Renal screening sonography—A comparative study in a Portuguese basic emergency service
[Correction added on 10 August 2024, after first online publication: The abstract section has been revised in this version].
Abstract
Introduction
This study intends to compare the accuracy and pertinence of sonographic findings obtained by a sonographer in a Basic Emergency Service (BES) with the imaging findings at the Referral Hospital (RH).
Methods
Thirty-one patients suspected of having renal pathology underwent initial renal sonography screening with sonographer reporting at the BES and were subsequently referred to the RH for additional imaging examinations. The results of both examinations were compared to verify whether the findings from the BES were confirmed by the radiologist in the RH and to ensure that the patient referrals from BES to RH were appropriate.
Results
In our sample, most patients (80%) exhibited varying degrees of pyelocaliceal distension, with nearly half (48%) presenting obstructions. A strong association between the sonographic findings in the BES and the RH was found in the variables “Dilatation of pyelocaliceal system” (V=0.895; p=0.000), “Simple cystic formation” (V=0.878; p=0.000), respectively. There was a statistically significant correlation between BES and RH findings, indicating a strong association between these two variables respectively (k=0.890; p=0.000) and (k=0.870; p=0.000). In this research, an achieved sensitivity of 96% and a specificity of 85% were demonstrated in the identification of pyelocaliceal dilatation.
Conclusion
Renal sonographer reporting screening successfully detected abnormalities in the urinary system of patients suspected of having renal colic. The sonographic data obtained at the BES demonstrated a strong correlation with the additional imaging findings from the RH in Portugal. These results suggest that Radiographers/Sonographers can have an important role in the preliminary assessment of urgent renal pathology in remote areas, contributing to a correct referral and early treatment.
Introduction
Screening sonography has evolved and expanded in the last two decades, boosted by technological evolution, becoming a differentiated diagnostic tool serving multiple specialties in the provision of healthcare. It can be generically categorised into procedural, diagnostic and screening applications, thus demonstrating its versatility and worldwide distribution in clinical practice.1 Screening sonography is particularly valuable for patient screening in emergency departments and is utilised by a diverse group of healthcare professionals, including sonographers.2 The sonographers represent a highly diverse group of ultrasound practitioners who perform diagnostic imaging across a wide range of contexts, including emergency and pre-hospital settings, and within various clinical scenarios.3
Despite its widespread use, the role of sonographers varies significantly both across Europe4 and globally.3 Their responsibilities range from conducting vascular ultrasounds to performing comprehensive scans, which are then interpreted by specialty physicians, as observed in the English and Australian healthcare systems3.5 Unlike these countries where sonography is well-established, Portugal is still in the process of asserting its presence in this area, particularly in emergency settings. Nevertheless, some ultrasound activities and pilot projects are developing in emergency services, particularly in remote or underserved areas.
In this context, renal pathology is recognised as a significant field for screening sonography,6 as evidenced by the consistent use of renal point-of-care ultrasound (POCUS) in emergency department (ED) settings. These features grant the opportunity for sonographers7 and other non-imaging specialists8 to carry out a screening assessment in renal, ureteric and bladder suspicion of abnormalities9 in the context of acute renal colic.
Scientific literature clearly indicates the use of renal POCUS in suspected renal colic,10 and that its early use can lead to fewer days of hospitalisation and episodes in which ED is used in the context of acute kidney disease.11
Renal colic is an extremely frequent clinical situation in the ED,12 generally caused by stones from the upper urinary tract obstructing the flow of urine. Renal colic and nephrolithiasis continue to be a growing health and economic burden in the world13 with high rates of relapse and recurrence to health services.14
Renal POCUS screening is particularly useful in the context of suspected renal colic15 and corresponding differential diagnosis.16 It is also used in the detection of dilatation in the urinary collecting system of the kidney.17 Hydronephrosis18 is one of the main signs of pyelocaliceal or ureteric obstruction and a reliable predictor for additional differentiated care.19
Sonography reporting of renal imaging could hold significant value in Basic Emergency Services (BES) located in peripheral areas, such as the setting of our study. In these contexts, where comprehensive renal function analyses may be lacking and professional and technological limitations are present (no CT or MRI), the importance of having rapidly available provisional renal reporting becomes even more pertinent. The renal screening in this study was executed by a radiographer/sonographer with specific sonography emergency education and training where both radiography (RX) and sonography exams20 are used as complementary diagnostic methods to facilitate the screening process and clinical decision support for the local general practitioner physician.
The purpose of utilising renal sonographic imaging in this context is to assess the presence or absence of abnormalities in the urinary tract that can advise clinical decisions regarding local treatment or the need for referral to a hospital (RH) when appropriate. It is important to note that while renal ultrasound screening provides valuable information, it does not replace comprehensive imaging modalities, which are necessary to confirm suspected findings through the expertise of a radiologist21 and to perform any required differential diagnoses by other clinical specialties.22
Therefore, the primary goal of this study is to assess the detection of pyelocaliceal dilatation in a prehospital setting with sonographer-reported imaging at a BES compared with radiologist imaging findings at the RH in 101 sets of renal images performed.
Methods
Sample and instruments
This cross-sectional study was conducted at a peripheral BES in southern Portugal, incorporating data collected from 2016 through June 2022. Screening sonographic examinations in the BES were carried out using a Toshiba Némio XG ultrasound equipment equipped with a convex probe (3.0–6.0 MHz). Conversely, the ultrasound examinations conducted at the Radiology Department (RH) were performed by radiologists using a General Electric S8 ultrasound system, which featured three distinct probes (linear, convex, and micro-convex). Data analysis was conducted descriptively employing Microsoft Office Excel version 2019, while statistical analysis and correlation tests between variables were performed using IBM SPSS Statistics version 28 software. Ultrasound and other medical images, along with their corresponding reports, were retrieved from the local Picture Archiving and Communication System (PACS) and digital clinical reporting systems.
From an initial sample of 101 renal screening performed on patients presenting with suspected renal colic/flank pain, 31 patients' examinations satisfied the criteria. The inclusion criteria for the study were: (I) Renal colic suspicion/Flank or abdominal pain, (II) clinical suspicion of renal pathology, (III) sonographic image of suspected dilatation of the urinary collecting system of the kidney, (IV) sonographic screening performed in the BES by a radiographer/sonographer, (V) comprehensive sonography and or computed tomography(CT) performed by a radiologist in the RH under about the same complaint and clinical situation regardless of the episode number, (VI) retrieval of sonography images and respective radiologist reports from the PACS and (VII) retrieval of the patient's clinical process.
Statistical analysis
Descriptive statistical analysis, including percentages and frequencies, was conducted for all the variables examined in this study (Table 1). To assess the association between variables, Cramer's V test was employed. Furthermore, to evaluate the inter-rater reliability among the ultrasound findings in the BES and the RH, Cohen's Kappa coefficient was utilised, both with a 95% confidence interval.
| Variables under study | Cramer's V | Significant | Kappa measure of Agreement | Sig |
|---|---|---|---|---|
| Renal Murphy sign, abdominal flank or back pain | 0.682 | 0.001 | 0.466 | 0.000 |
| Bipolar renal measurement below 13 cm | Is a constant | |||
| Dilatation of pyelocaliceal system | 0.895 | 0.000 | 0.890 | 0.000 |
| Renal lithiasis (not obstructive) | 0.743 | 0.000 | 0.736 | 0.000 |
| Location of obstruction by sonography | 0.653 | 0.000 | 0.597 | 0.000 |
| Perirenal fluid | 0.599 | 0.001 | 0.528 | 0.001 |
| Simple cystic formation | 0.878 | 0.000 | 0.870 | 0.000 |
Ultrasound protocols covered in the study
The acquisition of the sonographic images followed a specific and systematic renal protocol to ensure thorough coverage of all urinary tract organs.23 The protocol was adaptable based on the patient's condition/cooperation and the sonographic findings, considering the appearance of any abnormalities during the examination. The ultrasound findings (study variables) or images and the corresponding clinical assessments were considered and documented as in Table 2.
| Category criteria in data evaluation | Option for classification |
|---|---|
| Exam Place | Basic Emergency Service or Referral Hospital |
| Renal Murphy sign, abdominal flank or back pain | Present, absent or doubtful |
| Bipolar renal measurement below 13 cm | Present, absent or doubtful |
| Dilatation of pyelocaliceal system | Present, absent or doubtful |
| Renal lithiasis (not obstructive) | Present, absent or doubtful |
| Location of the obstruction by sonography | Present, absent or doubtful |
| Perirenal fluid | Present, absent or doubtful |
| Simple cystic formation | Present, absent or doubtful |
Although renal ultrasound protocols include several measurements to be performed on the kidney, in this study, we will only consider the bipolar measurement.24 Since renal size can differ considerably depending on various factors such as anthropometric, ethnic and racial diversity,25 this study uses the universal bipolar measure of 13 cm as upper limit length of normality.26 Doppler technique was used in the inspection of suspicion of pyelocaliceal dilatation to avoid pitfalls on false dilatation.27
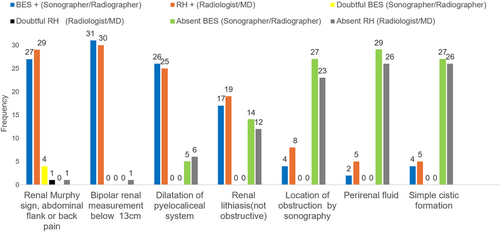
All ultrasound examinations in the BES were conducted by a single radiographer/sonographer, who collected and recorded on a data file built for that purpose. The sonographer performed, analysed, and classified the ultrasound results using the criteria outlined in Figure 1. Together with the BES physician, some patients were referred to the RH for further evaluation. However, due to the lack of connection of the ultrasound equipment with the PACS, it was not possible to send sonographic images from BES to the RH. The only information that the RH radiologists had regarding the initial screening performed at the BES was a brief report written by the BES physician indicating any deviations from normal findings observed during the BES sonographer screening. This limitation exists because the sonographers lack access to the SClinico clinical software, which facilitates information sharing between institutions, and because the ultrasound machines are not integrated with the PACS system.
Ethical approval statement
This study received ethics approval from the Unidade Local de Saúde do Algarve Review Board at Basic Emergency Service on 11-02-2016.
All ultrasound examinations were requested by emergency physicians. Due to the health conditions of some patients, they were unable to provide informed consent. In such cases, consent was obtained from their legal representative. To ensure adherence to the general data protection law, no patient or institutional data were recorded. The primary objective of the study was to showcase the importance and usefulness of sonographic screening in a pre-hospital environment. The study adhered to the ethical standards for scientific research, following the principles outlined in the Declaration of Helsinki and the relevant national data protection legislation.
Results
The final sample size of this study that met the inclusion criteria consisted of 31 patients, with 12 (38.7%) being male and 19 (61.3%) being female. The average age of the patients was 51.7 ± 21.15 years old. Abdominal or thorax radiographs were performed on 19 (61%) of the patients in BES, as well simple urine analysis was acquired in 20 (65%) where alterations were verified in eight patients. RH performed complete blood analyses in all 31patients, where white blood cell count (WBC) was high for 15 (48.4%) of patients, and nine (49%) had abnormal blood urea nitrogen (BUN). Regarding complementary diagnostic exams performed by RH imaging department, was obtained the following distribution: 21 (68%) patients underwent comprehensive sonography (CS) exam, nine (29%) patients performed computed tomography (CT) and US scan, and one patient (3%) performed only CT scan, by decision of the radiologists. The imaging comparative results between BES and RH are summarised in Figure 1 and the respective pathology diagnoses in RH and hospitalisation days are presented in Table 3.
| Patient | Reference Hospital Medical Report (quote) | RH –Hospitalisation Days | Exams under the same pathology RH | Previous attendance to BES For similar reason |
|---|---|---|---|---|
| 1 | ‘Left Ureterohydronephrosis, acute cystitis/Septic shock’ | 12 | Sono + CT | Yes |
| 2 | ‘Patient with urosepsis by obstructive pyelonephritis, admitted to intensive care. Perirenal band of fluid to the right kidney’ | 14 | Sono + CT | Yes |
| 3 | ‘In the right kidney, was observed the presence of moderate pyelocaliceal dilation, with a pelvis in extra-renal topography, measuring approximately 24 mm in AP diameter’ | 0 | Sono + CT | Yes |
| 4 | ‘Pyelocaliceal dilation in relationship with the presence of endoluminal lithiasis in the distal third of the left ureter’ | 0 | Sono | Yes |
| 5 | ‘Patient entered in anasarca, complicated pyelonephritis/Urinary retention/bilateral Ureterohydronephrosis’ | 8 | Sono | Yes |
| 6 | ‘Ureterohydronephrosis on the left, impacted stones in the ureter at the level of the crossing over the iliac vessels’ | 1 | Sono | No |
| 7 | ‘Left Kidney calculus and Slight homolateral pyelocaliceal prominence’ | 0 | Sono | Yes |
| 8 | ‘Urinary difficulty, renal colic, without obstructive signs, discrete pyelocaliceal dilation’ | 0 | Sono | Yes |
| 9 | ‘A slight layer of free fluid between bowel inter-loops and posterior cul-de-sac to be correlated with the clinical and analytical data’ | 1.5 | Sono | No |
| 10 | ‘Ureterohydronephrosis on the right and perirenal fluid slide’ | 1 | Sono | No |
| 11 | ‘Hydronephrosis, with a retroperitoneal mass and calculi in the distal portion of the right ureter’ | 6 | Sono + CT | Yes |
| 12 | ‘Calculus with 6 mm in the right pelvic ureter, conditioning upstream Ureterohydronephrosis’ | 5 | Sono | Yes |
| 13 | ‘Right Ureterohydronephrosis in relation to ureterolithiasis. Small slide of free perirenal fluid on the right’ | 0 | Sono | No |
| 14 | ‘Unilateral Ureterohydronephrosis, bacteremia/septic shock, Bladder neoformation’ | 8 | Sono + CT | Yes |
| 15 | ‘Left Ureterohydronephrosis, observing obstructive lithiasis in the proximal third of the ureter, measuring 8 mm’ | 8 | Sono | Yes |
| 16 | Slight to moderate right pyelocaliceal dilation | 1 | Sono | Yes |
| 17 | ‘Left Ureterohydronephrosis, secondary to obstructive calculus’ | 1.5 | Sono | No |
| 18 | ‘Bilaterally, there are no unequivocal signs of lithiasis or dilatation of the excretory tree’ | 0 | Sono | Yes |
| 19 | ‘Slight hydronephrosis conditioned by calculus, measuring about 4 mm, located in the ureteral meatus’ | 0 | Sono | Yes |
| 20 | Right pyelocaliceal prominence, small right perirenal fluid | 0 | Sono | Yes |
| 21 | ‘Bilateral Ureterohydronephrosis, with no obstructive cause identified’ | 1 | Sono | No |
| 22 | ‘Bladder with voluminous stone formation about 80 mm’ | 2 | Sono + CT | Yes |
| 23 | ‘Marked Right hydronephrosis, conditioned by calculus located in the pyelo-ureteral transition measuring 6 mm’ | 10 | CT | Yes |
| 24 | ‘Left Ureterohydronephrosis, voluminous faecaloma, may be conditioning the ureteral compressive alterations’ | 1 | Sono + CT | Yes |
| 25 | ‘Unremarkable ultrasound exam, it was done for 2 days of pain and traces of haematuria’ | 0 | Sono | Yes |
| 26 | ‘Left hydronephrosis. Signs of apparently non-obstructive ureteral lithiasis are identified on the left’ | 0 | Sono + CT | Yes |
| 27 | ‘Ureterohydronephrosis on the right, with AP diameter of the 18 mm pelvis’ | 1 | Sono + CT | Yes |
| 28 | ‘Normal ultrasound in a Lower Urinary Tract Symptoms setting’ | 3 | Sono | Yes |
| 29 | ‘Prominence of the right pelvis, non-specific, without dilation of the ureter, renal lithiasis in left kidney, non-obstructive’ | 1.5 | Sono | Yes |
| 30 | ‘Right Ureterohydronephrosis, with pelvis measuring approximately 12 mm in diameter AP’ | 0 | Sono | Yes |
| 31 | ‘8 mm obstructive stone at the right proximal ureteral level, responsible for moderate upstream hydronephrosis’ | 0 | CT | Yes |
- BES, Basic emergency Service; CT, Computed Tomography; RH, reference Hospital; Sono, sonography.
For this study, 25 patients (80%) had at least one previous attendance to BES for the same clinical condition. From the patient's observation in RH, there were 19 (61%) patients who needed hospitalisation for further investigation and treatment with an average of 2.7 days of length stay which fits the time intervals described in the available literature, although hospitalisation days can vary greatly.28
There were two patients sent to the RH (6%) that presented normal ultrasound findings, one was sent by persistent pain with high WBC and signs of blood in sample urine simple analyses in the BES, and the second case was a pyelonephritis with unclear sonographic signs which necessitated a 3-day hospitalisation for antibiotic therapy.
Descriptive analysis and interpretation of sonographic findings between BES and RH
The study variables were analysed in terms of BES+/RH+ (%), where (%) = (+RH(100%))/31, as well as percentages on doubtful and absent for RH were calculated based on 31 patients of our final sample. Doubtful and absent ultrasound findings for BES are presented without percentages (one patient had a value of 3.2258% but for simplicity, we designated 3%).
The results (Fig. 1) demonstrated a high degree of concordance in the presence of ‘Renal Murphy sign, abdominal flank or back pain’, with 27 out of 29 patients (94%) being assessed as positive by both BES and RH (Radiologists). Only one patient (3%) did not exhibit positive signs for sonographic renal Murphy according to BES, and one patient (3%) was considered to be absent of this sign by the radiologists. BES had uncertainties in four cases.
In the category of ‘Bipolar renal measurement below 13 cm’, there was a high degree of concordance between observers in 31 out of 30 patients (97%). Only one patient (3%) was identified by radiologists as having a kidney size exceeding 13 cm.
In the category of ‘Dilatation of pyelocaliceal system’, there was a degree of concordance between observers in 26 out of 25 patients (81%). Radiologists determined that six patients (19%) displayed no evidence of pyelocaliceal dilatation. Conversely, the BES (sonographer) identified five patients as lacking pyelocaliceal dilatation.
Concerning the variable ‘Renal lithiasis (not obstructive)’, Concordance was observed in 17 out of 19 positive cases (61%), with a difference of two cases in the analysis. RH (radiologists) determined that 12 patients (39%) exhibited no signs of nephrolithiasis. On the other hand, the sonographer from BES classified 14 patients as showing no signs of nephrolithiasis.
During the evaluation of ‘Location of obstruction by sonography’, it was detected in four out of eight patients (26%). Thus, there was a discrepancy of four patients between professionals in detecting the obstruction site by sonography. Radiologists determined that 23 patients (74%) presented no indications of obstructive signs, while the sonographer from BES identified 27 patients as negative for obstructive signs.
Regarding the presence of ‘Perirenal fluid’, there was consensus in the positive identification among observers in two out of five patients (16%), with a discrepancy of three patients. Radiologists determined that 26 patients (84%) exhibited no evidence of perirenal fluid. Conversely, the sonographer categorised 29 patients as being devoid of perirenal fluid.
In the assessment of ‘Simple cystic formation’ detection, there existed a degree of concordance among observers in four out of five patients (16%), with only one patient showing disparity. Radiologists determined that 26 patients (84%) displayed no indications of cystic structures, whereas the sonographer assessed 27 patients as such.
Discussion
In this study, the primary aim was to assess the detection of pyelocaliceal dilatation in a prehospital setting utilising the sonographer's preliminary report and to compare it with the imaging findings in the RH. Pyelocaliceal dilatation, which typically necessitates a comprehensive investigation, as mentioned earlier, was observed in 84% of the sample population included in this study.
There was one patient in whom the detection of pyelocaliceal dilatation differed between BES and RH. In this particular case, RH classified it as an extra sinus pelvis, whereas BES erroneously interpreted it as pyelocaliceal dilation, a common pitfall among non-specialists.29 However, a follow-up examination was conducted using CT, which suggested the presence of junctional syndrome.30
Due to the limited availability of scientific literature investigating the general comparability of renal sonography conducted by sonographers and radiologists, this study intends to assess and compare the outcomes of renal ultrasound performed in an underserved setting. Specifically, this study examined the agreement in detecting pyelocaliceal dilatation between sonographer reporting from ultrasound images in the BES and the radiologist's reports from ultrasound and CT techniques at the Referral Hospital.
This study demonstrates a sensitivity of 96% and specificity of 85% in the detection of pyelocaliceal dilatation. These values surpass the sensitivity of 75.8% and specificity of 55.2% reported in the study by Abdulaziz et al.31 Furthermore, our findings exhibit superior accuracy compared to the detection of hydronephrosis performed by emergency physicians, with a sensitivity of 72.6% and specificity of 73.3% as reported in the study by Meghan et al.32
When evaluating the sensitivity and specificity results of this study across different categories, specifically, pyelocaliceal dilatation (96%/85%), obstructive lithiasis (66%/85%), and perinephric fluid (65%/100%), we observe similarities with the study results conducted by Bourcier et al,10 which also examined same parameters.
Inferential statistical analysis conducted in this study demonstrated the presence of statistically significant associations between variables related to signs of pyelocaliceal dilation, as confirmed by the calculated Cramer's V and Kappa test values. These significant associations underscore the importance of sonographic findings in renal sonography, particularly in the evaluation of pyelocaliceal dilation, as it could potentially serve as an abnormal parameter that warrants further investigation due to its potential association with complex clinical conditions.
The similarity in results among performers, both sonographers and radiologists, in interpreting findings demonstrates a high degree of concordance (kappa values) in image assessment and analysis at both BES and RH, despite the differences in the imaging methods available between each location. This consistency suggests that the study could be reproducible with similar variables, yielding consistent results.
The findings of this study further highlight the crucial contribution of comprehensive sonography performed by radiologists. Although emergency clinician-performed point-of-care ultrasound (POCUS), BES sonographer reporting, and comprehensive radiology-performed ultrasound serve distinct roles and objectives, this research highlights the critical need for sonographers to possess a deep understanding of renal pitfalls.33 Such knowledge is essential for optimising the effectiveness of renal screening in sonography.
Given the limited availability of radiologists within the Portuguese National Health Service and their frequent overwhelming workload due to high demand from Emergency Departments, the comprehensive ultrasound examination of the kidneys ranks at the top of the list of requested imaging procedures as described by Martins et al.34 Therefore, it should be mandatory to take actions to avoid unnecessary referrals of patients who can be locally managed in BES.
Limitations of the study
The BES ultrasound equipment used in this study exhibited probe limitations and lower image quality and was much older when compared to GE equipment used in the RH. These limitations may stem from factors such as reduced spatial resolution, diminished image quality, or limited depth penetration, which can pose challenges in accurately visualising certain clinical conditions. Furthermore, the lower level of expertise among sonographers compared to radiologists may contribute to discrepancies in the obtained results, especially in the detection of obstruction sites and perirenal fluid. Although higher health schools in Portugal have been providing theoretical and practical education in ultrasonography for many years to radiographers, it does not have the breadth and depth found in the extensive training of radiologists, who undergo a journey of approximately 12 years to obtain their specialisation in all imaging methods.
Moreover, the fact that some patients performed urine simple analyses before the ultrasound exam (empty bladder) may have increased the difficulty in detecting an eventual obstructing stone in the distal ureter.
In our study, we encountered cases of patients with renal pyelocaliceal dilation in which, upon being sent to the RH, opted to discontinue their participation in the national health system. Consequently, it became unfeasible to track their follow-up progress, resulting in a reduction in the representativeness of our sample.
Representative associations and advanced health education institutions could integrate renal BES sonography reporting into institutional protocols for patients with renal colic or suspected urological conditions in similar contexts. Enhancing postgraduate ultrasound programs, offering continuous training, and enacting clearer legislation could increase adherence among radiographers/sonographers in this specialised field, thereby enlarging the sample size of further studies significantly. Such improvements could validate and amplify the benefits observed in this study. However, it is crucial to maintain a cautious interpretation of BES images and ensure that sonographer reporting is followed by appropriate oversight and adheres to the highest quality standards.
Conclusion
BES sonographer reporting, employed as a tool for screening prior to assessment at a referring hospital with more extensive facilities, has shown its efficacy in supporting physician decision-making regarding patient referral and management based on clinical findings in this specific scenario. This study demonstrates a sensitivity of 96% and specificity of 85% in the detection of pyelocaliceal dilatation in the BES. Given the evidence presented in the literature, which highlights the frequent occurrence of recurrent episodes in acute renal pathology leading to multiple visits to emergency services, it would be useful to investigate whether the early utilisation of renal screening from the very first episode of renal colic could potentially decrease the recurrence rate to BES for same causes.
It should be noted that sonography reporting is not intended for making definitive diagnostic determinations. Sonographers can contribute to the screening process without infringing on the work field of other medical specialists, and their involvement has been demonstrated to enhance patient care in certain situations and specific contexts.
Further research involving larger sample sizes and broader geographical coverage is necessary in order to validate and deepen our understanding of this study's findings in similar contexts.
Conflict of Interest
The authors declare no conflict of interest.
Transparency Statement
All authors declares that this manuscript provides an honest, accurate, and transparent account of the study being reported. They confirm that no significant aspects of the study have been omitted and any discrepancies from the planned study (and, if applicable, registered) have been duly explained.
Declaration of Generative AI in scientific language
Generative AI was used to improve the clarity and the grammar issues of some sentences in this article. All the original content and ideas are original and remained that way.
Author Contributions
SM, MDL, RPA: Conceptualisation; data curation; formal analysis; investigation; methodology; resources, supervision; validation; writing – original draft; writing – review and editing. NB, CJ, TF, CG, IR, JM, CH: Review, data curation and validation.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.