Australian medical imaging and world war one
Abstract
Twenty years after the birth of medical imaging from Röntgen's 1895 discovery, military authorities understood the advantage of visualising injuries of wounded soldiers and monitoring their treatment. In World War One, medical imaging equipment was difficult to use and had to be operated in challenging environments. The most common use of x-rays was the imaging of metallic foreign bodies such as bullets and shrapnel lodged within a soldier's body. The need to diagnose, manage war injuries and return soldiers to battle, led to medical imaging innovations including alternate means to record an image, better x-ray tubes and an early form of tomography. Such technological advancements were made by scientists serving their respective countries. With information sourced from the Australian War Memorial archives, this paper also focusses on the experiences of an Australian wartime radiographer. This investigation demonstrates the importance, sacrifice and skills of men and women who took on the difficult task of medical imaging in the first truly world-based conflict. It highlights how a new profession and associated technology emerged as an important tool in military medicine. Importantly, our profession's history within the context of military history should be preserved, while also honouring the legacy of individuals who contributed.
X-ray Imaging and War
X-ray imaging was used in war as early as 1896, just 1 year after Röntgen's discovery. Publications began to appear describing the use of x-rays for examinations of wounded soldiers.1 The first use of wartime x-ray imaging was attributed to the Italian military in the Italian Ethiopian War2 where x-ray installations were located in established military/civilian hospitals or on navy ships. This provided power supply and safety to such fragile equipment.3 Other conflicts that incorporated x-ray imaging were the British army in now modern day Pakistan, the Greco-Turkish War of 1897, the British war in the Sudan 1896–1898 and the Spanish American War of 1898.1 The first significant implementation of x-rays was in the Boer War4, 5 as by this time, x-rays were considered essential to military medicine, especially identifying fractures and foreign objects.6 X-ray machines were standard issue to all Boer War British hospitals.2 Generators were operated by a pedal bicycle or hand powered2, 3, 7 with exposure time described as being ‘short exposures of about four minutes’5 while some exposures were 10–30 minutes.3 Senior Radiologist in the Boer War, Dr John Hall-Edwards, lost his left arm and his right fingers from ionising radiation effects.2 A total of 280 of the British troops were radiologically examined during that conflict.2
The changing nature of WWI warfare was to bring increased complexities in medical treatment. Traditionally, combat consisted of a relatively organised battle sequence which allowed ordered movement of wounded off the battlefield before recommencing.7 This had now changed with the introduction of highly destructive artillery and more accurate and powerful guns. The increased length of fighting made retrieval of soldiers from battle fields more complex and increased the severity of injuries.7, 8 WWI also saw change in how foreign bodies were managed. Unless septic or causing issues due to their location, bullets would often be left in place, whereas shell fragments were quite possibly contaminated and could provide more extensive damage to tissue due to their more varied trajectory. Therefore, these injuries were usually surgically managed.9 Antibiotics had not been available until Fleming's discovery in 1929.10 These foreign objects frequently caused infections, particularly when several days passed before treatment was received off the battle field.11 Prior to x-ray imaging for foreign body localisation, extraction was only possible through high risk exploratory surgery.8 Even with x-ray imaging, it was described that foreign bodies were easily imaged but difficult to exactly locate within the body,12 with the abdomen being the greatest surgical challenge.13 When x-ray imaging was used to locate foreign material, a mark was made on the skin surface and a perpendicular surgical incision made and probe inserted to the suggested depth.14, 15 Errors were common, as the variation in patient position from the x-ray to operating table often rendered measurements inaccurate. This provided a strong impetus to develop a reliable and repeatable technique to accurately locate foreign bodies, with several variations based on trigonometry and triangulation, while others relied on a metallic compass or localisation device similar to modern day stereotaxis.11, 16
The first concepts of tomography were also developed. French military hospitals used a rudimentary system of simultaneously moving the x-ray tube (XRT) and patient to obtain an image of bullets/shrapnel at a certain depth.17 The concept of orthogonal projections was particularly important, as were distortion, penumbra and centring. Surgeons could then gather some confidence with location and depth of fragments.15 The need to identify and surgically remove foreign bodies also resulted in the combined x-ray/operating theatre.12
Military X-ray Departments
Serious medical treatment was kept far from front lines and usually in either established hospitals, repurposed buildings or semipermanent structures called a Stationary Hospital.9, 18 The advantage of these included reliable electricity and running water19 and their own x-ray facilities. Their distance from the front lines was also a disadvantage, which meant soldiers would arrive for treatment days after considerable blood loss and infection onset.7
WWI also saw change to traditional methods of managing war casualties with the introduction of the Casualty Clearing Station (CCS),20 a smaller medical facility just behind the front line and often close to major transport routes such as train lines or roads,20 designed to reduce treatment time and improve medical outcomes.21
Prior to WWI, any mobility in x-ray equipment had been facilitated by a cart drawn by horses, mules or oxen.7 The weight and fragility of x-ray equipment made some journeys difficult or impossible.3 To solve this, allied forces and axis powers worked independently, developing motor vehicle transportation7 (Fig. 1) and thus mobile x-ray units. Using motor vehicles for transporting x-ray units meant it could also supply a power source either directly from its engine or via an electric generator (dynamo) attached to the engine.7 Many temporary hospitals and CCSs did not have power, so the fact that mobile units could supply power to x-ray equipment, lights and surgical instruments, was a significant benefit.7 These motorised units were so highly valued that, to prevent them from falling into enemy hands, standard orders were to destroy them should a retreat be necessary.22 In 1914,23 an Australian version of this self-contained mobile x-ray/surgical unit design was put forward by Ferguson Lemon and advocated twelve staff to operate it, including two photographers, two surgeons, two unqualified assistants, a mechanical engineer, an electrical engineer and four ambulance men for moving the wounded.

X-ray units were also implemented in ships, despite issues of ships pitching and immobilising patients24 with records showing seventy-seven hospital ships in WWI with x-ray units.7 Other mobile units used trains, where carriages were equipped with x-ray units and operating theatres. These could be moved vast distances carrying wounded.7
The X-ray Equipment
XRTs (Fig. 2) were rudimentary and unpredictable, as they needed gases to operate.13 That is, they required gas molecules inside the XRT glass environment rather than the vacuum of modern XRTs.7 Without these gas molecules, the flow of x-ray photons was impeded. With active use, these XRTs became ‘hard’ or resistant to electrical current flow, due to gas molecules adhering to the interior glass surface, cathode and ‘anticathode’ (as the anode was termed then).7 A method to counteract this was to warm the tube with a Bunsen burner, which would release the gas molecules.2, 7 Termed the ‘gas tube era’, these XRTs were unreliable, often gave varying exposures,25 were vulnerable to ambient temperatures and often easily broken.25
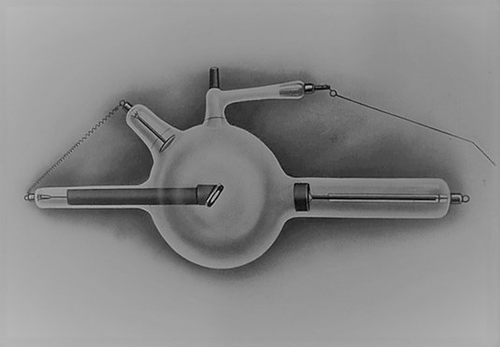
These XRTs needed to be kept in perfect working order with daily maintenance required. A common method of measuring XRT hardness was to use two conductors attached to high voltage supply. Called a Béclère spintermeter, the length of the short circuit spark that emanated between the two conductors was measured. The longer the spark, the more hardening the tube had developed due to increased resistance between the cathode and anticathode.26 Another method was to observe the fluorescence of the XRT when energised. The glass would fluoresce green or blue depending on the composition of the glass. Fluorescence at the frontal hemisphere of the round XRT bulb indicated it was in good working order.26
The XRT that better resembles modern day versions (Coolidge XRT) only became common the United States American Expeditionary Force entered in April 1917. This also applies to the newly invented Potter-Bucky diaphragm.27
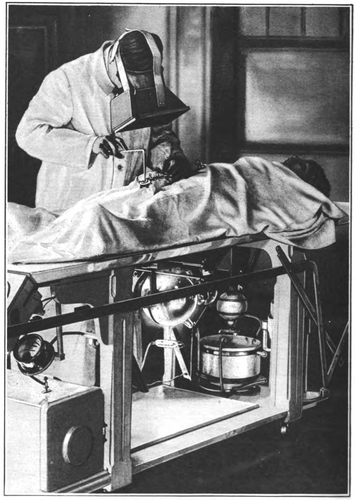
X-ray recording/display medium, as with photography, was still predominantly glass-based plates. X-ray plates used similar emulsion materials to photography but required thicker layers for better direct exposure.28 Apart from being fragile, they were also expensive and prone to poor contrast and optical density.29 The Allies also found that much of the glass used in x-ray imaging plates were made in Belgium, part of the Axis. With supply restrictions, alternatives were sought, with some utilising highly flammable cellulose nitrate film or a paper-based medium.28, 29 Many surgeons used the fluoroscope as a quick and simple means of visualising foreign bodies. These devices were improved in 1916 with calcium tungstate that had a high fluorescence rate, compared the original barium platinocyanide phosphor.7, 29 The issue with this device was that the viewer had their face directly exposed to the x-ray beam (Fig. 3).
During this time, basic radiation protection was known, however, lead-encased XRTs and consistent radiation protection techniques were not common.30 The high volume of x-ray imaging required created an environment where military hierarchy often overlooked the protection of operators.31 Without the concept of cumulative dose being understood, the idea at the time was that operators needed to ‘lose’ the amount of radiation they had received by resting in the country away from radiation sources, returning then to resume its use. Most operators used these dangerous units with a sense of duty to their country and later suffered from their effects. France, Germany and Great Britain had the highest recorded operator deaths resulting from their long and extensive exposure.7 It was these and other radiation-induced injuries that instigated the formation of the X-ray and Radium Protection Committee (IXPRPC) (now the International Commission for Radiation Protection (ICRP)) in 1928.32
Nobel Laureates on Opposing Sides
In 1914, Marie Curie ceased research on radium and ventured into WWI in her adopted France.33, 34 Her major contributions to the war effort were the introduction of mobile x-ray units and the education of x-ray operators. These lorries were equipped with an x-ray machine and a dark room.33 Finance for these came from donations from a philanthropic organisation for women and a wealthy French aristocrat that Curie had lobbied for donations. She finally had a fleet of 18 lorries (Petite Curies)35 or x-ray cars (voiture radiologique1) and recruited women volunteers to provide the service. Both Curie and her daughter Irene, trained approximately 150 women through an x-ray school they established.1, 33 She also operated an x-ray lorry at the front and her experiences helped her further understand the dangers of x-rays. Soldiers not only had to deal with battle injuries but also some had radiation burns. Curie suffered aplastic anaemia later in life, which she attributed to her x-ray exposure during WWI rather than her work with radium and this was partly confirmed by tests on her remains in 1995.35 Her efforts also resulted in 200 hospital-based x-ray rooms, providing over 1 million x-ray examinations throughout WWI33. After WWI, Marie Curie wrote of her experiences in the book La Radiologie et la Guerre.1, 3
At a similar time to Marie Curies' efforts in France, a document titled Aufruf an die Kulturwelt ‘An Appeal to the Civilised World’ was published.36 Better known as ‘the manifesto of ninety-three scholars’,37 it was a set of statements drawn up and signed by prominent German scientists, artists and scholars, aimed to provide rationale for Germany's actions before and during the early stages of WWI. Signatory number 50 was Wilhelm Röentgen, Professor of Physics, Munich. Röentgen's support for the German war effort also extended to him helping raise funds by donating his gold and silver B. Rumford Medal,38 presented to him by the Royal Society in 1896.7 Röentgen was offered a position at Columbia University, New York City, which he initially accepted but after the onset of WWI he decided to stay at Munich University as the Chair of Physics for the rest of his academic life.39 In 1923, Röentgen wrote to a friend stating he was embarrassed when he read the document and indicated he had signed without reading it, at the insistence of Fritz Haber40 a Nobel prize winning chemist and collaborator on the development of chemical (gas) weapons by the German army.41
Suggestions of exploitation of English x-ray technologies were amongst a number of criticisms laid by the Allies towards Germany.42 There was no mention of Röentgen in Allied training manuals when addressing the production of x-rays. Instead, there was acknowledgement of the developer of the Crookes tube, English physicist Sir William Crookes (1891).26 At the time, production of quality XRTs was dominated by Germany and so the war exposed British limitations in this area. For some time, they were restricted to XRTs that could not stand high voltages and strong currents of the exposures necessitated.13 The Allies were even wary of some American technologies which were thought to be the German industry in disguise.26 The solution was finally remedied by France who took up the manufacturing challenge. Post war, a considerable amount of animosity remained between Germany and Allied countries. An example of this is the Röentgen Society (a predecessor to the British Institute of Radiology) contemplated a name change to remove any reference to Röentgen and Germany.43
War Time Radiographers
Across the world, Australia included, radiography was still in its infancy.7 Although education in x-ray imaging for military service began in the UK in 1903,44 there were not enough trained Allied service personnel to operate the required number of x-ray units at the commencement of WWI. Skilled x-ray operators were in demand on the war front which led to shortages in Australia.45 This shortfall necessitated a range of recruits becoming involved in x-ray imaging. Medical doctors, nurses, photographers, engineers or anyone who was free to assist6 often became unskilled operators. This often resulted in mistakes, leaving patients poorly diagnosed and/or with radiation burns.33, 46 It was clear, being placed in the middle of a war zone in a vehicle with little support required more than just novices. Newly enlisted ‘radiographers’ were afforded training, mostly occurring ‘on the job’ while working in the stationary military hospitals. They would soon find themselves working alone or in tandem with a surgeon, once deployed.7 It was a position that required adaptability and ingenuity to meets the needs of tasks required.7
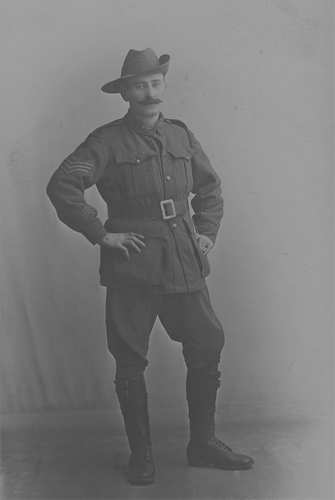
Sergeant William Henry Jones
Sergeant William Henry Jones (Fig. 4) enlisted on 15th of November 1915 at the age of 38 years. A resident of Ryde, Sydney, New South Wales, his occupation prior to enlisting was noted as X-ray Operator;47 however, other records show he was actually a photographer. He had developed these skills after leaving school at 14 years old in Bathurst, New South Wales. At the time, it was not unusual for photographers to be associated with radiography due to the already acquired skills of image development and film processing.28, 48 The length or location of his radiographic practice is not known; however, his younger brother Leslie John Roberts (Jack) Jones had established an x-ray business and also worked at Sydney Hospital.49 With the rank of Sergeant (Sgt.), Jones was assigned to the Second Australian Casualty Clearing Station (2nd ACCS). Just 8 days after enlisting, he departed Melbourne by ship,50 landed in Egypt on 24th of December and travelled to Tel-El-Kebir; the training location for the First Australian Imperial Force reinforcements, No 2 Australian Stationary Hospital.47 The No 2 Australian Stationary Hospital occupied sixty large marquee-tents and accommodated up to 1000 patients after evacuation of the injured from ANZAC peninsula.19 They were specifically located near a railway station to allow the transport of the injured troops from the front.
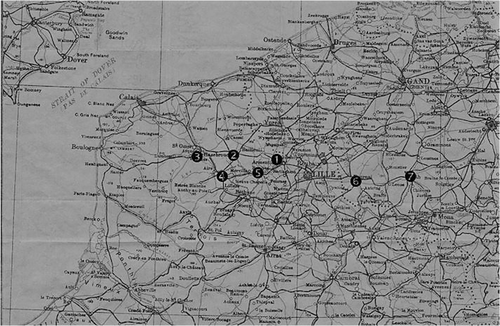
In April 1916, Sgt. Jones was shipped from Alexandria Egypt to Marseilles France where he joined the 2nd ACCS47 at Trois Arbres. As stated, a CCS provided more timely medical care and this was located just behind the front line, far enough to be out of the range of enemy artillery.51 Still, being close to the front, it was not unusual for fighting to affect its activities, with at least two occasions where it was bombed in its first few months.18, 20 Life at the CCS was described as eventful.20 It had three operating tables, two of which functioned 24 h a day. In his first 2 months there were approximately 2000 operations performed.20 Patients were treated from all Allied countries as well as German soldiers.52 As the front lines changed throughout the conflict, so did the CCS location. Sgt. Jones found himself initially at Trois Arbres, then Hazebrouck, Blendeques, St. Venant, Estaires, Tournai and finally Ath20 (Fig. 5).
Although there are no records of what or how many examinations Sgt. Jones was involved in, these can be deduced from accounts of activities undertaken by the 2nd ACCS. Surgical operations from artillery and gunshot wounds were countless and would have had to require him to image to locate shrapnel and/or bullets. Impact wounds would have created fractures and organ injuries that would have necessitated imaging prior and following surgery. Records show injuries ranged from compound fractures, amputations both traumatic and surgical, foreign body removal, head injuries and abdominal wounds. Often there were multiple injuries of these type in one soldier.52 Burst appendices, pneumonia, dysentery and hernia were also treated in clearing stations. Records from July 1917 stated that a number of soldiers were treated for Mustard gas injuries,20, 53 which would have required thoracic imaging. Some conditions rarely heard of today were also documented, for example a ‘soldiers heart’ which is the over exhaustion of the heart due to war time stresses (also known as Da Costas Syndrome or hyperventilation syndrome).13 Its diagnosis and treatment would have been part of a clinical diagnosis and confirmed through thoracic radiographs.
…Pte. Fisher – came in about midnight – 2 am operation for head wounds – died 7 am.
Mr McIntosh – returned to us after leaving a few days ago – wounds head shoulder and leg – seven were having tea in their dugout when shell came over – killed 2 officers.
Johnson – going to operating room – arm to be amputated? – looks very bad.
Long – foot and leg very painful – very bad – had piece of shell removed from bladder – badly wounded poor boy.
Pte. Morris – admitted at 6:30 pm – wounds head, legs, abdomen – taken to operating room – died before anything could be done….
Excerpt from diary of Nurse Bessie Pocock (AANS, RRC)52
The second is an account from one of his patients, Private (Pte) James (Jim) G. Arnott, Scottish born and living near Glasgow. He enlisted into the Yeomen Battery on 23rd of January 1913 where the 17 year old received basic training.54 On the outbreak of the war, he was transferred to the 6th Argyle and Sutherland Highlanders and soon found himself in France in the Battle of the Somme (1st July to 18th November 1916). On the 23rd of September 1916, he was hit by a mortar which shattered both his legs. Lying exposed to the weather and artillery bombardment, he developed hypovolemic shock before being evacuated from the front line. Suffering from contaminated wounds as well as exhaustion and shell shock, he was sent to the 2nd ACCS.54 His wounds would have been assessed clinically and radiographically with images taken by Sgt. Jones. His prognosis was seen as poor. He did not improve and died at approximately 2 pm on the 23rd of September 1916.52
Despite the disturbing scenes and challenging environment, Sgt. Jones remained in active service until the end of WWI. He left emancipated France on the 28th of June 1919 on the ship ‘H.T (Hired Transport) Karoola’.47 In Australia, William did not continue working with x-rays and returned to photography. This may have been a personal preference or due to the challenges of working with x-ray equipment or concerns about the dangers of x-rays on human tissue25, 42, 55-57 from both sides of the conflict.7, 13
There are only a few remaining x-ray plates from the time of Sgt William Jones that are kept in the Australian War Memorial archives. Figure 6 is an image of a forearm with notable shrapnel wounds. Records show that this arm was surgically amputated. It could be suggested that the lack of plates was due to their fragility not surviving the environment in which they were produced. Another suggestion was that the fluoroscope was utilised more frequently for fragment location. Its quick image production reduced the need for processing plates and dark rooms.3, 7, 58

Conclusion
Advancement in technology and science due to the pressures of war were to translate to everyday life.42 By the end of WWI, everything present in major city hospitals was also available in a field hospital in northern France.59 Men and women who provided health care were instrumental in the progression of medical diagnoses and treatments, one of which was diagnostic radiography. They endured difficult situations with challenging and unpredictable equipment in an environment where little expertise existed. WWI affected everybody from an Australian photographer with a small insight into the career of taking x-rays to the most venerated Nobel Prize winners. Our appreciation to these pioneers can be best described by this quote by George W.C. Kaye, a physicist and president of the Röentgen Society.
‘Who will deny the glorious part played by the X-rays in re-establishing shattered and mutilated humanity, and who will withhold an appreciation of the skill and unwearying patience of the radiographer, both medical and layman, whose practised vision detects significant markings which would pass unnoticed by the uninitiated, and whose training and accumulated experience enable him to provide the surgeon with the true interpretation of his wonderful shadow pictures?’ pg713 George W. C. Kaye Physicist and President of the Röetngen Society 1918.




