Cervical epidural abscess mimicking crowned dens syndrome
Graphical Abstract
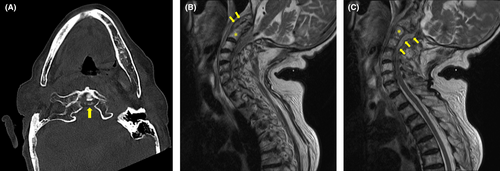
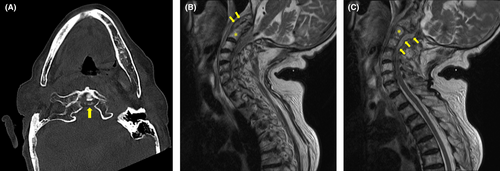
An 88-year-old woman with hypertension and chronic kidney disease presented with pain in her left shoulder and neck that had persisted for 2 days. She had no fever, but her pain was exacerbated by forward bending and rotation of the neck. Plain computed tomography revealed calcification of the atlantoaxial joint (Figure 1A). Therefore, she was diagnosed with crowned dens syndrome (CDS) and was prescribed acetaminophen and no antimicrobials. Five days later, she returned because of a fever and difficulty moving. She was hospitalized, and ceftriaxone was administered. Blood culture was positive for Staphylococcus aureus the day after admission. Cervical magnetic resonance imaging showed an abscess around the odontoid process (Figure 1B) and an epidural abscess in the spinal canal from C1 to Th2 (Figure 1C). Transthoracic echocardiography showed aortic regurgitation and vegetation adhering to the aortic valve (Figure 2). These observations led to the diagnosis of infective endocarditis.
The lumbar level is the predominant site of pyogenic vertebral osteomyelitis and epidural abscesses, whereas the cervical level is less common.1 Even if CDS is diagnosed based on calcification of the atlantoaxial joint, patients should be monitored closely thereafter. Therefore, clinicians should explore alternative diagnoses if the patient fails to respond to treatment for CDS. Repeat imaging studies using different modalities should also be considered because upper cervical spine lesions are difficult to differentiate from CDS,2 as in this case.
AUTHOR CONTRIBUTIONS
Nobumasa Okumura: Conceptualization; writing—original draft preparation; writing—review and editing (lead). Nana Akazawa-Kai: Writing—review and editing (supporting). Naoya Itoh: Funding acquisition; supervision; writing—review and editing (supporting).
FUNDING INFORMATION
This work was supported by the Department of Clinical Infectious Diseases, Nagoya City University Graduate School of Medical Sciences, an endowment department funded by Nagoya City.
CONFLICT OF INTEREST STATEMENT
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
ETHICS STATEMENT
Ethics approval statement: None.
Patient consent statement: Written informed consent was obtained from the patient for publication of this clinical image.
Clinical trial registration: None.