Explant liver evaluation decodes the mystery of cryptogenic cirrhosis!
Abstract
Background and Aim
To determine the concordance of liver explants with the pretransplant diagnosis.
Methods
This was a retrospective analysis of 251 liver explants. Patient information included demography, comorbidity, and etiological diagnosis. Final diagnosis was based on morphological and histological findings. For non-alcoholic steatohepatitis (NASH) and cryptogenic cirrhosis, we investigated comorbid states such as obesity, hypertension, and diabetes. Chi square test and Cohen's Kappa value were used. A P value of <0.05 was considered significant.
Results
A total of 192 patients (76.5%) were males. A significant concordance of explant diagnosis with pretransplant diagnosis was present in 225 (89.6%) patients. It was 100% for alcohol-related disease, hepatitis B, hepatitis C, autoimmune (AI) liver disease, biliary cirrhosis, and Budd–Chiari syndrome. Of 37 patients with a pretransplant diagnosis of cryptogenic cirrhosis, major discordance was observed in 23 (62.1%). On explant, seven patients each had hemochromatosis 5 (13.5%), AI hepatitis, and NASH (18.9%); two had noncirrhotic fibrosis (5.4%); and one each had Wilson's disease and congenital hepatic fibrosis (2.7%). Of the 20 explants, 3 with pretransplant diagnosis of NASH had a diagnosis of cryptogenic cirrhosis on explant specimens. Cohen's Kappa for the concordance of pretransplant diagnosis and explant diagnosis in NASH and cryptogenic cirrhosis patients was 0.75 and 0.47, respectively. An incidental hepatocellular carcinoma was picked up in 16 explants, and 18 had granulomas.
Conclusion
Concordance between pretransplant and explant diagnosis is lower for NASH and cryptogenic cirrhosis. The true prevalence of cryptogenic cirrhosis in our study was 5.6%.
Introduction
Liver transplantation (LT) is currently the treatment of choice for end-stage liver diseases (ESLD), offering a cure to the patient. Explant liver often confirms the pretransplant diagnosis and, at times, provides additional findings not considered prior to transplant. Transplant pathology is integral for a better understanding of the pathogenesis of various liver diseases.1 More importantly, serendipitous findings in the explant specimen can provide a clue to “cryptogenic cirrhosis,” which is essentially a diagnosis of exclusion.
The prevalence of cryptogenic cirrhosis in various series ranges from 5 to 30%.2-4 The diagnosis is largely an exclusion of known causes of liver cirrhosis based on pretransplant etiological work-up, including serological tests and histopathology of liver.
We studied the explant specimens of liver for concordance of explant and pretransplant diagnosis. For specimens with a final diagnosis of non-alcoholic steatohepatitis (NASH) and cryptogenic cirrhosis, a validation was performed for the pretransplant presence of diabetes, hypertension, hypothyroidism and dyslipidemia.
Methods
This was a retrospective analysis of explant liver histology of 251 adult patients with cirrhosis of liver who underwent LT between 2014 and 2016. Patient information included baseline demography and information on comorbid conditions such as diabetes, hypertension, hypothyroidism, dyslipidemia, and etiology of liver disease. The medical records of all patients were carefully reviewed for etiology-based pretransplant diagnosis; comorbid states (hypertension, hypothyroidism, obesity, diabetes mellitus); use of alcohol and drugs; and work-up for metabolic liver disease, viral and autoimmune (AI) markers, and lipid profile. Presence of cirrhosis was based on clinical presentation, imaging studies (computed tomography scan), and presence or absence of varices at endoscopy. The pretransplant diagnosis was based on the sum total of these observations (Table 1).
| Pretransplant diagnosis | Basis for diagnosis |
| HBV related | HBsAg+, total anti-HBc positive with or without detectable viral load |
| HCV related | Anti-HCV + with detectable HCV-RNA |
| Alcohol related | Alcohol intake in cirrhogenic dose (>60 g/day for more than 10–20 years)5, 6 |
| Autoimmune liver disease | ANA/ASMA+, High IgG, liver biopsy suggestive of AIH (wherever possible) |
| NASH |
|
| Cryptogenic | Not fulfilling any of the above criteria |
- AIH, autoimmune hepatitis; ANA, antinuclear antibody; ASMA, antismooth muscle antibody; HBV, hepatitis B, HCV, hepatitis C; NASH, non-alcoholic steatohepatitis.
All explant liver specimens were subjected to special stains for copper and iron, except the hematoxylin and eosin stain. The sites of concentration and location of these elements were noted. In those with a discordant diagnosis, excess copper and iron in liver tissue was correlated with biochemical parameters for Wilson's disease and hemochromatosis. Comorbid states such as diabetes, hypertension, hypothyroidism, and dyslipidemia were particularly scrutinized for explant specimens with a diagnosis of NASH and cryptogenic cirrhosis. Incidental findings, if any, were documented and were reviewed with the pretransplant work-up, and follow-up protocol was instituted.
Exclusion criteria were as follows: patients below the age of 18 years, retransplants, and dual liver kidney transplants.
Statistical Analysis: Age and tumor size were expressed as median and range. Other parameters were expressed as percentage and proportions. The concordance rate was expressed as percentage and evaluated using Cohen's Kappa index value. A comparison of proportions was conducted using the chi square test. A P value of <0.05 was considered statistically significant.
The institutional ethics committee approved this study.
Results
A total of 251 patients underwent LT during the study period—50 deceased donor liver transplantation (DDLT) and 201 living donor liver transplantation (LDLT). Overall, 192 patients (76.5%) were males. The median age was 49.8 years (range 18–64 years). The indication for LT and concordance with the explant diagnosis is shown in Table 2. The concordance with pretransplant diagnosis was 89.6% (225 explants). It was 100% for alcohol-related liver disease, hepatitis B (HBV), hepatitis C (HCV), autoimmune (AI) liver disease, biliary cirrhosis, and Budd–Chiari syndrome.
| Pretransplant diagnosis (n) | Explant diagnosis | Concordance in percentage | Change in diagnosis, n (%) | Incidental HCC, n (%) | Incidental granuloma, n (%) |
|---|---|---|---|---|---|
| Alcohol (82) | 82 | 100 | None | 3 (7.6) | 2(2.4) |
| Hepatitis B (39) | 39 | 100 | None | 3 (7.6) | 1(2.6) |
| Hepatitis C (47) | 47 | 100 | None | 2 (4.2) | 5(10.6) |
| NASH (20) | 17 | 85 | Cryptogenic: 3 (15%) | 4 (20) | 4(20) |
| AI liver disease (16) | 16 | 100 | None | None | None |
| Biliary cirrhosis (8),including Primary biliary cirrhosis (6) and primary sclerosing cholangitis (2) | 8 | 100 | None | None | None |
| BCS (2) | 2 | 100 | None | None | None |
| Cryptogenic (37) | 14 | 37.5 | Hemochromatosis 5 (13.5%) | 4 (10.8) | 6(16.2) |
| AI 7 (19%) | |||||
| WD 1 (2.7%) | |||||
| CHF 1 (2.7%) | |||||
| NCPF 2 (5.4%) | |||||
| NASH 7 (19%) |
- AI, autoimmune; BCS, Budd–Chiari syndrome; CHF, congenital hepatic fibrosis; HCC, hepatocellular carcinoma; NASH, non-alcoholic steatohepatitis; NCPF, noncirrhotic portal fibrosis; WD, Wilson's disease.
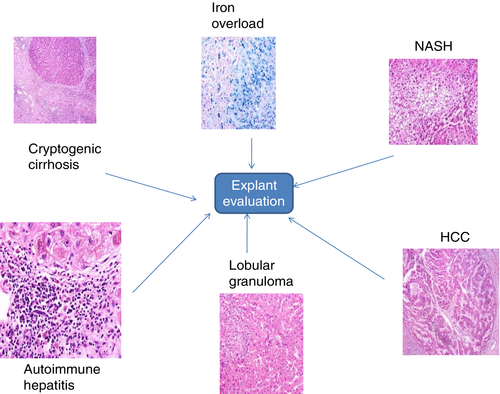
A major discordance was seen in 23 of 37 (62.1%) patients with a pretransplant diagnosis of cryptogenic cirrhosis. On explant, five patients (13.5%) had a definitive diagnosis of hemochromatosis based on site-specific iron distribution and special stain, AI liver disease and NASH in seven each (18.9%), noncirrhotic fibrosis in two (5.4%), and Wilson's disease (based on site-specific copper deposition) and congenital hepatic fibrosis in one each (2.7%) (Fig. 1). HFE gene mutation was negative in all five cases with hemochromatosis. In the patient with Wilson's disease, the pretransplant ceruloplasmin level was 16 mg/dL; Kayser Fischer ring was absent on slit lamp examination, and there was no family history of Wilson's disease. Genetic testing was not performed in this case, and on explant evaluation, the liver copper quantification was 280 mcg/gram of liver tissue. None of the cases with AI liver disease had positive pretransplant serological diagnosis; liver biopsy was also not performed during the pretransplant work-up. On retrospection of patient records, none of the pretransplant diagnoses could be revised. None of the recipients with explant diagnosis of NASH had any of the components of metabolic syndrome (two or more of the following: obesity, hypertension, diabetes, and dyslipidemia).The median body mass index for these patients was 23 kg/m2 (range 19–25) with the presence of ascites, and none of them reported alcohol use.
A mild discordance was seen in patients with a pretransplant diagnosis of NASH (20 patients). Three of the 20 explants had a diagnosis of cryptogenic cirrhosis, possibly burnt out NASH, as all had, in retrospection, two or more components of metabolic syndrome. Cohen's Kappa for concordance of pretransplant and explants diagnosis in NASH and cryptogenic cirrhosis was 0.75 (substantial) and 0.47 (moderate), respectively.
Other findings
A total of 16 explants had an incidental hepatocellular carcinoma (HCC), not identified during liver transplant work-up, 50% each in NASH and cryptogenic cirrhosis. The median size of the tumor was 1.1 cm (0.6–1.8 cm) (Table 2). The alpha fetoprotein was normal, and triple-phase computed tomography was suggestive of dysplastic nodule in eight cases (50%). All the 16 patients are being followed prospectively on protocol-based surveillance.
Eighteen explants had well-defined granulomas. These were seen in 10 explants with cryptogenic or NASH pretransplant diagnosis, in 5 with HCV, in 2 with alcohol-related cirrhosis, and in 1 with a diagnosis of HBV-related cirrhosis. Five patients who had undergone transarterial chemoembolization prior to transplantation had foreign body granuloma. Five patients were diagnosed with caseating granulomas and were started on a four-drug regimen for tuberculosis—isoniazid, rifabutin, pyzinamide, and ethambutol. All responded well to treatment. Three patients with HCV infection showed portal microgranulomas/granulomas. These were compact, nonnecrotizing, epithelioid granulomas of varying sizes observed within portal tracts and lobules. In five cases where the diagnosis of granulomas remained elusive, isoniazid prophylaxis was given for 9 months to reduce the risk of reactivation of tuberculosis.
Discussion
The present study highlights that etiological diagnosis has a perfect concordance with pretransplant diagnosis in nearly three fourths of the cases. The prevalence of “true CC” was 5.6%. NASH was the most common cause of nonalcoholic, nonhepatotropic, virus-related cirrhosis in our patients. Cryptogenic cirrhosis (CC) remains a major clinical challenge for hepatologists. Explant evaluation in such cases is of paramount importance. A study from North India included 84 cases of CC and found non-alcoholic fatty liver disease (NAFLD) as the cause of cirrhosis in 57 patients and noncirrhotic portal fibrosis in 9 patients.7 Another study by the same group assessed pathomorphological features of explants and showed that 63% of CC was NASH related.8 Ayata et al.9 reported that, in a group of 27 patients with pretransplant cryptogenic cirrhosis, the diagnosis remained unresolved in 4 (14.8%) patients. Yet another study reported steatosis (80%) and ballooning (70%), indicative of NASH in 30 CC explants..10
Diagnosis of NASH in clinical setting is primarily circumstantial and associative. In our study, we used the criteria mentioned above to make a diagnosis of NASH in the pretransplant period. Diagnosis of NASH on histopathology remains a challenge as there may be disappearance of fat with progression of NASH—“burnt out NASH.” This may be related to a loss of sinusoidal fenestrations that retard fat deposition in hepatocytes, hepatocyte deprivation of the lipogenic hormones, acinar repopulation by stem cell-derived hepatocytes that are relatively disease resistant, and increased adiponectin levels.11-15
Of CC patients, 12.3% were diagnosed with AI hepatitis. All these patients had a negative autoantibody work-up in the pretransplant evaluation. Autoantibody-negative AI hepatitis is noted in 7% of cases with acute presentations, and 1–34% patients with chronic presentations.16 Use of other new serological markers may help to further diagnose approximately 25% cases of CC.17 Moreover, a few patients present with subacute liver failure with bridging necrosis/collapse, which may demonstrate appearances of cirrhosis on imaging. In our series, one patient had such features.
In our series, five cases had excessive iron deposition on explant evaluation. However, genetic testing for HFE gene mutation was negative in all cases. This excess deposition remains unexplained and could be secondary hemochromatosis. This observation needs further studies for better understanding. One case had excessive copper deposition suggestive of Wilson's disease. The pretransplant ceruloplasmin levels were not very low, and there was no family history of Wilson's disease in family members. A genetic test was not performed for this patient. Two explant livers showed features suggestive of noncirrhotic portal fibrosis (NCPF). A study from North India reported an overlap of clinical features of NCPF and cirrhosis in around 5% of patients with idiopathic portal hypertension.18 NCPF is usually nonprogressive, although a subset of patients is likely proceed to progressive liver failure with the development of ascites and may even require LT.19
Excessive iron and copper deposition in liver explants has been noted in earlier studies as well. Iron overload is common in patients with alcohol-related disease, HCV, and cryptogenic cirrhosis.20 Bilirubinostasis is commonly associated with increased copper deposition and is a frequent observation in pediatric explant specimens. In a recent study,21 the authors surveyed histochemically detectable copper in various liver diseases with an emphasis on chronic biliary disease and venous outflow impairment. Copper was detected in 39% of specimens; all had chronic liver disease. Copper increased with increasing fibrosis. In our study, copper was detected in 43% of specimens. All our patients with Budd–Chiari syndrome and biliary cirrhosis were positive for copper.
Pretransplant assessment of tumor volume based on best available imaging can be inaccurate in nearly 25% of patients.22 Incidentally detected HCC is more common in patients with more advanced liver disease. It has been noted that alfa feto protein is usually not elevated when cumulative tumor size is smaller. Survival of patients with incidental HCC is similar to patients with established HCC. However, recurrence is rare in those with incidentally detected HCC.23 Incidental HCC was more common in those with NASH and cryptogenic cirrhosis. Eight patients with pretransplant diagnosis of NASH and three with explant analysis suggestive of NASH had incidental HCC. Recent data suggest that the prevalence of HCC related to NASH is likely to increase exponentially due to the growing epidemic of obesity and diabetes. In a significant proportion of patients with NAFLD and NASH, HCC can occur even in the absence of cirrhosis. Currently, NASH-related HCC is the most rapidly evolving indication for liver transplant in HCC candidates.24
Eighteen cases had incidentally detected granulomas. Hepatic granulomas are focal aggregates of transformed epithelioid histiocytes with or without multinucleated giant cells that are cuffed by lymphocytes and plasma cells. They represent delayed-type, specialized, cell-mediated immunity and are usually multifactorial. Different antigens like infectious agent, medication, foreign body, and malignancy can initiate granuloma formation. The presence of granulomas suggestive of tuberculosis (TB) in the explant liver is associated with the development of TB in the recipients.25 An earlier study from our center had shown that there was a low prevalence of TB in postliver transplant recipients. Five of our patients with caseating granulomas received antituberculous drugs with dose adjustment of the calcineurin inhibitor level and no untoward adverse effects. In cases where the etiology of the granuloma could not be established, isoniazid prophylaxis was given for 9 months based on institutional protocol. In all these cases, a history of previous tuberculosis, close contact with known tuberculosis, pretransplant chest imaging, and pretransplant interferon gamma assays were taken in to consideration before initiating treatment.
To conclude, extensive morphological and histological evaluation of liver explant specimens is helpful in identifying the underlying etiology of liver cirrhosis. There was 100% correlation between HBV, HCV, alcohol, and Bud–Chiari syndrome as pretransplant diagnoses and the corresponding explants. We noted that concordance between pretransplant and explant diagnosis was lower for NASH and cryptogenic cirrhosis. The true prevalence of cryptogenic cirrhosis in our study was 5.6%.
Acknowledgment
We thank Dr Sruthi Sankar and Mr Tom Michael for providing assistance during the study period and tabulating the data.




