combined PTT and CDT.106 However, the endogenous hydrogen peroxide of tumor cells is not sufficient to achieve satisfactory chemokinetic effect. Therefore, it is necessary to develop chemical kinetic reagents that can increase the function of intracellular hydrogen peroxide. Metal peroxide, which is composed of peroxy group and metal ion, is an excellent hydrogen peroxide supply material. Since iron, copper, manganese, cobalt, and other metal ions have been proved to have good Fenton catalytic activity, Fenton metal peroxide will be a potential selffeeding chemical dynamic anticancer agent of hydrogen peroxide. Chen et al. successfully synthesized copper peroxide nanoparticles and realized selfsustaining chemokinetic treatment of hydrogen peroxide. The team prepared copper peroxide nanoparticles using the complexation of copper ions and hydrogen peroxide assisted by hydroxide ions, which could be reversed under acidic conditions. Therefore, copper peroxide nanoparticles had the characteristics of acid response, and decomposed and released hydrogen peroxide and copper ions with Fenton-like catalytic activity under weak acidic conditions. The accompanying Fenton-like reaction effectively generated hydroxyl free radicals, so as to kill cells efficiently. Both cell and animal experiments showed that copper peroxide nanoparticles had good chemical kinetic effect on tumor. As hydrogen peroxide self-contained enhanced chemical kinetic intelligent anticancer drugs, copper peroxide nanoparticles had a good application prospect in cancer therapy.
4.5 SDT based on Cu nanoparticles
SDT can achieve inexpensive, safe and effective tumor therapy by utilizing the sonosensitive agents at tumor sites and the strong tissue penetration capacity of ultrasound. US radiation causes the transition from Cu2+ to Cu+, accelerating the formation of ·OH from H2O2 for SDT. As electron-hole pairs separate due to the transition, ROS creation for SDT is encouraged.107 The Cu2+ contains 27 electrons. After TCPP chelates the Cu2+, an unpaired electron will appear in the middle of the overall molecular orbital. This state is also called open shell with the ground state of Cu(II)NS being a double state D0. After this nanoparticle entered tumor cells, the hyperexpressed GSH will reduce Cu(II)NS to univalent Cu(I)NS, and GSH will give an electron to pair with the unpaired electron.108 The ground state of the Cu(I)NS is restored to the singlet state S0 for SDT.
However, the antitumor activity of SDT is usually based on the oxygen, which limits its application in solid tumors with hypoxic TME, such as pancreatic cancer. To overcome this limitation, more and more studies had been conducted to explore a variety of new sound-sensitive systems. At the same time, PTT, chemotherapy, PDT, CDT and immunotherapy also showed effective synergistic effect. Huang et al. developed a kind of Cu-metal-organic framework (Cu-MOF) nanoparticles loaded with acoustic free radical initiators for hypoxic-adaptive chemosonodynamic therapy of pancreatic cancer in situ. In anoxic TME of in situ pancreatic cancer, structural degradation of Cu-MOF results in the release of Cu2+ and AIPH, and further dissociation of Cu-MOF and decomposition of AIPH to produce cytotoxic alkyl radicals (R·) and N2 bubbles after US irradiation at the tumor site, which does not require oxygen supply. In turn, Cu2+ consumed high levels of GSH in tumor cells and was reduced to Cu+, which catalyzed Fenton-like reactions to produce additional ROS. On the other hand, N2 bubbles enhanced the deep penetration of nanoparticles through ultrasonic cavitation effect under the action of ultrasound. Therefore, this acoustic-chemokinetic synergy of hypoxic TME response provided an ideal means to achieve nonoxygen-dependent free radical generation and enhancement of the antitumor effect of SDT.
4.6 MDT based on Cu nanoparticles
Under microwave (MW) irradiation, Cu-based nanoparticles can also enhance the production of ROS. Meng at al. constructed a biomimetic multifunctional red blood cell membrane (RBC) coated nanoparticle (RBC-Zr@APC/C NPs).109 Through the targeting effect caused by biomimetic alteration, the nanoparticles aggregated at the tumor site after i.v. administration and continued to convert O2 to ROS for MDT. Copper-cysteamine was discovered by Chen et al. to be a new group of sensitizers that could produce ROS when activated by light, X-rays, microwaves, or ultrasound.110
4.7 Catalytic therapy based on Cu nanoparticles
Nanocatalysis medicine is a cutting-edge academic idea proposed by a scientific research team led by Shi et al. It aims to use nontoxic/low-toxic nanomaterials to initiate in situ catalytic reactions in tumor by responding to specific internal field microenvironment or exogenous laser and ultrasonic fields of action at tumor sites. It can effectively realize oxidative damage and cell death of tumor cells. This catalytic tumor treatment method does not use highly toxic chemotherapy drugs, has the characteristics of high efficiency, strong specificity, high safety, has been widely recognized by the peer, and has been rapidly developed in recent years. The redox reaction between Cu2+ and GSH can not only remove GSH and improve the oxidative stress of tumor cells, but also the reduction product Cu+ can transform H2O2 into more toxic •OH through Fenton-like reaction, enhancing the efficacy of catalytic therapy.
In addition to Cu2+/Cu+, Cu atom also plays a vital role in tumor therapy, such as the Cu single-atom nanozyme, a peroxidase (POD) that catalysis H2O2 to •OH. Cu single-atom nanozyme has a unique metal active center and good microenvironment regulation ability, which can overcome the shortcomings of conventional nanozyme like element heterogeneity and low density of active sites. Wang et al. designed a biomimetic copper single-atom nanozyme system for self-enhanced nanocatalytic tumor therapy.111 Likelywise, Shi at al. reported a bioinspired hollow N-doped carbon sphere doped with a single-atom copper species (Cu-HNCS) for effective antitumor therapy.112
No matter it is CDT, SDT, MDT, or catalytic therapy, all the therapies are relied on the electron rearrangement on the hybridized orbital of Cu to generate energy conversion, trigger reactions in tumor cells, transform nontoxic or low-toxic chemodrugs into more toxic chemodrugs, and effectively realize oxidative damage and cell death. These methods have the characteristics of high efficiency, strong specificity, high safety, and have been widely recognized by the scientists. They are helpful to solve some bottlenecks of chemotherapy, phototherapy, acoustic therapy, and other applications in clinical.
4.8 Cu and ferroptosis
Cu-based nanoparticles can catalyze not only Fenton-like reaction, but also artemisinin (ART) to produce ROS, which further aggravates the oxidative damage and lipid peroxidation buildup in cells, and thus kill cancer cells. Moreover, ART can also be used as a powerful autophagy inducer to increase the iron level in cells by degrading ferritin, promoting ferroptosis, and producing significant antitumor effects.113 The study demonstrates the interaction between metal ions in cells, expanding the application of ferroptosis in cancer treatment.
In addition to copper-mediated catalytic reactions, copper ions are also directly involved in the regulation of ferroptosis. The chelating agents TM and TEPA of copper ions can inhibit ferroptosis, while the addition of additional copper ions can promote ferroptosis, suggesting that copper ions may have the function of promoting ferroptosis. Moreover, copper ions did not affect the intracellular level of iron ions during the process of promoting ferroptosis, suggesting that copper ions may be a new type of Fe-promoting death metal ions besides iron ions. The results showed that the chelating agent reversed erastin induced glutathione peroxidase 4 (GPX4) protein decline, while copper ions promoted GPX4 protein decline. At the same time, copper ion did not affect GPX4 gene expression during ferroptosis. In addition, erastin combined with copper ions increased ubiquitination of GPX4 protein, and the autophagy inhibitor chloroquine (CQ) prevented GPX4 protein degradation. Therefore, the copper ion might promote GPX4 protein degradation via autophagy. Researchers found that the combination of copper ions and erastin significantly activated autophagy dependent ferroptosis, while knockdown of autophagy related gene autophagy protein 5 (ATG5) significantly inhibited the combination of copper ions and erastin induced ferroptosis. Then they found that erastin and copper ions selectively increased GPX4 binding to the autophagy receptor tax1 binding protein 1 (TAX1BP1). At the same time, TAX1BP1 knockdown did indeed inhibit GPX4 protein degradation and reduce cell sensitivity to ferroptosis, suggesting that TAX1BP1 was a key autophagy receptor in GPX4 protein degradation. This was the first ruled out erastin-induced GPX4 aggregation due to copper ion mediated ROS production. Based on a fluorescence conformational change on recombinant GPX4 protein, researchers found a significant spectral shift under copper ion treatment, indicating a direct interaction between copper and GPX4. Finally, they found that copper ions selectively bind to GPX4 cysteine residues C107 and C148. Similar results were obtained in vivo studies that copper promoted ferroptosis.
4.9 Vascular therapy based on Cu nanoparticles
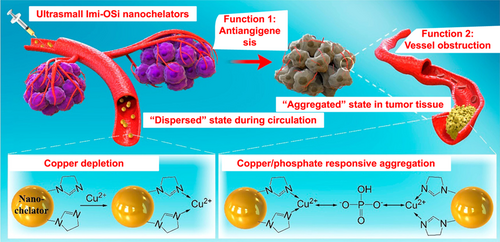
Despite widespread clinical success, traditional cancer cell focused therapies have shortcomings that allow patients to develop drug resistance and suffer serious side effects. Tumor vascular targeting therapy is a promising approach to halt tumor progression by interfering with the vascular system instead of cutting off the supply of nutrients. This strategy has gained significant attention in recent years. Currently, there are two main strategies for tumor vascular targeting therapy. The first strategy involves blocking angiogenic pathways, such as VEGF and the copper signaling pathway, to prevent the formation of neovascularization. The second strategy involves obstructing or destroying established tumor vasculature. For instance, DNA nanorobots can be constructed to mediate the thrombin delivery system, which induces tumor blood vessel thrombosis and obstruction. Recently, Yu et al. reported a nanochelating agent (Imi-OSi, <6 nm) that effectively inhibited tumor by chelating with Cu,114 suppressing tumor angiogenesis. Moreover, under the stimulation of the TME, the Imi-OSi can change from dispersion to aggregation, forming secondary particles and blocking blood vessel functions (Figure 6). The rational design of functional nanomaterials provides a conceptual framework for vascular-targeted therapy. Furthermore, in the current era of rapidly advancing tumor therapies, combining immunotherapy with chemotherapy has led to unexpected tumor suppression. Antiangiogenic therapy has also shown benefits at a higher level. Multiple studies have demonstrated the synergistic effect of combining immunization with Cu-antiangiogenic therapy.
4.10 Cuproptosis
The cell death is a normal life phenomenon, and its related research has been a point in the field of life science. According to the different mechanism, the cell death mode is also different, such as apoptosis, pyroptosis, necrosis, ferroptosis and so on. Among them, ferroptosis, an emerging cell death named in 2012, has become the focus of research in recent years. Similar to iron, intracellular copper ions exhibit cytotoxicity when concentrations exceed the threshold for maintaining homeostasis mechanisms. The researchers first performed experiments on different cell lines using copper ionophores with structures, demonstrating that copper ionophores could induce cell death, which was mainly dependent on the accumulation of copper ions in cells. To confirm the mechanism of this mode of cell death, they performed knockout of key apoptosis factors Bcl2 associated protein X (BAX) and Bcl2 antagonist/killer 1 (BAK1), and used caspase inhibitors for apoptosis, ferrostatin 1 for ferroptosis, necrostatin 1 for necrotic apoptosis and N-pancreatic cysteine for oxidative stress. It was found that the cell death induced by copper ionophores could not be eliminated. This suggested that copper ionophores induced cell death was a mechanism quite different from the known mode of cell death. Meanwhile, the researchers observed that cells that relied more on mitochondrial respiration were about 1000 times more sensitive to the copper inducer than cells that relied on glycolysis. Treatment with mitochondrial antioxidants, fatty acids and mitochondrial function inhibitors significantly changed the sensitivity of cells to copper ions. In addition, electron transport chain (ETC) complex inhibitors, as well as inhibition of mitochondrial pyruvate uptake, reduced cupric-induced cell death, while none of these inhibitors had an effect on ferroptosis. At the same time, it was found that the content of tricarboxylic acid cycle (TCA) related metabolites changed in copper ionophores treated cells, suggesting that copper ionophores induced cell death may act on the TCA stage. To further explore the metabolic pathway of cuproptosis, genome-wide CRISPR-Cas9 loss of function screening identified seven genes, including ferredoxin 1 (FDX1), associated with copper ionophores induced cell death. It had been confirmed that FDX1 and protein lipid acylation were the key factors of copper ionophores induced cell death. Excess copper promoted the aggregation and disfunction of fatty acylated proteins, triggering instability of ferrothiotubulin, leading to proteotoxic stress, and ultimately cell death. Overall, the team identified a new type of cell death that they named cuproptosis, to distinguish it from existing cell death methods. The main process of cuproptosis depended on the accumulation of copper ions in the cell. The identified mechanism of cuproptosis, which involves the direct binding of copper ions to fatty acylation components in the TCA cycle leading to protein aggregation and imbalance, is a novel form of cell death. The study revealed that FDX1 is a key regulator of cuproptosis and the upstream regulator of protein lipid acylation, which is highly correlated with various human tumors. The sensitivity of cell lines to cuproptosis is associated with the abundance of FDX1 and fatty acylated proteins, suggesting that copper ionophores may have therapeutic potential in targeting cancer cells with such metabolic characteristics (Figure 7A).115 However, further research is required to fully understand the specific mechanisms of cuproptosis.
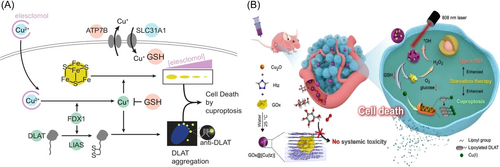
Subsequently, Cu-based nanoparticles were blowout applied to cuproptosis. Pan at al. reported a nonporous copper(I) coordination polymer nanoplatform loaded glucose oxidase (GOx) (GOx@[Cu(tz)]) for cuproptosis-based dynergistic cancer therapy. In this paper, they combined GOx with [Cu(tz)] to simultaneously increase the level of Cu and reduce the level of glucose and GSH in tumor cells, thus improving the sensitivity of cancer cells to cuproptosis (Figure 7B).65 This study demonstrates the application of nanocarriers in cuproptosis, but the relationship between Cu and cuproptosis is still unclear, such as the relationship of Cu valence (Cu0, Cu1+, and Cu2+), the Cu containing nanocarriers (CuS, CuO, and CuP), other metal ions (Fe2+, Zn2+, and Ca2+) and cuproptosis.
4.11 Immunotherapy based on Cu nanoparticles
Over the past few decades, immunotherapy has emerged as one of the most significant treatment approaches. However, the lack of T-cells and the immunosuppressive milieu severely restrict the clinical use of immunotherapy. Copper plays a crucial role in regulating immune function, and its deficiency can result in a decline of immune function. In copper-deficient mice, the level of interleukin was found to be only 40%–50% of that in normal mice. Moreover, increased serum copper levels were observed in various infections, which stimulated liver synthesis and release of ceruloplasmin, thus promoting resistance to microbial invasion. The elevation of blood copper levels is primarily attributed to a leukocyte endogenous substance secreted during the activation of neutrophils and macrophages. This substance is transported to the relevant target cells via the bloodstream and plays a critical role in immune regulation and sterilization. Many studies have shown that copper deficiency can affect the development of immune organs and normal immune function. The growth and development of immune organs in mice with severe copper deficiency were observed by biochemical and morphological methods, and spleen enlargement and thymus shrinkage were found. Thymus and spleen atrophy and decreased thymus weight were reported in copper deficient rats. T cells are the main participants of cellular immunity in animals and can assist humoral immunity of B cells. Copper plays an important role in T cell proliferation, assisting T cells and B cells. Copper deficiency can alter the composition of lymphoid tissue, and T cells are more sensitive to copper deficiency than B cells. T cells mature in the thymus and gradually differentiate into different subgroups with complementary and cytotoxic functions. Studies have shown that the number and percentage of CD4+ and CD8+ cells in T lymphocytes of copper deficient male rats decreased. The amount of copper can be increased by adding copper. Adding copper to feed can improve the cellular immune function of animals and enhance the body resistance. As a growth promoting agent, copper is widely used in culture production. Proper amount of copper can maintain the immune function of the body and promote the cellular and humoral immunity of the body. Although copper can promote growth and contribute to the play of immune function, it should not be added to feed without limit.
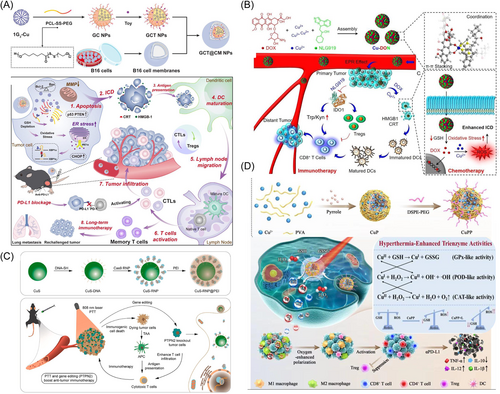
Recently, immunogenic cell death (ICD) with damage-associated molecular patterns (DAMPs) released from dying tumor cells as robust antigenic and adjuvant signals attracted increasing attention in antitumor immunotherapy. Various therapies, such as chemotherapy, PDT, PTT, CDT, RT, and so on. have been reported to incite the ICD-related immune response. The corresponding Cu-based therapy can still stimulate ICD. Shi et al. reported a biomimetic polymeric nanoparticle coloaded with phosphorus containing dendrimer copper complex (1G3-Cu) and endoplasmic reticulum stress drug fengjiamycin (Toy) for chemotherapy enhanced tumor immunotherapy, and further combined with programmed cell death-ligand 1 (PD-L1) antibody to activate long-term and sustained antitumor immune response (Figure 8A).116 CuS nanoparticles mediated PTT synergistically ablated tumors and promoted ICD to amplify antitumor efficacy (Figure 8B).117 Intracellular redox imbalance can be brought up by Cu-mediated GSH consumption and oxidative stress, which will further encourage ICD response (Figure 8C).118 Moreover, the CAT-like activity of Cu was reported to alleviate tumor hypoxia, reduce the antioxidant level and improve oxidative stress, thus inducing the polarizing of M2-type to M1-type tumor associated macrophage (TAM), reversing tumor immunosuppressive microenvironment and enhancing immunotherapy (Figure 8D).119 These studies have shown the effect of Cu and immunotherapy via ICD, but whether Cu metabolism directly affecting the function of immune cells has not been studied.
5 CONCLUSIONS AND OUTLOOK
This review summarizes the multimodal copper therapeutic strategies reported at present, focusing on the nanotechnology-based antitumor therapies with copper depletion and copper supplementation, to promote the development of copper antitumor therapies, collaborative application of copper therapy and other excellent treatment methods, and various multimodal anticancer drugs that affect copper metabolism. Great progress has been made in the research of various inorganic nanomaterials for tumor therapy. However, unfortunately, the biocompatibility of inorganic nanomaterials is still the bottleneck that hinders their clinical application. Based on the special biological effects of copper ions, the authors believe that the special biological effects of functional ions or ion clusters generated by the degradation of nanomaterials (including inorganic nanomaterials) can be utilized to interfere with or hinder the metabolism and proliferation process of tumor cells, or in a broad sense, by regulating the interaction between bioactive ions and the physiological process of tumor cells. It can induce metabolic disorder of tumor cells and inhibit tumor growth and metastasis. This novel tumor therapy strategy will open up a new way for the application of inorganic nanomaterials in clinical tumor therapy. Although copper therapy has made substantial progress and breakthrough, some unresolved problems and challenges need to be solved before practical clinical application. Increasing observations have linked copper signals with tumor proliferation and metastasis. However, more basic mechanisms are needed to be established causality rather than correlation, and further connect copper-dependent targets and pathways with diseases. The relationship between Cu and cancer, microenvironment, and inflammatory response, needs to be further researched. To improve therapeutic efficiency and specificity, delivering therapeutic medicines to specific cells (tumor cells, tumor vascular endothelial cells) or even subcellular regions (mitochondria, lysosomes, and Golgi) remain challenging. Increasing evidence have shown that the efficiency of nanodrugs accumulated at the tumor sites is less than 10% only via EPR effect, resulting in poor performance in vivo. Nanodrugs with the appropriate size and targeting group need to be designed. The clinical application of copper-based nanodrugs depends on their solubility, biocompatibility, and biosafety. Copper-based catalysis therapy is closely related to the composition, morphology, size, and surface functionalization of the nanomaterials. The mechanism of ROS produced by Fenton/Fenton-like reaction in vivo should be further investigated because the complex physiological system may greatly change the catalytic efficiency of Fenton/Fenton-like reaction. Numerous methods for achieving copper therapy have been proposed thanks to the advancements in nanotechnology and medicinal chemistry. Therefore, to promote the rapid development of this field, a unified evaluation system is essential to be established to assess their therapeutic effect.
AUTHOR CONTRIBUTIONS
Yongjuan Li: Conceptualization (equal); data curation (equal); formal analysis (equal); resources (equal); visualization (equal); writing—original draft (equal). Ya Dong: Data curation (equal); formal analysis (equal); investigation (equal); writing—original draft (equal). Xinyao Zhou: Writing—original draft (equal); writing—review and editing (equal). Kelong Fan: Conceptualization (equal); project administration (equal); supervision (equal); writing—original draft (equal); writing—review and editing (equal). All authors have read and approved the final manuscript.
ACKNOWLEDGMENTS
We would like to thank Home-for-Researchers, China, for help with drawing the Figure 1 with 3D Studio Max and Adobe illustrator. This work was supported by the National Natural Science Foundation of China (52103190), the National Key Research and Development Program of China (No. 2021YFA1201102).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
Not applicable.
Open Research
DATA AVAILABILITY STATEMENT
Not applicable.




