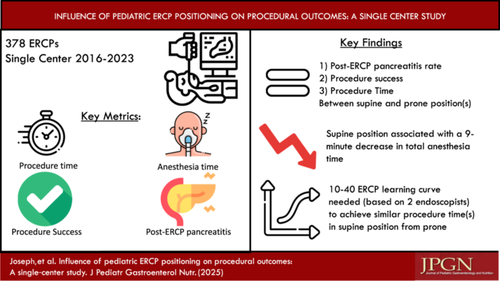
Influence of pediatric ERCP positioning on procedural outcomes: A single-center study
Abstract
Objectives
Endoscopic retrograde cholangiopancreatography (ERCP) is traditionally done in the prone position. In pediatrics, patient anatomy and anesthesia practices are considerations that affect procedural success and anesthesia time. The aim of our study was to evaluate the safety, procedural success, and efficiency of pediatric ERCP in the prone versus supine positions.
Methods
ERCPs from September 2016 to August 2023 were reviewed at our center. Demographic and procedure variables were collected. Multivariate linear regression was performed to determine the effect of patient position on total anesthesia time.
Results
Two hundred and eighty-three patients (378 ERCPs) were included. There were significant differences in fellow involvement, proportion of native papillae, procedural indication, and total anesthesia time by ERCP position. Multivariate linear regression found that supine position was associated with 9.3-min decrease in anesthesia time and American Society of Anesthesiologists Class 1 or 2 was associated with 10.6-min decrease in anesthesia time. Factors that were associated with increased anesthesia time were additional procedure, increased procedure time, and native papilla. Finally, we found a learning curve for transitioning from prone to supine position was between 10 and 40 cases. After the learning curve, we found 11-min decrease in mean procedure time and 16-min decrease in total anesthesia time in the supine position.
Conclusions
This is the first pediatric study to evaluate the role of patient positioning on ERCP outcomes and total anesthesia time. Given similar procedural outcomes, the impact of increased anesthesia time on neurodevelopment in children, and the cost to the patient, the supine position may be preferred to a prone position.
Graphical Abstract
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.