Prevalence of irritable bowel syndrome and functional abdominal pain disorders in children with inflammatory bowel disease in remission
Declaration of conflict of interest: The authors have no conflicts of interest to disclose.
Abstract
Despite evidence of an increased prevalence of irritable bowel syndrome (IBS) in adults with inflammatory bowel disease (IBD) compared with the general population, the prevalence of IBS in children with IBD is unclear. In this review, we aimed to identify the reported prevalence of IBS or functional abdominal pain disorders (FAPDs) in children with IBD in remission. A search of three databases (MEDLINE, Embase, and PubMed) was performed to identify studies reporting the prevalence of IBS or FAPDs in pediatric patients with IBD in remission. A total of 60 studies were identified, with four eligible studies remaining following abstract screening. In children with IBD in remission, the overall prevalence of IBS ranged between 3.9 and 16.1%, and the overall prevalence of FAPDs ranged between 9.6 and 29.5%. The prevalence of FAPDs in patients in biomarker-based remission was generally higher than those in clinical remission (range 16–22.5% vs 9.6–16.7%, respectively). There is a paucity of literature reporting on the prevalence of IBS or FAPDs in children with IBD in remission. Despite the differences in criteria used to define IBD remission in the included articles, there seems to be an increased overall prevalence of IBS or FAPDs in children with IBD.
Introduction
Inflammatory bowel disease (IBD) is a chronic medical condition that manifests primarily as alterations in bowel habit, abdominal pain, and bleeding per rectum.1 In 2017, there was an estimated 6.8 million cases of IBD globally, and the crude prevalence rate of IBD has previously been reported as 24 per 100 000 persons,1, 2 and importantly incidence of both Crohn's disease (CD) and ulcerative colitis (UC) were found to have increased markedly since 1990s.3, 4 The primary goals of treatment in patients with IBD are to achieve remission of disease and limit morbidity and mortality associated with the condition, as well as limitation of adverse effects related to medical and surgical therapy.
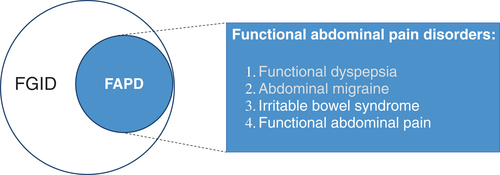
Functional gastrointestinal disorders (FGIDs) are a group of disorders comprising functional abdominal pain disorders (FAPDs), functional nausea and vomiting disorders, and functional defecation disorders.5 These disorders are characterized using the Rome criteria, with the absence of other organic medical conditions as a requirement for diagnosis.5 Studies investigating the worldwide prevalence of FGIDs recently reported that more than 40% of people in the general population experienced symptoms that met the diagnostic criteria for at least one FGID globally,6 and FGIDs were found to affect up to 20–30% children worldwide.7, 8 Figure 1 shows a diagram of FAPDs as a subclassification of FGIDs in children and adolescents, which encompass multiple conditions, including irritable bowel syndrome (IBS), functional abdominal pain, functional dyspepsia, and abdominal migraine.5, 9 A meta-analysis investigating the prevalence of FAPDs in children reported a worldwide pooled prevalence of 13.5%, with IBS comprising the majority of cases with a pooled prevalence of 8.8%.10 Additionally, the same meta-analysis reported a global prevalence of functional abdominal pain of 3.9%.10
Patients with IBD in remission may experience symptoms meeting the diagnostic criteria for IBS or other FAPDs. Fairbrass et al. reported a 32.5% pooled prevalence of IBS in adult patients with IBD in remission based on a systematic review of 27 studies.11 This is in contrast to the global prevalence of IBS in adults, which has been reported as 11%.12 Despite the high prevalence of FGIDs affecting children worldwide, there have been limited studies reporting the prevalence of IBS or FAPDs in pediatric patients with IBD in remission. The aim of this article is to review the current available literature reporting the prevalence of IBS and FAPDs in children with IBD in remission.
Methods
A literature search was conducted in August 2021 to identify primary resources published in the MEDLINE (Ovid) and Embase databases pertaining to the prevalence of FAPDs or IBS in children with IBD. The following search terms were used: IBD, IBS, abdominal pain, FAPD, FGID, prevalence, remission, and children. Case reports, comments, editorials, guidelines, letters, conference abstracts, conference proceedings, and conference reports were all excluded. Results were limited to English language and those including children (age 0–18 years). Additional references were identified following a search of references from relevant articles, as well as an independent search of the PubMed database.
Results
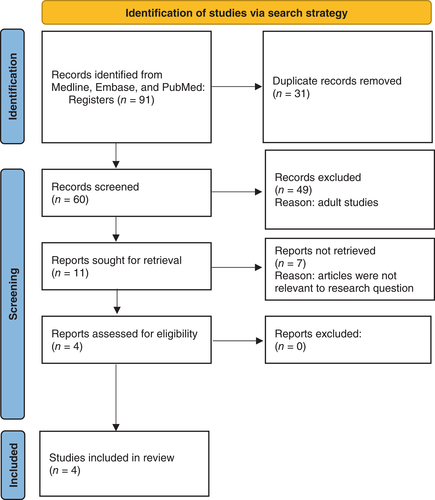
A total of 23 and 46 publications were identified using the MEDLINE and Embase databases, respectively. A search of the PubMed database identified a total of 22 publications. Elimination of duplicates resulted in a total of 60 individual publications identified using the three databases. After exclusion of adult studies and those not relevant to the review, four eligible articles remained (Fig. 2). A search performed without including the term “remission” did not identify any additional articles relevant to the review.
The earliest study investigating the prevalence of FAPDs in pediatric patients with IBD in remission was published by Zimmerman et al. in 2013.13 This study focused specifically on the presence of functional abdominal pain in pediatric patients (aged 9–17 years) with CD in remission. The 174 patients included in the study were subcategorized as being in clinical and/or biomarker-based remission. The authors defined remission of CD in participants of the study by: (i) physician's global assessment, with absence of clinical features (including three or more stools per day, nocturnal stools, bloody diarrhea, recurrent steroid therapy, or strictures or disease flares within the last 6 months); (ii) normal values of biomarkers such as erythrocyte sedimentation rate (ESR) (<10), albumin (>3.5), and C-reactive protein (CRP) (<1.0), (iii) absence of signs of active inflammation on endoscopy; and (iv) no history of clinical relapse within the 6 months prior to the commencement of the study period. Functional abdominal pain was defined as presence of abdominal pain while patients were in remission of CD. Based on these criteria, the authors reported a prevalence of functional abdominal pain of 10.3% in children with CD in remission.
In 2016, Diederen et al. published an article utilizing the Rome III criteria to define the presence of IBS or functional abdominal pain in 184 children with IBD (67% with CD, 33% with UC).14 Rome III criteria for IBS was defined as abdominal discomfort or pain at least once per week for a minimum of 2 months, with the presence of two of the following for at least 2 weeks: (i) improvement with defecation; (ii) onset associated with a change in frequency of stool; or (iii) onset associated with a change in form of stool. Rome III criteria for functional abdominal pain was defined as episodic or continuous abdominal pain at least once per week for a minimum of 2 months, not meeting the criteria for other Rome III diagnoses. This study utilized multiple different definitions of remission. Clinical remission was defined by an abbreviated Pediatric Crohn's Disease Activity Index (aPCDAI) or Pediatric Ulcerative Colitis Activity Index (PUCAI) score of <10. Biochemical remission was defined as a fecal calprotectin <250 μg/g and normal serum CRP. A total of 125 (67.9%) patients met the criteria for clinical remission and 84 (45.6%) met the criteria for biochemical remission. The overall prevalence of IBS in patients meeting the criteria for clinical remission was 6.4% (4.5% in children with CD in remission, 10.8% in children with UC in remission). The prevalence of IBS in patients meeting the criteria for biochemical remission was 16.1% (16.7% in children with CD in remission, 10.8% in children with UC in remission). The prevalence of patients in clinical or biochemical remission who met diagnostic criteria for either IBS or functional abdominal pain was 9.6% (7.9% in children with CD in remission, 13.5% in children with UC in remission), and 22.6% (26.8% in children with CD in remission, 14.3% in children with UC in remission), respectively.
An article by Watson et al. in 2017 similarly aimed to determine the prevalence of FAPDs in pediatric patients with IBD, 71 of whom were in remission.15 Remission of IBD was determined by physician's global assessment, aPCDAI or PUCAI score of <10, as well as normal values of hemoglobin, ESR, albumin, and CRP. A normal fecal calprotectin and/or endoscopy were also used as part of the remission criteria when they were performed. Reference ranges for normal values of pathology tests used in the study were not defined by the authors. Patients were then assessed by patient- or parent-reported Questionnaires on Pediatric Gastrointestinal Symptoms—Rome III version (QPGS-Rome III) to determine the presence of FAPDs. Based on these parameters, the authors found that 21 of 71 patients (29.5%) of children who were in clinical remission of IBD met the criteria for FAPDs (30.9% of children with CD in remission, 25% of children with UC in remission), with 11 of 71 (15.5%) meeting criteria for IBS, 9 (12.7%) for abdominal migraine, and 1 (1.4%) for functional abdominal pain.
The most recent study reporting on the prevalence of FAPDs in children with IBD in remission was published by Tran et al. in 2021.16 A total of 102 patients were recruited based on the study inclusion remission criteria, defined by physician's global assessment and features that include the absence of each of the following: >3 stools/day, blood in stools, nocturnal stools, ongoing steroid therapy, recurrence of disease or optimization of treatment in the last 3 months. Patient- and parent-reported Rome III Diagnostic Questionnaire for the Pediatric Functional Gastrointestinal Disorders (Fr-qPGS) were utilized to diagnose FGIDs, which included FAPDs and other subclassifications of FGIDs. All 102 participants were reported as being in clinical remission (PCDAI or PUCAI score < 10). A total of 79 patients met criteria for biomarker-based remission (CRP < 5 mg/L, ESR < 10 mm/h). Thirty-one patients had abdominal imaging performed, and 28 of them met the criteria for imaging-based remission, which was defined as having no signs of active disease on imaging. Fifteen participants had endoscopy performed, and 11 met the criteria for endoscopic remission (absence of ulcerations and/or CDEIS < 6 in patients with CD; or absence of bleeding, ulceration or erosion, and/or Mayo score ≤ 1 in patients with UC or IBD-U). Ten participants met the criteria for histological remission, which was defined as absence of neutrophils, and normal levels of plasmocytes and eosinophils in the lamina propria. The study reported that 21.5% (22 of 102 participants) of pediatric patients with IBD in remission met the diagnostic criteria for at least one FGID, and 17 (16.7%) met the criteria for at least one FAPD. The reported prevalence of FAPDs in children with IBD, which met the diagnostic criteria for biomarker-based imaging, endoscopic, and histological remission, were 16.4, 14.2, 18.2, and 20%, respectively, and a total of four children (3.9%) met the diagnostic criteria for IBS.
Discussion
This review highlights the limited number of published studies reporting the prevalence of IBS or FAPDs in children with IBD in remission. The four studies included in the review reported a wide prevalence range of IBS in this cohort of children (Table 1). The study published by Zimmerman et al. had the largest cohort size of 174 patients in remission, though all of the patients included had CD.13 The other three studies included patients with either CD or UC, as well as patients with IBD-U in the study by Tran et al.14-16 Overall, the prevalence of IBS in children with IBD in remission ranged between 3.9 and 16.1%, while the prevalence of FAPDs in children with IBD in remission ranged between 9.6 and 29.5%. The prevalence of functional abdominal pain was found to be 10.3% based on the result by Zimmerman et al.13
| Study | Country | Criteria used to define IBS/FAPDs | Type of remission | Remission criteria definition | No. of patients in remission | Prevalence (%) of FAPDs in remission |
|---|---|---|---|---|---|---|
| Zimmerman et al.13 | United States | Presence of abdominal pain despite remission of Crohn's Disease | Clinical/Biomarker-based (n = 307) | Physician's global assessment Clinical features† Normal values of ESR, albumin, CRP No signs of active inflammation when endoscopy was performed (<6 months) |
174 | Functional abdominal pain: 10.3 |
| Diederen et al.14 | Netherlands | Rome III | Clinical (n = 184) | aPCDAI or PUCAI score < 10 | 125 | IBS: 6.4 FAPD: 9.6 |
| Biomarker-based (n = 184) | Serum CRP, fecal calprotectin <250 μg/g | 84 | IBS: 16.1 FAPD: 22.6 |
|||
| Watson et al.15 | United States | Questionnaires on Pediatric Gastrointestinal Symptoms—Rome III version | Clinical/Biomarker-based (n = 128) | Physician's global assessment aPCDAI or PUCAI score < 10 Normal values of Hb, ESR, albumin, CRP Normal fecal calprotectin and/or endoscopy (if performed) |
71 | IBS: 15.5 FAPD: 29.5 |
| Tran et al.16 | France | Rome III Diagnostic Questionnaire for the Pediatric Functional Gastrointestinal Disorders | Study inclusion criteria | Physician's global assessment Clinical features† |
102 | |
| Clinical (n = 102) | PCDAI or PUCAI score < 10 | 102 | IBS: 3.9 FAPD: 16.7 |
|||
| Biomarker-based (n = 102) | Serum CRP <5 mg/L, ESR <10 mm/h | 79 | FAPD: 16.4 | |||
| Imaging (n = 31) | No signs of active disease | 28 | FAPD: 14.2 | |||
| Endoscopic (n = 15) | (CD) No ulcerations and/or CDEIS <6 (UC) No bleeding, ulceration or erosion and/or Mayo score < 1 |
11 | FAPD: 18.2 | |||
| Histological (n = 15) | Absence of neutrophils Normal levels of plasmocytes and eosinophils in lamina propria |
10 | FAPD: 20 |
- † Absence of: three or more stools/day, nocturnal or bloody stools, recurrent steroid therapy, strictures, recurrence of disease or treatment optimization within 3 months prior to the start of the study.
- (a)PCDAI, (abbreviated) Pediatric Crohn's Disease Activity Index; CD, Crohn's disease; CDEIS, Crohn's disease index of severity; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate, albumin; FAPD, functional abdominal pain disorder; FGID, functional gastrointestinal disorder; PUCAI, Pediatric Ulcerative Colitis Activity Index; UC, ulcerative colitis.
The study conducted by Zimmerman et al. utilized less stringent criteria to determine the presence of functional abdominal pain, as opposed to the well-recognized Rome criteria utilized in the other three articles. Two of the reviewed articles did not stratify the remission criteria based on clinical parameters or biomarkers.13, 15 The authors in these articles also used endoscopy result as a part of their remission criteria definition; however, this was not consistently performed, meaning that the definition of remission was not standardized across the study cohort. As a result of this, the authors were not able to report clear prevalence rates based on clinical, biomarker-based, or endoscopic remission criteria for these two studies, which may partly explain the wide range in prevalence rate obtained between the articles.
Due to the heterogeneity between the articles, it was not feasible to determine a pooled prevalence of FAPDs from the studies included. In contrast, the meta-analysis of 27 adult studies published by Fairbrass et al.11 was able to conclude that the prevalence of IBS in patients with IBD in remission is higher than the reported global prevalence of IBS. Data on children and adolescents are still lacking. However, based on the current data, it seems that there is a significant proportion of children with IBD in remission who meet diagnostic criteria for IBS or FAPDs, and this rate seems to be higher than seen in children in the general population.
There have been several proposed mechanisms for the development of IBS or other FAPDs in children with a history of IBD. A meta-analysis conducted by Halpin et al. proposed that low-grade inflammatory processes could lead to altered permeability and sensitization of the visceral afferent neurons, thus resulting in changes to gut motility and visceral sensation.17 Pro-inflammatory cytokines and an altered gut microbiome may contribute to the development of these symptoms in patients despite IBD remission, as observed in post-infectious IBS.5, 18 Psychological distress associated with having a chronic medical condition contributes to symptom generation in these patients.19
Three of the studies included in this review used the Rome criteria to define FAPDs or IBS.20 The most recent version of the Rome criteria, the Rome IV criteria, includes several adjustments compared with previous versions.9 The articles discussed in this review used the Rome III version of the criteria, which has some differences when compared with the latest version (Table 2). Despite some limitations that may occur with the use of the Rome criteria (such as co-existing medical conditions or overlap of multiple FAPDs or FGIDs), there is a need for a standardized diagnostic criteria in clinical setting, and the identification of various FAPD subclassifications, which will help to guide management principles.9, 20 The inclusion of symptoms in various definitions of IBD remission, which may also be consistent with IBS, may be problematic when attempting to delineate active inflammatory disease from functional symptoms.
| IBS | Functional abdominal pain | |
|---|---|---|
| Rome III criteria (established in 2006) |
|
≥1 time/week of all the following:
|
There is no evidence of any inflammatory, anatomic, metabolic, or neoplastic process that may explain the symptoms. Criteria fulfilled for at least 2 months prior to diagnosis. |
||
| Rome IV criteria (established in 2016) |
|
≥4 times/month of all the following:
|
The symptoms cannot be fully explained by another medical condition after appropriate evaluation. Criteria fulfilled for at least 2 months prior to diagnosis. |
||
- † Constipation-predominant IBS.
- FAPD, functional abdominal pain disorder.
The sensitivity and specificity of biochemical parameters to define IBD remission must also be considered. The use of fecal calprotectin should arguably be prioritized over serum-based markers of inflammation, which may not reflect the presence of active inflammation, especially in the setting of distal colitis in patients with UC. The disparity between this small group of studies we have reported highlights the need for a standardized approach to diagnosing FGIDs in patients with a history of IBD, and some adjustments to pre-existing criteria may be warranted to account for this patient group.
By addressing these inconsistencies, we may be able to more accurately define the prevalence of these disorders in this patient cohort. The articles included in this review suggest that up to one in six patients with IBD in remission may meet the criteria for IBS, and up to one in three may meet the criteria for at least one FAPD. Given this, treating physicians should have a high index suspicion for these conditions, and should be wary of escalating treatment based on symptoms that may be functional in origin. Regardless of whether the rates reported are indeed an overestimate of the true prevalence rates, it remains true that a minority of patients with IBD in remission will meet the criteria for IBS or FAPDs, and recognition of this will likely have implications on treatment.
Despite the limitations of this review and the heterogeneity between the articles obtained, the existing literature suggests an overall prevalence of IBS ranging between 3.9 and 16.1%, and an overall prevalence of FAPDs ranging between 9.6 and 29.5% in children with IBD in remission. Despite the wide range in prevalence rates identified by the small number of studies in this review, there is certainly a proportion of children with IBD in remission who would meet the diagnostic criteria for IBS or FAPDs. The heterogeneity we have observed between the articles discussed in this review suggests a need for a standardized guideline for the determination of remission of IBD as well as for the diagnosis of IBS or FAPDs in these patients. Recognition of these conditions is critical to avoid unnecessary escalation of treatment in patients with functional symptoms without other evidence of active IBD. Studies or larger populations using strict criteria for IBD remission are required to determine more accurately the prevalence of FAPDs in this patient group.




