Evaluation of the circumferential location of mild reflux esophagitis (Grade A and B) in the lower esophagus
Declaration of conflict of interest: The authors have no conflicts of interest to declare.
Financial support: This study was self-funded by the authors.
Abstract
Background and Aim
Discrepancies have been reported in the circumferential locations of mild mucosal breaks. We investigated their locations using a new method.
Methods
This is a retrospective study. Eighty patients (Grade A/B: 53/27) with mild mucosal breaks in the lower esophagus were examined. Since the 3 o'clock position corresponded to the right wall of the lower esophagus using our method with sufficient accuracy, the circumferential locations of mucosal breaks were identified as times on a clock face, which were changed to circular data to calculate the mean direction. The circumferential distribution of mucosal breaks was evaluated in the single lesion group (single group) and multiple lesion group (multiple group).
Results
Forty-eight of 80 patients had 1 mucosal break, while 32 had ≥2 mucosal breaks. Circumferential locations markedly differed between the single and multiple groups. In the single group, mucosal breaks were exclusively distributed between 2 and 7 o'clock, with 50% in the 3 o'clock direction (right wall). In the multiple group, 81 mucosal breaks were distributed circumferentially, not uniformly; however, at least 1 lesion was located between 2 and 7 o'clock in 91% of subjects. Therefore, a factor for the development of mucosal breaks from the right to posterior wall was present in both groups.
Conclusion
In the single group, mucosal breaks were localized from the right to posterior wall, mainly in the right wall. In the multiple group, mucosal breaks were located circumferentially, but often between the right lateral and posterior wall. These two distributions significantly differed.
Clinical trial registration: This is a retrospective study, so it was not registered.
Introduction
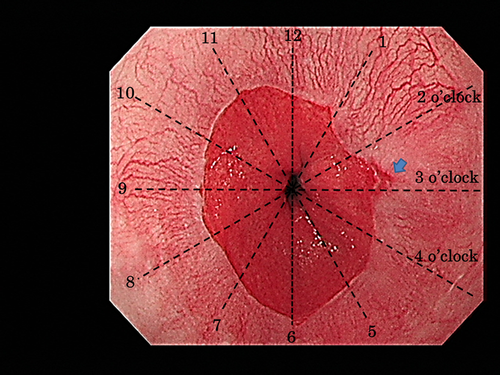
The circumferential location of small lesions in the lower esophagus is generally indicated using a clock face (Fig. 1). Among studies using this representation method, Grade A and B mucosal breaks according to the Los Angeles (LA) classification1 have mainly been detected in two different areas,2, 3 revealing a difference in the angle of approximately 90°. These studies did not describe the method used to confirm that the endoscope was held in the same direction.
We developed a method to manipulate the endoscope by orienting it in the 3 o'clock direction (right lateral wall) from the esophageal hiatus to the lower esophagus along the extension of the center line of the lesser curvature of the stomach.4 Therefore, the circumferential locations of small lesions may be easily detected with sufficient clinical accuracy.
Few studies, except for one,5 have evaluated the characteristics and differences in the circumferential distribution of solitary and multiple mucosal breaks.
The present study was retrospectively conducted to identify the circumferential location of mild mucosal breaks in the lower esophagus using our method, and to clarify the characteristics and differences in the circumferential distribution of single and multiple mucosal breaks.
Materials and methods
Subjects
Eighty subjects with Grade A or B mucosal breaks were selected, excluding those who met the exclusion criteria, from those exhibiting mild reflux esophagitis with mucosal breaks localized in the lower esophagus by routine esophagogastroduodenoscopy (EGD) performed using our new method between April 2015 and January 2017 at Nippon Medical School Hospital. They consisted of 53 LA Grade A and 27 Grade B reflux esophagitis patients.
Exclusion criteria were as follows: patients (i) treated with a proton pump inhibitor or H2 receptor antagonist within 1 month prior to endoscopy, (ii) after gastrointestinal surgery, (iii) with an esophageal hiatus hernia exceeding 2 cm, (iv) with stenosis of the squamocolumnar junction, (v) with a malignant neoplasm of the gastrointestinal tract, or (vi) with a serious disease.
This study was performed according to the ethical principles of the Declaration of Helsinki for medical research involving human subjects. The protocol of the present study was approved by the Ethics Commission of Nippon Medical School (27-11-521). Written informed consent was waived due to the retrospective design of this study.
Methods
Endoscopic procedure
After pharyngeal anesthesia, the endoscope was inserted into the esophagus, mucosal breaks in the lower esophagus were examined during deep inhalation, and findings were recorded. The endoscope was then inserted into the stomach, immediately fixed in a position where the fold of the greater curvature in the upper body of the stomach appeared horizontal (3 o'clock direction) on the monitor screen, and then gradually withdrawn to the lower esophagus while recording images. During this procedure, the 3 o'clock direction was the direction of the right lateral wall of the lower esophagus to the hiatus, that is, the lesser curvature of the stomach.4 When the endoscope was withdrawn from the stomach to the esophagus, the scope was inserted again into the stomach from the esophagus to confirm the horizontal position of the folds of the greater curvature on the monitor.
Since this new method required that the endoscope be kept in a fixed direction, endoscopy was carefully performed by three board-licensed endoscopists of the Japan Gastroenterological Endoscopy Society who had experience in this technique (AY, YH, and KI). Images were acquired using a high-resolution endoscope (GIF-260 and 290; Olympus Co., Tokyo, Japan, and GF-260WR and 280WR; Fujifilm Co., Tokyo, Japan) with the patients throughout in the left lateral position.
Identification of the circumferential location of mucosal breaks
Using the 3 o'clock direction described above, the circumferential locations of mucosal breaks were expressed as 1 to 12 o'clock on a clock face (Fig. 1). In patients with multiple mucosal breaks, the locations of all lesions were shown as times on the clock face. Patients were divided into those with a single lesion and those with ≥2 lesions, and the circumferential distribution of lesions was compared.
To change the time on the clock face to circular data, the 12 o'clock direction was defined as 0°, and each hour was expressed clockwise as an angle and defined as a unit vector directed from the center of the unit circle to each hour on the unit circle. The mean resultant vector [mean direction, mean resultant length] of the circumferential distribution of mucosal breaks was calculated in the single and multiple lesion groups.
Statistical analysis
Statistical analyses were performed using the R statistics program (version 3.4.2 /https://cran.r-project.org). The circumferential distribution of mucosal breaks and the male:female ratio was compared between the single and multiple lesion groups using Fisher's exact test and age distribution using Welch's t-test.
Circular statistical analyses were performed using “circular” and “CircStats,” which are libraries of R. Since frequency distribution by the clock face representation is grouped circular data, we examined whether the time frequency distribution of lesions was uniform using a program modified by the parametric bootstrap method from Watson's U2 statistic used for continuous circular data according to the method of Pewsey et al.6 P < 0.05 was considered to be significant.
Results
Patient characteristics
Among 80 patients with mild reflux esophagitis, 48 had only 1 mucosal break (single lesion group) and 32 had ≥2 breaks (multiple lesion group). The male:female ratio and age of patients in the two groups were 37:11 and 27:5 and 21–85 (mean: 56.3 ± 14.7) and 36–85 (mean: 61.7 ± 13.4) years, respectively. The frequency of Grade B was slightly higher in the multiple lesion group (Table 1). Eighty-one mucosal breaks (A/B: 39/42) were detected in the multiple lesion group (Table 1).
| Grade A and/or B | Single lesion | Multiple lesions | P-value |
|---|---|---|---|
| Case | 48 | 32 | |
| Male:Female | 37/11 | 27/5 | 0.571 |
| Age mean ± SD (years) | 56.3 ± 14.7 | 61.7 ± 13.4 | 0.098 |
| Range | 21–85 | 36–85 | |
| Grade A/Grade B | 36/12 | 17/15 | 0.055 |
| Mucosal break | 48 | 81 | |
| (Grade A/Grade B) | (36/12) | (39/42) | |
| Mean resultant vector [mean direction, mean resultant length] | [111°, 0.79] | [134°, 0.18] |
Circumferential distribution of mucosal breaks in single and multiple lesion groups
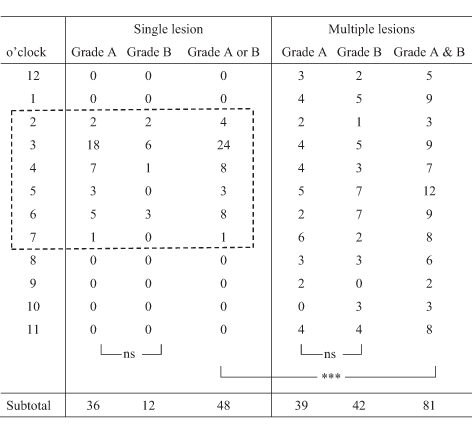
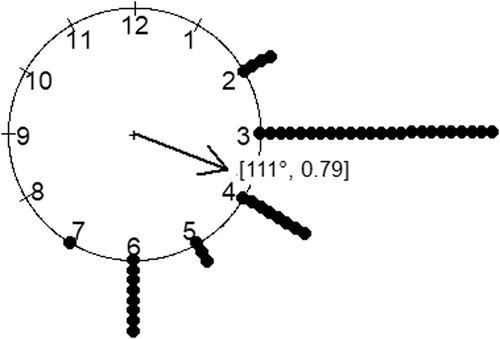
- Mucosal breaks were distributed exclusively between 2 and 7 o'clock in the single lesion group. Mucosal breaks were observed in the 3 o'clock direction (right lateral wall) in 50% of patients (Table 2, Fig. 2).
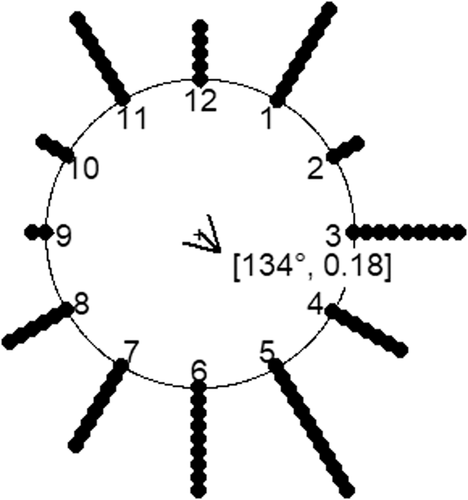
- At least 1 lesion was located between 2 and 7 o'clock in 29 of 32 patients in the multiple lesion group (91%). Eighty-one mucosal breaks were distributed circumferentially, and a uniform distribution was rejected with P < 0.05 by evaluations using circular statistics (Table 2, Fig. 3)
- Circumferential distribution significantly differed (P < 0.001) between the single and multiple lesion groups (Table 2, Figs. 2 and 3).
|
- The broken line indicates that mucosal breaks in patients with a single lesion were localized between 2 and 7 o'clock.
- ***<0.001 (Fisher's exact test).
- ns, not significant (Fisher's exact test).
Evaluation of mean resultant vectors of mucosal breaks in single and multiple lesion groups
-
In the single lesion group, the mean resultant vector was [111°, 0.79] and was located between 3 o'clock (90°) and 4 o'clock (120°) (Table 1, Fig. 2).
-
In the multiple lesion group, the mean resultant vector was [134°, 0.18] and was located between 4 o'clock (120°) and 5 o'clock (150°) (Table 1, Fig. 3).
Discussion
The circumferential locations of Grade A and B mucosal breaks have frequently been detected from the right lateral to anterior wall2 and from the right lateral to the posterior, particularly the posterior wall,3 with a difference of approximately 90°. Those results were different because of the absence of a method to confirm that the endoscope was facing the prescribed direction at the time of judgments. Therefore, the circumferential location of small lesions in the lower esophagus needs to be examined using a method with sufficient clinical accuracy.
In previous studies, all multiple mucosal breaks in the same patient were evaluated, and single and multiple lesions were not assessed separately. Therefore, descriptions of the characteristics and differences in the circumferential distribution of mucosal breaks in patients with a single lesion and those with multiple lesions are insufficient.
In our method to evaluate the circumferential location of small lower esophageal lesions,4 the 3 o'clock direction in the endoscopic view was clarified to fall on the right lateral wall of the lower esophagus (along the extension of the center line of the lesser curvature of the stomach) with sufficient clinical accuracy. This method showed mucosal breaks in the single lesion group from the right lateral to posterior wall and 50% of solitary lesions were distributed in the 3 o'clock direction (Table 2, Fig. 2), suggesting the important role of gastric acid reflux from the lesser curvature in the development of solitary mild mucosal breaks.
Adachi et al.5 retrospectively evaluated a large number of patients with reflux esophagitis and reported that “a large number of esophageal mucosal breaks in the subjects with a single mucosal break was located at 12 to 3 o'clock 0–1 cm from the esophagogastric junction.” Despite a difference of approximately 90° from our results due to a difference in the reference point, solitary lower esophageal mucosal breaks were located within an area of approximately 3 h (90°), similar to the present results. These findings are important when discussing the etiological factors of solitary mucosal breaks.
Similarly, there have been no studies on the circumferential location of mild mucosal breaks in patients with multiple lesions alone, except for the study by Adachi et al.5 They reported that, among the mucosal breaks at 0–1 cm from the esophagogastric junction, a significantly higher percentage of single mucosal breaks were located between the 12 and 3 o'clock directions than multiple mucosal breaks. However, they mainly investigated the relationship between the circumferential distribution of mucosal breaks and the distance from the esophagogastric junction. They simply presented a graph showing the circumferential distribution of mucosal breaks by combining those in the single and multiple lesion groups and did not numerically or graphically show the circumferential distribution of mucosal breaks on a clock face separately in the two groups, resulting in insufficiency of comparison of the circumferential distribution between single and multiple mucosal breaks and evaluation of its clinical significance.
Therefore, their characteristics remain unclear. Among patients with ≥2 mucosal breaks in the present study (Table 2), mucosal breaks were distributed circumferentially (Fig. 3), in contrast to patients with a single mucosal break, suggesting that mucosal breaks are caused by a different mechanism in patients with multiple lesions than in those with a single lesion.
The mean direction in the multiple lesion group was between the right lateral and posterior wall, similar to the single lesion group. In addition, at least one mucosal break was observed between 2 and 7 o'clock in 91% of patients with multiple lesions, and the mechanism that causes mucosal breaks from the right lateral to posterior wall was also considered to have played a major role in many patients with multiple lesions.
The present results are important for evaluating the pathophysiology of the development of Grade A and B mucosal breaks. Many factors have been proposed to contribute to their distribution. For example, an imbalance in the internal pressure of the lower esophagus7, 8 and the direction of acid reflux9-11 have been examined; however, a conclusion has not yet been reached. Ohara et al.11 measured acid reflux at a point 2 cm from the upper margin of the lower esophageal sphincter in healthy individuals, patients with nonerosive reflux disease, and patients with mild reflux esophagitis using an 8-channel pH catheter equipped with 8 antimony pH sensors radially arrayed at the same level, and reported no radial variations of gastric acid reflux in healthy individuals and more acid reflux in the direction of mucosal breaks in many patients with mild reflux esophagitis. However, when the direction of gastric acid reflux in patients with nonerosive reflux disease and those with mild reflux esophagitis was evaluated, gastric acid reflux was predominantly observed on the right side (3 o'clock direction) of the lower esophagus.
Sato et al.12 reported that in resected samples of upper and middle esophageal cancer, a squamous epithelium was located on the stomach side in the central area of the lesser curvature in the esophagogastric junction. The center of the lesser curvature corresponds to the 3 o'clock direction in our method and is the area in which mucosal breaks are concentrated in patients with a single lesion. These findings are of interest for evaluating the etiological factors of mild mucosal breaks, and more detailed examinations of their relationships with the development of mucosal breaks are needed.
This study has several limitations. This was a retrospective study that was performed at a single institute. Furthermore, the number of patients evaluated was small. The numbers of single and multiple mucosal breaks were 48 and 81, respectively. Comparison of the circumferential distribution of mucosal breaks between the single and multiple lesion groups using the R statistics program showed a significant difference (P < 0.001). Since locations in terms of hours were grouped data, the bootstrap method was used to evaluate the uniformity of distribution.6 Therefore, the number of cases needed for analyses (number of lesions, circular data) and the analytical method were appropriate. However, evaluations of a large number of patients by the method developed herein to identify the circumferential location are also needed to clarify the underlying mechanisms and background factors for their development.
Moreover, judgments on the location of each mucosal break on the clock face are subjective to an extent due to the possibility of interobserver errors. The circumferential locations of mucosal breaks in each patient were evaluated by a conference of three researchers (AY, YH, and IK) to reduce biases. Since differences were likely, particularly when the endoscope was withdrawn from the stomach to the esophagus, the scope was inserted again into the stomach from the esophagus to confirm the horizontal position of the folds of the greater curvature on the monitor.
Conclusions
LA Grade A and B mucosal breaks in the lower esophagus were localized from the right lateral to posterior wall in patients with a single lesion, and 50% of lesions were located in the 3 o'clock direction, that is, along the extension of the center line of the gastric lesser curvature. In patients with multiple lesions, mucosal breaks were often located in the middle between the right lateral and posterior wall, but were observed circumferentially. Therefore, in mild reflux esophagitis of the lower esophagus, a mechanism may be causing mucosal breaks from the right lateral to posterior wall, particularly in the right wall; however, other mechanisms are also considered to be involved in patients with multiple lesions.
Acknowledgment
We would like to thank Medical English Service (https://www.med-english.com) for English language editing.
Open Research
Data availability statement
All data generated or analyzed during this study are included in this published article.




