Impact of occlusive material and cochlea-carotid artery relation on eustachian tube occlusion in subtotal petrosectomy
Abstract
Objective
To evaluate the success rate of eustachian tube (ET) occlusion in subtotal petrosectomy relative to the occlusive material used and to the varying protympanum anatomy, by means of standardized alignment of the cochlea-carotid artery relation on computed tomography images.
Patients and methods
All cases of subtotal petrosectomy carried out by the same surgeon at a tertiary care referral center were retrospectively evaluated. Only cases with available computed tomography prior to second stage cochlear or middle ear implantation were included. The occlusive material was either muscle tissue or oxidized regenerated cellulose in combination with bone wax. On 3D multiplanar image reconstruction, the varying topographic interrelation of the cochlea and the petrous carotid artery was measured and categorized into two groups: detachment or overlapping.
Results
In 9 (31%) of the 29 included cases there was insufficient occlusion of the ET. In none of these cases was an infection of the fat filling in the obliterated cavity observed during the implantation procedure on second stage (average 10 months interval). The failure rate of both occlusion materials was almost the same (using muscle tissue, in 4 (33.3%) of 12 or oxidized regenerated cellulose, in 5 (29.4%) of 17 cases). It was also similar for both materials in each of the anatomic variation groups.
Conclusions
An incomplete occlusion of the ET alone does not appear to lead to an infection of the obliterated cavity. Autologous muscle tissue and oxidized regenerated cellulose had similar rates of ET occlusion failure. The topographical variance of the protympanum appears to have no direct influence on the success of the ET occlusion.
1 INTRODUCTION
Subtotal petrosectomy is a well-established surgical procedure that enables hearing restoration by means of cochlear implants and active middle ear implants in challenging cases with chronic and recurrent otitis media. The revision rate after subtotal petrosectomy caused by infection of the fat filling of the obliterated cavity varies widely in the literature from 0% to 16% of the operated cases.1 Besides closure of the external auditory canal and complete removal of the infected mucosa, occlusion of the tympanic orifice of the eustachian tube (ET) have been thought to prevent fat graft infection.2 However, the efficacy and benefit of ET occlusion in subtotal petrosectomy is unknown, so that its role as a source of infection is questionable.
The present study evaluates the success rate of this surgical step using two different occlusive materials. Additionally, it explores whether there is an anatomic predisposition for insufficient ET occlusion in subtotal petrosectomy using objective comparison of varying protympanum anatomy in different patients. For this purpose, a method for standardization of the topographical interrelation between the cochlea and the petrous carotid artery on computed tomography images was developed.
2 MATERIALS AND METHODS
2.1 Patients
All cases of subtotal petrosectomy with abdominal fat obliteration of the resulting tympanomastoidal cavity carried out by a single experienced surgeon (senior author) at a tertiary care referral center were retrospectively evaluated. This study was conducted in line with the ethical standards of the institutional review board. All cases had already undergone multiple ear operations due to chronic otitis media with dry radical cavity or active inflammation and were carried out in a 10-year period in preparation for implantation of active middle ear implants (vibrant soundbridge, bone bridge, middle ear transducer, direct acoustic stimulator) or cochlear implant. Only cases with available computed tomography (in all cases cone beam computed tomography) prior to the second stage hearing aid implantation were included.
2.2 Surgical technique
After creating a common tympanomastoidal cavity all epithelial and inflammatory tissue was meticulously removed, the tympanic orifice of the ET was blocked, the external auditory canal was closed in blind sac, and the compartmentalized cavity was obliterated with abdominal fat.
2.3 Data acquisition
Temporal bone cone beam computed tomography data was performed on a stationary Xoran MiniCAT (Ann Arbor, Michigan) equipped with a 536 × 536 matrix detector resulting in 0.3 mm3 isotropic voxel (standard department protocol: 125 kVp, 7 mA).
The success of ET occlusion was determined according to the aeration of the obliterated cleft on computed tomography and was correlated to the material for occlusion and the topography of the protympanum.
2.4 Occlusive material
The material used for ET occlusion was either temporalis muscle tissue (n = 12) or oxidized regenerated cellulose (Surgicel, Ethicon, Somerville, NJ, n = 17), both supported by bone wax.
2.5 Protympanum anatomy
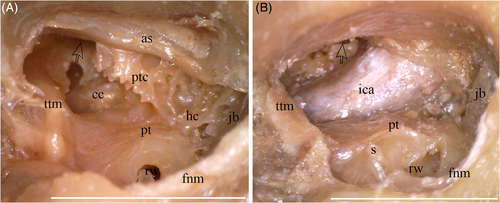
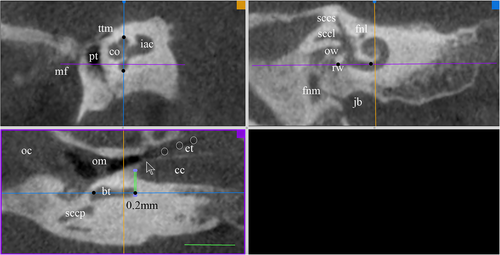
The cochlea-carotid artery relation, which determines the form of the protympanum and of the tympanic orifice of the ET was assessed (Figure 1). DICOM data processing was performed with imaging software Osirix MD (Pixmeo, Los Angeles, California). Evaluation and measurements were performed in standardized alignment using three-dimensional multiplanar reconstruction which provides three windows, for the three main orthogonal planes (Figure 2). The reference plane (bottom left window, violet) was set through the maximal length of the basal cochlear turn and then in a second section (top right window, blue) it was readjusted as a line through the upper edge of the round window running directly under the modiolus. The third plane (top left window, orange) was determined from the first two. Finally, the interrelation between the basal turn of the cochlea and the bony carotid canal was categorized as detachment or overlapping of both structures and the interval was measured parallel to the blue plane (Figure 3). Our objective was not to determine the minimum distance between these varying structures, but to set a standard alignment for further analysis and comparable measurements.
3 RESULTS
11 (15.3%) of the 72 reviewed cases underwent revision surgery because of dehiscence of the wound closure retroarticular or in the ear canal. At the time of data acquisition, 9 (12.5%) had not received an implant and 3 (4.2%) were simultaneously implanted. All 29 patients who met the above-mentioned inclusion criteria were adult (17 female, 12 male, average age 61 years, range 27 to 81 years). The interval between the evaluated second stage implantation procedure to the initial subtotal petrosectomy ranged from 4 to 28 months (average 10 months). In 9 (31%) of the cases there was insufficient occlusion of the ET, with air in the obliterated cavity to varying extent (Figure 4). In none of these cases was an infection of the fat graft observed. There were also no signs of foreign body reaction caused by Surgical or bone wax.
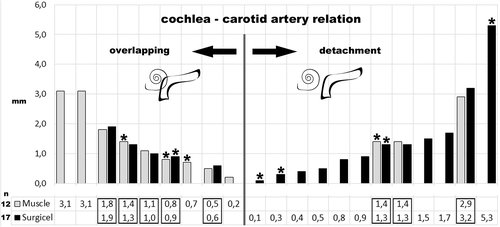
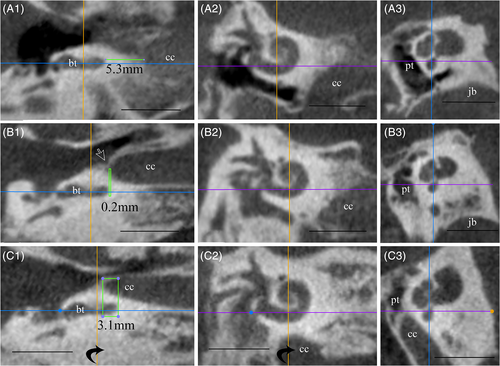
The failure rate of both occlusion materials was similar (using muscle tissue, in 4 (33.3%) of 12 or oxidized regenerated cellulose, in 5 (29.4%) of 17 cases, Figure 4). The topographical interrelation of the above-mentioned landmarks varied from overlapping (average 1.3 mm, range 0.2 to 3.1 mm) to detachment (average 1.5 mm, range 0.1 to 5.3 mm). Insufficient ET occlusion could be seen in 4 (28.6%) of all 14 cases with overlapping (with muscle, 3 (33.3%) of 9 or with Surgicel, 1 (20%) of 5 cases) and in 5 (33.3%) of all 15 cases with detachment (irrespective of the occlusive material 33.3%; with muscle, 1 of 3 or with Surgicel, 4 of 12 cases).
To minimize the influence of the anatomic variable 16 of the 29 cases could be matched in 8 pairs of different material but similar cochlea-carotid artery relation distance, 5 in the overlapping and 3 in the detachment category. In all but one of all these pairs the same occlusion result was achieved (Figure 4).
4 DISCUSSION
This study evaluates influential factors for insufficient ET occlusion in subtotal petrosectomy with the intention to weigh benefit against potential risk of this surgical step. There are many reasons for postoperative infection of the fat graft, the main one undoubtedly being residual infected mucosa in bony cells.3 Since all the included cases in the current study were infection free during the second stage implantation, their evaluation could retrospectively give some insight into the role of ET occlusion alone in prevention of infection.
In the first aspect of the study, two occlusion materials were compared. These vary in the literature from different autologous soft tissues to inert materials as well as combinations of both: periosteum, free temporalis muscle graft with fascia4 or in combination with connective tissue,5 folded back tensor tympani muscle,6 small cartilage fragments from the outer ear canal,7 bone pate,8 bioactive ionomeric cement,9 incus with inverting of the mucosa,10 hydroxyapatite cement,11 and oxidized regenerated cellulose12 with or without supporting materials like bone wax or fibrin sealant. An overview of the pertinent literature did not reveal consensus of which one is optimal or even how effective the intended occlusion is. The present results show that there is essentially no difference in the success rate between the use of autologous muscle fragments and resorbable inert material like oxidized regenerated cellulose.
In none of our cases was there a clinically relevant foreign body reaction of the used bone wax. Although rare, such complication has been previously reported, and its application in subtotal petrosectomy should therefore be carefully reconsidered.13, 14 In contrast to bone wax, on histopathological examination Surgicel provokes fewer foreign body giant cells and elicits no inflammation.15
It is not the material alone, but rather the occlusion technique which seems to play the decisive role. ET occlusion only makes sense if the communicating peritubar cells are also blocked (Figure 1). If they are not drilled smooth, the mucosa in this area cannot be completely removed. Furthermore, since these cells usually aerate in the ET, sufficient obliteration will not be achieved. Jen and colleagues found on computed tomography with 1-mm slices that in temporal bones with petrous apex pneumatization the incidence of peritubal cells opening into the ET anterior to the tympanic orifice was 92%.16 The communication was in the lateral one third of the ET in 56%, in the middle one-third in 42%, and in the anterior one-third in 2%. Furthermore, Saim and colleagues found that in 120 adult temporal bones the incidence of peritubal cells was 65%.17 In 59% of all specimens the peritubal cells open directly into the ET and in 23% this connection could be histologically verified more than 5 mm anterior of a reference line representing the beginning of the osseous ET. They reported a case with occlusion failure and recurrent cerebrospinal fluid otorhinorrhea after skull base surgery in which they had to skeletonize the internal carotid artery to reach these peritubal cells in order to exteriorise them into the common cavity. The re-occlusion of the ET with temporalis fascia and bone wax was only then successful. The risk of injuring the internal carotid artery in such cases should be weighed against the risk for meningitis. However, in our opinion the potential risk for infection of the fat graft through the ET in elective subtotal petrosectomy for chronic otitis media cannot justify such extensive dissection around the carotid artery.
Another potential cause for insufficient occlusion is the funnel- and slope-like form of the tympanic ostium of the ET after the peritubal cells have been drilled out. Because of the resulting smooth bony surface inlay materials like soft tissue or Surgicel cannot adhere firmly on the bone due to scar tissue and are likely to loosen.
The second aspect of the study was analysis of the varying topography of the protympanum and its influence on ET occlusion. Lack of everyday experience in ear surgery in this area could make this procedure an ordeal, especially for an inexperienced surgeon who nevertheless should be aware of the complex anatomy, and understand the interrelation between the cochlea and the petrous carotid artery. Penido and colleagues found on histologic sections of 122 temporal bones that most frequently the smallest distance between the cochlea and the carotid canal is located in the basal turn and ranges from 0.33 to 4.33 mm.18 On the other hand, the basal turn is well-defined on computed tomography images. For this reason, we chose the basal turn as a reference landmark in the above described alignment of the computed tomography dataset. The standardized view of the protympanum shows that in cases of detachment, the transverse segment of the canal is hardly seen, the curvature of the carotid canal is more medial compared with the cochlea and is separated from the osseous ET from peritubal cells (Figure 3A). However, with increase of overlapping, the artery runs further lateral to the reference line (Figure 3B). In the case of maximal overlapping, the vessel bulges in the protympanum and reduces the lumen of the tympanic orifice of the ET (Figure 3C). In such cases the tiny carotid wall is the medial wall of the osseous path to the ET isthmus. After subtotal petrosectomy in typical surgical view along the promontory, the proximal carotid artery close to the annular sulcus is higher than the distal vertical segment (Figure 1B). This anatomical feature should be kept in mind since the anterior hypotympanal cells and the peritubal cells lay over the carotid canal. By drilling in such a narrow blind ending on a bone-to-soft tissue interface, the diamond burr can easily flip into the carotid canal.
In the literature, the incidence of carotid canal dehiscence in human temporal bones ranges widely from 4.9% to 35.2%.18, 19 Moreano and colleagues who examined the largest number of serial sectioned temporal bones found 7.7% with dehiscence, additionally 7.4% with a microdehiscence and 15.5% with a wafer-thin carotid canal wall in 1000 specimens.20 Furthermore, Savic and Djeric reported in 150 specimens 22.2% with a wafer-thin carotid canal wall, and which in 2% was even missing.21 The maximal bone thickness which separated the ET from the internal carotid artery was 3 mm.
Pauna and colleagues found on serial histological sections an increased incidence of carotid canal dehiscence in temporal bones of deceased donors with chronic otitis media compared to a control group.22 The dehiscence, which was frequently closer to the promontory, was larger in size and the bony wall (when present) was thinner compared to findings in non-diseased ears. On the other hand, in cases with active chronic otitis media the mucosa is usually scarred, hyperplastic and vulnerable with good blood supply so that its removal is performed under a suboptimal operative view. Injuring the caroticotympanic artery from the carotid canal additionally can worsen the orientation in the surgical field.
The petrous carotid artery has a thin vein-like wall, which lacks muscle and elastic fibers and does not pulsate.23 Moreover, in aged patients the wall of the internal carotid artery is often atherosclerotic, dilated and thinned, so that the bony carotid canal stabilizes its lumen. Sometimes it can even be totally atrophied and the bony canal replaces the artery wall, meaning that if the bony scaffold is opened, the artery could be easily injured.24 However, since in 96% of temporal bones the carotid artery forms a barrier between the air spaces anterior and posterior, particular attention to the carotid artery is warranted to achieve successful ET occlusion.25
Ugo Fisch, the name giver of “subtotal petrosectomy,” recommended that the internal carotid artery should be followed with diamond burr in order to remove the bony ET as far as the isthmus.26 After the mucosa is coagulated the obliteration should be done “with bone wax, which is firmly packed with a suction tip covered with a neurosurgical cottonoid.” However, he described this technique primarily as an approach to the lateral skull base and not as an eradication procedure for chronic otitis media.
Taking all facts mentioned above into consideration, as well as the fact that most of the patients undergoing subtotal petrosectomy in preparation for hearing implants have a clinical history of multiple curative surgeries for chronic otitis media, there is an increased risk of injuring or plugging the carotid artery in its dehiscent or iatrogenic weakened bony canal by pushing the occluding material firmly into a funnel like ET orifice. Therefore, the surgeon should consider how much risk is reasonable to take for sufficient occlusion. In the presented case series, after the mucosa of the protympanum was removed with diamond drill without opening the carotid canal, the occlusive material was pushed gently into the tympanic orifice.
It should also be considered that sequelae from iatrogenic trauma of the artery wall could remain unrecognized. Vascular stenosis of the carotid artery through atheromatous plaques is not rare in aged individuals. Furthermore, soft and vulnerable plaques in the petrous segment are a diagnostic challenge and could remain invisible in preoperative magnetic resonance imaging workup without special sequences.27 Consequently, manipulation of the carotid artery wall could potentially lead in such cases to plaque rupture and in the long-term to clinically relevant arterial stenosis, which would not be directly connected to the operation.
Knowledge of the exact location of the carotid canal can minimize the risk of accidental injury to the internal carotid artery and would assist the surgeon to drill more safely in this region. Detailed preoperative assessment of the individual anatomy of the patient with computed tomography scans is easily facilitated by using three-dimensional multiplanar reconstruction as shown in Figure 2.
An interesting alternative for traditional transtympanal ET closure is endonasal ablation for which various surgical techniques have already been described in the literature.28 Almost all these were developed to address recalcitrant cerebrospinal fluid rhinorrhea after skull base surgery and none describe a problem of simultaneous infection of the fat graft with insufficient ET occlusion. Barañano and colleagues used such a technique in a case of subtotal petrosectomy for chronic otitis media with aeration of the obliterated cavity 8 months after surgery in which they successfully closed the ET transnasally by ablation using fat tissue from the ear lobe in monitored anesthesia care.29 Unfortunately, they did not explain why they decided to perform revision of this “noninfectious complication” 8 months after the initial obliterative surgery.
Finally, a prospective study should assess whether transtympanic ET occlusion after subtotal petrosectomy for eradication of chronic otitis media has any role in the prevention of fat graft infection in the obliterated cavity. The findings of such a study could make it easier for ear surgeons to decide how far they should proceed drilling into the protympanum to achieve successful ET occlusion and whether this surgical step is even necessary.
5 CONCLUSION
In our study, an incomplete occlusion of the eustachian tube after subtotal petrosectomy does not appear to lead to an infection of the obliterated cavity. Autologous tissue, such as temporalis muscle, may be considered to be just as suitable for tube occlusion as an inert material like oxidized regenerated cellulose. The topographical variance of the protympanum seems to have no direct influence on the success of ET occlusion.
ACKNOWLEDGMENT
Human temporal bones were acquired from autopsies of elderly subjects in line with the donation program of the institution. The authors acknowledge the contribution made by the donors of the tissue. We would like to thank Mr. P. James for proofreading of the manuscript.
CONFLICT OF INTEREST
The authors have no conflict of interest to declare. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.