Parent-child interaction is related to emotional and behavioral problems in pediatric intestinal failure
Rozemarijn A. L. Duister
Department of Pediatrics, Division of Gastroenterology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorLotte E. Vlug
Department of Pediatrics, Division of Gastroenterology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorMerit M. Tabbers
Department of Pediatrics, division of Gastroenterology, Hepatology and Nutrition, Emma Children's Hospital, Amsterdam University Medical Centers, Amsterdam, The Netherlands
Search for more papers by this authorEdmond H. H. M. Rings
Department of Pediatrics, Division of Gastroenterology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorRené M.H. Wijnen
Department of Pediatric Surgery, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorMarjolein Spoel
Department of Pediatric Surgery, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorCorresponding Author
Barbara A. E. de Koning
Department of Pediatrics, Division of Gastroenterology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Correspondence Barbara A. E. de Koning, Department of Pediatrics, division of Gastroenterology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Dr. Molewaterplein 40, 3015 GD, Rotterdam, The Netherlands.
Email: [email protected]
Search for more papers by this authorJeroen S. Legerstee
Department of Child and Adolescent Psychiatry/Psychology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorMijke P. Lambregtse-van den Berg
Department of Child and Adolescent Psychiatry/Psychology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Department of Psychiatry, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorthe PICASsO Group
Search for more papers by this authorRozemarijn A. L. Duister
Department of Pediatrics, Division of Gastroenterology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorLotte E. Vlug
Department of Pediatrics, Division of Gastroenterology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorMerit M. Tabbers
Department of Pediatrics, division of Gastroenterology, Hepatology and Nutrition, Emma Children's Hospital, Amsterdam University Medical Centers, Amsterdam, The Netherlands
Search for more papers by this authorEdmond H. H. M. Rings
Department of Pediatrics, Division of Gastroenterology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorRené M.H. Wijnen
Department of Pediatric Surgery, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorMarjolein Spoel
Department of Pediatric Surgery, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorCorresponding Author
Barbara A. E. de Koning
Department of Pediatrics, Division of Gastroenterology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Correspondence Barbara A. E. de Koning, Department of Pediatrics, division of Gastroenterology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Dr. Molewaterplein 40, 3015 GD, Rotterdam, The Netherlands.
Email: [email protected]
Search for more papers by this authorJeroen S. Legerstee
Department of Child and Adolescent Psychiatry/Psychology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorMijke P. Lambregtse-van den Berg
Department of Child and Adolescent Psychiatry/Psychology, Erasmus MC Sophia Children's Hospital, University Medical Center Rotterdam, Rotterdam, The Netherlands
Department of Psychiatry, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands
Search for more papers by this authorthe PICASsO Group
Search for more papers by this authorRozemarijn A.L. Duister and Lotte E. Vlug are contributed equally to the study and therefore share first authorship.
Clinical Trial Registration (if any): MEC 2019-098, Dutch Trial Register NL8964, https://trialsearch.who.int/Trial2.aspx?TrialID=NL8964.
Abstract
Objectives
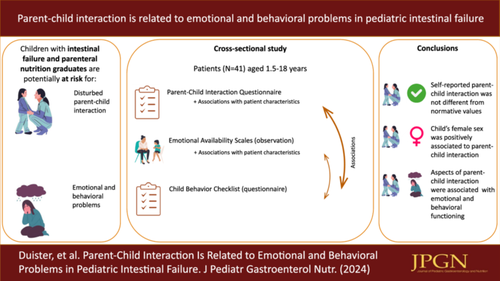
Parent-child interaction in pediatric intestinal failure (IF) and in parenteral nutrition (PN) graduates can be disturbed due to parental responsibilities related to the condition, and could affect the child's emotional and behavioral functioning (EBF). The aim was to assess parent-child interaction, to examine associations with clinical features, and to relate parent-child interaction to EBF.
Methods
A cross-sectional study of IF patients and PN graduates aged 1.5−18 years and one primary caregiver was performed in two Dutch multidisciplinary pediatric IF teams. Parent-child interaction was observed using the Emotional Availability Scales (EAS), reported with the Parent Child Interaction Questionnaire (PACHIQ) and compared to normvalues when available. Associations between parent-child interaction and clinical factors and EBF were examined. EBF was assessed using the Child Behavior Checklist. All measures are validated.
Results
A total of 41 parent-child dyads were included, 17 (41.4%) received PN at time of assessment and median age was 8.9 [interquartile range 5.8−11.9] years. No significant differences in parent-reported interaction compared to normative values or between PN-receiving and weaned children were found. Exploratory multivariable regression indicated that only the child's female sex was significantly positively related to parent-child interaction. Parent-child interaction was negatively related to EBF for nonhostility, conflict resolution, and acceptance.
Conclusion
Our findings suggest that (self-reported) parent-child interaction in IF patients and PN graduates is not significantly different as compared to healthy peers, and unrelated to clinical characteristics. However, aspects of parent-child interaction were correlated to EBF, potentially being a target for prevention or intervention in children with diminished EBF.
Graphical Abstract
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
REFERENCES
- 1Goulet O, Ruemmele F, Lacaille F, Colomb V. Irreversible intestinal failure. J Pediatr Gastroenterol Nutr. 2004; 38(3): 250-269.
- 2Hess RA, Welch KB, Brown PI, Teitelbaum DH. Survival outcomes of pediatric intestinal failure patients: analysis of factors contributing to improved survival over the past two decades. J Surg Res. 2011; 170(1): 27-31.
- 3Bondi BC, Gold A, Belza C, et al. Predictors of Social-Emotional development and adaptive functioning in School-Age children with intestinal failure. J Clin Psychol Med Settings. 2023; 30(3): 589-605.
- 4Nagelkerke SCJ, van Oers HA, Haverman L, et al. Longitudinal development of health-related quality of life and fatigue in children on home parenteral nutrition. J Pediatr Gastroenterol Nutr. 2022; 74(1): 116-122.
- 5Vlug LE, Legerstee JS, Tabbers MM, et al. Children with intestinal failure are at risk for psychopathology and trauma. J Ped Gastroenterol Nutrition. 2023; 77(6): e104-e113.
- 6Querido JGES. Assessment of parent-child interactions. In: THSC Ollendick. Encyclopedia of Clinical Child and Pediatric Psychology. Kluwer Academic/Plenum; 2003.
- 7Belza C, Patterson C, Ghent E, et al. “Line care governs our entire world”: understanding the experience of caregivers of children with intestinal failure receiving long-term parenteral nutrition. J Parent Enteral Nutri. 2022; 46(7): 1602-1613.
- 8Cousino MK, Hazen RA. Parenting stress among caregivers of children with chronic illness: a systematic review. J Pediatr Psychol. 2013; 38(8): 809-828.
- 9Belza C, Ungar WJ, Avitzur Y, Stremler R, Fehlings D, Wales PW. Carrying the burden: informal care requirements by caregivers of children with intestinal failure receiving home parenteral nutrition. J Pediatr. 2022; 250: 75-82.
- 10Dudek-Shriber L. Parent stress in the neonatal intensive care unit and the influence of parent and infant characteristics. Am J Occup Ther. 2004; 58(5): 509-520.
- 11Hopkins J, Cermak SA, Merritt RJ. Oral feeding difficulties in children with short bowel syndrome: a narrative review. Nutr Clin Pract. 2018; 33(1): 99-106.
- 12Power N, Franck L. Parent participation in the care of hospitalized children: a systematic review. J Adv Nurs. 2008; 62(6): 622-641.
- 13van Oers HA, Haverman L, Limperg PF, van Dijk-Lokkart EM, Maurice-Stam H, Grootenhuis MA. Anxiety and depression in mothers and fathers of a chronically ill child. Matern Child Health J. 2014; 18(8): 1993-2002.
- 14van Oers HA, Haverman L, Olieman JF, et al. Health-related quality of life, anxiety, depression and distress of mothers and fathers of children on home parenteral nutrition. Clin Nutr. 2019; 38(4): 1905-1912.
- 15Halsey M, Hodgson K, Russell R, et al. Emotional wellbeing in parents of children on home parenteral nutrition. J Pediatr Gastroenterol Nutr. 2020; 71(4): 557-562.
- 16Engström I, Björnestam B, Finkel Y, Engström I, Björnestam B, Finkel Y. Psychological distress associated with home parenteral nutrition in Swedish children, adolescents, and their parents: preliminary results. J Pediatr Gastroenterol Nutr. 2003; 37(3): 246-250.
- 17Bohlin G, Hagekull B, Rydell A-M. Attachment and social functioning: a longitudinal study from infancy to middle childhood. Social Develop. 2000; 9(1): 24-39.
- 18Merritt RJ, Cohran V, Raphael BP, et al. Intestinal rehabilitation programs in the management of pediatric intestinal failure and short bowel syndrome. J Pediatr Gastroenterol Nutr. 2017; 65(5): 588-596.
- 19Biringen Z. The Emotional Availability (EA) Scales Manual. 4th Edn. International Center for Excellence in Emotional Availability; 2008.
- 20Biringen Z, Easterbrooks MA. Emotional availability: concept, research, and window on developmental psychopathology. Dev Psychopathol. 2012; 24(1): 1-8.
- 21Kogan N, Carter AS. Mother-infant reengagement following the still-face: the role of maternal emotional availability an infant affect regulation. Infant Behav Develop. 1996; 19: 359-370.
- 22Bornstein MH, Gini M, Putnick DL, Haynes OM, Painter KM, Suwalsky JTD. Short-Term reliability and continuity of emotional availability in mother-child dyads across contexts of observation. Infancy. 2006; 10(1): 1-16.
- 23Lange A. OKIV-R. Ouder Kind Interactie Vragenlijst Revised. Handleiding [Parent-Child Interaction Questionnaire Revised. Manual]. Bohn Stafleu van Loghum; 2009.
- 24Lange A, Evers A, Jansen H, Dolan C. PACHIQ-R: the Parent-Child Interaction Questionnaire—revised. Fam Process. 2002; 41(4): 709-722.
- 25Achenbach T, Rescorla M, Leslie A. Manual for the ASEBA Child Behavior Checklists for Ages 1.5-5 years (CBCL/1.5-5). University of Vermont, Research Center for Children, Youth, & Families; 2001.
- 26Achenbach TMRL. Manual for the ASEBA school-age forms & profiles: child behavior checklist for ages 6-18, teacher's report form, youth self-report: an integrated system of multi-informant assessment: University of Vermont, research center for children youth & families. 2001.
- 27Holmbeck GN, Thill AW, Bachanas P, et al. Evidence-based assessment in pediatric psychology: measures of psychosocial adjustment and psychopathology. J Pediatr Psychol. 2008; 33(9): 958-980.
- 28Pinquart M. Do the parent-child relationship and parenting behaviors differ between families with a child with and without chronic illness? A meta-analysis. J Pediatr Psychol. 2013; 38(7): 708-721.
- 29Cassibba R, van IJzendoorn MH, Coppola G. Emotional availability and attachment across generations: variations in patterns associated with infant health risk status. Child Care Health Dev. 2012; 38(4): 538-544.
- 30Golics CJ, Basra MKA, Finlay AY, Salek S. The impact of disease on family members: a critical aspect of medical care. J R Soc Med. 2013; 106(10): 399-407.
- 31Silver HJ. The lived experience of home total parenteral nutrition: an online qualitative inquiry with adults, children, and mothers. Nutr Clin Pract. 2004; 19(3): 297-304.
- 32Stack DM, Matte-Gagné C, Dickson DJ. Persistence of effects of VLBW/PT birth status and maternal emotional availability (EA) on child EA trajectories. Front Psychol. 2019; 9: 2715.
- 33Salvatori P, Neri E, Chirico I, Andrei F, Agostini F, Trombini E. Mother-Toddler play interaction in extremely, very low birth weight, and Full-Term children: a longitudinal study. Front Psychol. 2016; 7: 1511.
- 34Célia MG, Stack DM, Serbin LA. Developmental patterns of change in mother and child emotional availability from infancy to the end of the preschool years: a four-wave longitudinal study. Infant Behav Develop. 2018; 52: 76-88.
- 35Korja R, Latva R, Lehtonen L. The effects of preterm birth on mother-infant interaction and attachment during the infant's first two years. Acta Obstet Gynecol Scand. 2012; 91(2): 164-173.
- 36Cappelli M, McGrath PJ, MacDonald NE, Katsanis J, Lascelles M. Parental care and overprotection of children with cystic fibrosis. Br J Med Psychol. 1989; 62(Pt 3): 281-289.
- 37Bornstein MH, Putnick DL, Heslington M, et al. Mother-child emotional availability in ecological perspective: three countries, two regions, two genders. Dev Psychol. 2008; 44(3): 666-680.
- 38Lovas GS. Gender and patterns of emotional availability in mother-toddler and father-toddler dyads. Infant Ment Health J. 2005; 26(4): 327-353.
- 39Stack DM, Serbin LA, Girouard N, et al. The quality of the mother-child relationship in high-risk dyads: application of the Emotional Availability Scales in an intergenerational, longitudinal study. Dev Psychopathol. 2012; 24(1): 93-105.
- 40Cerezo MA, Sierra-García P, Pons-Salvador G, Trenado RM. Parental and infant gender factors in parent-infant interaction: state-space dynamic analysis. Front Psychol. 2017; 8: 1724.
- 41Biringen Z, Robinson JL, Emde RN. Maternal sensitivity in the second year: gender-based relations in the dyadic balance of control. Am J Orthopsychiatry. 1994; 64(1): 78-90.
- 42Engle JM, McElwain NL. Parental reactions to toddlers' negative emotions and child negative emotionality as correlates of problem behavior at the age of three. Social Development. 2011; 20: 251-271.
- 43Eisenberg N, Fabes RA, Shepard SA, Guthrie IK, Murphy BC, Reiser M. Parental reactions to children's negative emotions: longitudinal relations to quality of children's social functioning. Child Dev. 1999; 70(2): 513-534.
- 44Jones S, Eisenberg N, Fabes RA, MacKinnon DP. Parents' reactions to elementary school children's negative emotions: relations to social and emotional functioning at school. Merrill Palmer Q. 2002; 48: 133-159.
- 45Bjorseth A, Wichstrom L. Effectiveness of Parent-Child interaction therapy (PCIT) in the treatment of young children's behavior problems. A randomized controlled study. PLoS One. 2016; 11(9):e0159845.
- 46Thomas R, Abell B, Webb HJ, Avdagic E, Zimmer-Gembeck MJ. Parent-child interaction therapy: a meta-analysis. Pediatrics. 2017; 140(3):e20170352.
- 47Zvara BJ, Sheppard KW, Cox M. Bidirectional effects between parenting sensitivity and child behavior: a cross-lagged analysis across middle childhood and adolescence. J Fam Psychol. 2018; 32(4): 484-495.
- 48Lytton H. Observation studies of Parent-Child interaction: a methodological review. Child Dev. 1971; 42(3): 651-684.
- 49Gardner F. Methodological issues in the direct observation of parent-child interaction: do observational findings reflect the natural behavior of participants? Clin Child Fam Psychol Rev. 2000; 3(3): 185-198.
- 50Atzaba-Poria N, Meiri G, Millikovsky M, Barkai A, Dunaevsky-Idan M, Yerushalmi B. Father-child and mother-child interaction in families with a child feeding disorder: the role of paternal involvement. Infant Ment Health J. 2010; 31(6): 682-698.
- 51Wang X, Cheng Z. Cross-sectional studies. Chest. 2020; 158(1S): S65-S71.
- 52Endendijk JJ, Groeneveld MG, Deković M, van den Boomen C. Short-term test–retest reliability and continuity of emotional availability in parent–child dyads. Int J Behav Dev. 2019; 43(3): 271-277.
- 53Shakiba N, Doron G, Gordon-Hacker A, Egotubov A, Wagner NJ, Gueron-Sela N. Mother-infant emotional availability through the COVID-19 pandemic: examining continuity, stability, and bidirectional associations. Infancy. 2023; 28(1): 34-55.
- 54Sümeyye Koşkulu a b ACK, Berna AU. Maternal behaviors mediate the relationship between socioeconomic status and joint attention. J Appl Dev Psychol. 2021; 75:101291.
- 55Horstman H, Hays A, Maliski R. Parent-child interaction. 2016.