Correlations among noninvasive right ventricular myocardial work indices and the main parameters of systolic and diastolic functions
Jian Wu and Xinyi Huang contributed equally to the study.
Funding information: Science and Technology Planning Project of Xiamen, Grant/Award Numbers: 3502Z20214ZD1166, 3502Z20214ZD2183; Xiamen's Key Project of Medical and Health Sciences, Grant/Award Number: 3502Z20209147
Abstract
Background
Right ventricular (RV) myocardial work (RVMW) is the latest method used to assess RV function. To date, correlations among RVMW indices and RV systolic and diastolic functions have not been studied.
Methods
A total of 106 healthy volunteers (median age, 34 years; 46% male) were prospectively enrolled. RVMW indices were measured using the RV pressure–strain loop using specific software. The correlations among RVMW indices and other RV functions were analyzed.
Results
During the multivariate analysis, the RV global work index (RVGWI) was significantly correlated with RV global longitudinal strain (RV GLS) (p < .0001), pulmonary systolic artery pressure (PASP) (p < .0001), and tricuspid annular (TA) plane systolic excursion (TAPSE) (p = .036). RV global constructive work (RVGCW) was correlated with RV GLS (p < .0001) and PASP (p < .0001). RV global wasted work (RVGWW) was correlated with RV GLS (p = .008) and TA isovolumetric acceleration (TA IVA) (p = .008). RV global work efficiency (RVGWE) was correlated with RV GLS (p < .0001) and tissue Doppler (TD) RV myocardial performance index (TD RMPI) (p = .043).
Conclusion
RVMW indices showed good correlations with RV myocardial systolic function.
1 INTRODUCTION
Recently, the function of the right ventricle has received increasing attention from researchers and clinicians. Compared with the left ventricle, the right ventricle is more affected by afterload.1, 2 The most frequently used methods to analyze right ventricular (RV) function are tricuspid annular (TA) plane systolic excursion (TAPSE), RV fractional area change (RV FAC), and myocardial tissue Doppler (TD) velocities (S′).3-5 However, these parameters do not consider RV afterload and are unable to accurately evaluate RV function. RV longitudinal strain, as an advanced and superior method of evaluating RV function, remains an afterload-dependent parameter.6, 7
RV myocardial work (RVMW) is a novel indicator used to quantitatively analyze RV function.8 RVMW indices are acquired by integrating the RV global longitudinal strain (RV GLS), pulmonary artery pressures, and tricuspid and pulmonic valvular events. Therefore, RVMW can evaluate RV function more precisely than conventional two-dimensional (2D) parameters. We aimed to assess the correlations among RVMW indices and other main parameters of RV systolic and diastolic functions.
2 METHODS
2.1 Study population
A group of 143 healthy volunteers were prospectively recruited from May 2021 to July 2021. The inclusion criteria were as follows: age older than 18 years; body mass index < 30 kg/m2; normal physical examination results; normal electrocardiogram results; normal 2D echocardiography results; and absence of any cardiovascular or respiratory diseases. The Organizational Ethics Committee approved the protocol, and all participants provided informed consent before undergoing the examinations.
2.2 Echocardiographic acquisition
Transthoracic echocardiography was performed using a Vivid E95 scanner (GE Vingmed Ultrasound, Norway) according to the recommended protocols.9, 10 The 2D echocardiography images were acquired using an M5Sc probe, and the four-dimensional (4D) echocardiography RV images were acquired using a 4Vc probe. All electrocardiogram-triggered echocardiography images were obtained over three to five consecutive cardiac cycles during breath holding. Datasets were digitally stored and analyzed offline using EchoPAC v204 (GE Vingmed Ultrasound).
2.3 Echocardiographic measurements
The RV volume and RV ejection fraction were obtained using a software package (4D Auto RVQ). The TAPSE, RV FAC, and RV index of the myocardial performance according to pulsed-wave Doppler (PD) and TD imaging (PD RV myocardial performance index [RMPI] and TD RMPI, respectively) and peak systolic velocity of the tricuspid annulus according to pulsed-wave TD imaging and color TD imaging (TA pulsed-wave TD S′ and TA color TD S′, respectively) were measured according to the current guidelines.5 TA isovolumetric acceleration (TA IVA) was measured by color TD imaging.11 In the RV-focused apical four-chamber view, RV GLS was evaluated by tracing the RV free wall and interventricular septum.10 The tricuspid flow pattern with E and A wave velocities were obtained with the sample volume positioned at the tricuspid leaflet tips. The tricuspid deceleration time was defined as the time from the top point to the end point of the E wave. Isovolumetric relaxation time (IVRT) was measured at the tricuspid lateral annulus using pulsed-wave TD imaging.12 TA velocities according to TD imaging included early and late diastolic annular velocities (E′ and A′, respectively).
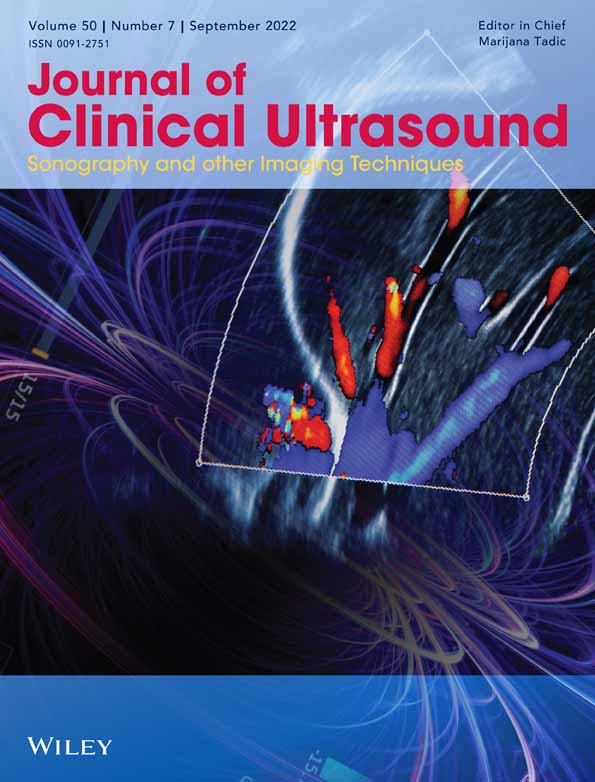
Pulmonary artery systolic pressure (PASP) was computed as follows: PASP = 4 × [tricuspid regurgitation (TR) velocity]2 + mean right atrial (RA) pressure.13 The mean RA pressure was estimated based on the diameter and collapsibility of the inferior vena cava.4 The mean RV–RA gradient was estimated by tracing the TR velocity-time integral (Figure 1A).14 The pulmonary artery mean pressure equals the mean RV–RA gradient plus the mean RA pressure. According to the theoretical formula, pulmonary artery diastolic pressure (PADP) was assessed as follows: PADP = 1.5 × [pulmonary artery mean pressure − (PASP/3)].4 RVMW indices were analyzed using a software package (AFI) designed to assess left ventricular (LV) myocardial work (LVMW). The prognostic validation of LVMW has been performed during several studies.15-17 The tricuspid and pulmonic valve event timings were derived from direct visualization of the parasternal short-axis views (Figure 1B). Then, measurements of RV GLS, PASP, and PADP were synchronized by tricuspid and pulmonic valve event timings to produce a noninvasive RV pressure–strain loop (Figure 1A–D).
- RV global work index (RVGWI): the area of the RV pressure–strain loop, which presents the total RVMW during tricuspid valve closure and tricuspid valve opening.
- RV global constructive work (RVGCW): constructive work during shortening in systole and lengthening during isovolumic relaxation.
- RV global wasted work (RVGWW): waste work during lengthening in systole and shortening during isovolumic relaxation.
- RV global work efficiency (RVGWE): RVGCW / (RVGCW + RVGWW).
2.4 Statistical analysis
The normality of the variables was tested using the Kolmogorov–Smirnov test. Normally distributed variables are expressed as the mean ± SD, and those that were not normally distributed are represented as the median (first quartile, third quartile). Differences between sex groups were analyzed using the two-tailed independent Student's t-test and Mann–Whitney U-test, as appropriate.
Univariate and multivariate linear regression analyzes were performed to examine the independent correlations among the RVMW indices and other RV echocardiographic parameters. Multicollinearity was tested by calculating the variance inflation factors in the multiple linear regression models. The collinear variables included the variables with the highest correlation coefficients.
The intra-observer and inter-observer variabilities of the RVMW were estimated for 20 random subjects using the Bland–Altman analysis. One observer analyzed the same echocardiographic images at two different times to evaluate intra-observer variability. Two independent blinded observers analyzed the echocardiographic images to assess inter-observer variability.
All data were analyzed using SPSS (version 26.0; SPSS Inc., IBM Corp). When p < .05, the difference between variables was considered significant.
3 RESULTS
3.1 Clinical characteristics
During the study, seven subjects were excluded from enrollment because of poor 2D echocardiography images or RV 4D echocardiography images. A total of 30 subjects were excluded because the TR Doppler envelope could not be obtained or the TR Doppler envelopes were of poor quality. Therefore, the feasibility of the RVMW assessment was 74.1% in the study population. The clinical characteristics of the enrolled patients are summarized in Table 1.
| Parameters | Total (n = 106) | Men (n = 49) | Women (n = 57) | p valuea |
|---|---|---|---|---|
| Age (years) | 34 (28, 44) | 33 (29, 42) | 34 (27, 47) | .744 |
| BMI (kg/m2) | 22.0 (20.0, 23.5) | 22.5 (21.7, 24.4) | 20.6 (19.1, 22.7) | <.0001 |
| BSA (m2) | 1.7 ± 0.2 | 1.8 ± 0.1 | 1.6 ± 0.1 | <.0001 |
| SBP (mmHg) | 125 (115, 131) | 130 (118, 132) | 119 (106, 129) | .001 |
| DBP (mmHg) | 74 ± 10 | 75 ± 9 | 73 ± 10 | .187 |
| Heart rate (bpm) | 68 ± 10 | 66 ± 10 | 70 ± 9 | .026 |
| PASP (mmHg) | 21 (19, 24) | 21 (19, 24) | 22 (20, 24) | .321 |
| PAMP (mmHg) | 16 (14, 18) | 15 (14, 18) | 17 (15, 18) | .027 |
| PADP (mmHg) | 13 (12, 15) | 12 (11, 14) | 14 (13, 15) | .001 |
| RVEDV | 94 (85, 104) | 104 (95, 117) | 89 (77, 96) | <.0001 |
| RVESV | 39 (35, 47) | 48 (42, 53) | 36 (32, 39) | <.0001 |
- Abbreviations: BMI, body mass index; BSA, body surface area; DBP, diastolic blood pressure; PADP, pulmonary artery diastolic pressure; PAMP, pulmonary artery mean pressure; PASP, systolic pulmonary artery pressure; RVEDV, right ventricular end-diastolic volume; RVESV, right ventricular end-systolic volume; SBP, systolic blood pressure.
- a p value refers to gender differences.
3.2 Parameters of RV function
Table 2 summarizes the RVMW and RV systolic and diastolic function parameters of the enrolled population. The RVGWI and RVGCW were lower for men (255 mmHg% [215, 332] vs. 291 mmHg% [263, 341]; p = .018 and 316 mmHg% [268, 387] vs. 357 mmHg% [308, 407]; p = .024, respectively), whereas the RVGWW and RVGWE showed no significant differences between sexes.
| Parameters | Total, mean ± SD or median (IQR) | Men, mean ± SD or median (IQR) | Women, mean ± SD or median (IQR) | p valuea |
|---|---|---|---|---|
| RVMW | ||||
| RVGWI (mmHg%) | 286 (233, 337) | 255 (215, 332) | 291 (263, 341) | .018 |
| RVGCW (mmHg%) | 343 (282, 402) | 316 (268, 387) | 357 (308, 407) | .024 |
| RVGWW (mmHg%) | 20 (11, 31) | 20 (12, 31) | 20 (11, 32) | .927 |
| RVGWE (%) | 93 (89, 96) | 93 (90, 96) | 93 (89, 96) | .816 |
| RV systolic and diastolic functions | ||||
| PD RMPI | 0.27 ± 0.07 | 0.27 ± 0.07 | 0.27 ± 0.07 | .999 |
| TD RMPI | 0.42 ± 0.06 | 0.44 ± 0.07 | 0.41 ± 0.06 | .032 |
| RV systolic function | ||||
| TAPSE (mm) | 20 (18, 22) | 20 (18, 22) | 19 (18, 22) | .456 |
| RV FAC (%) | 46 (43, 50) | 44 (41, 47) | 48 (45, 52) | <.0001 |
| 3D RVEF (%) | 58 (55, 59) | 55 (54, 56) | 59 (58, 60) | <.0001 |
| TA PTD S′ (cm/s) | 13 (12, 14) | 13 (12, 14) | 13 (12, 15) | .369 |
| TA CTD S′ (cm/s) | 10 (9, 11) | 10 (9, 11) | 10 (9, 11) | .479 |
| TA IVA (cm/s2) | 3.1 (2.6, 4.1) | 3.1 (2.4, 4.1) | 3.2 (2.7, 4.1) | .347 |
| RV FWLS (%) | −23.4 (−26.0, −21.1) | −23.0 (−26.2, −20.8) | −23.5 (−26.1, −21.4) | .406 |
| RV GLS (%) | −20.0 ± 2.5 | −19.8 ± 2.5 | −20.2 ± 2.4 | .382 |
| RV diastolic function | ||||
| Tricuspid E wave (cm/s) | 55 (48, 63) | 52 (48, 64) | 56 (49, 63) | .319 |
| Tricuspid A wave (cm/s) | 35 (30, 42) | 36 (30, 43) | 35 (30, 41) | .616 |
| Tricuspid E/A ratio | 1.5 (1.3, 1.8) | 1.4 (1.3, 1.7) | 1.6 (1.3, 1.9) | .075 |
| Tricuspid deceleration time (ms) | 167 ± 26 | 166 ± 26 | 167 ± 26 | .947 |
| Tricuspid IVRT (ms) | 51 (44, 58) | 51 (44, 58) | 51 (46, 59) | .405 |
| TA E′ (cm/s) | 14 (12, 17) | 14 (11, 16) | 14 (13, 18) | .061 |
| TA A′ (cm/s) | 13 (11, 15) | 12 (11, 15) | 13 (11, 16) | .676 |
| TA E′ /A′ ratio | 1.1 (0.9, 1.4) | 1.1 (0.8, 1.3) | 1.2 (0.9, 1.6) | .340 |
| E/ E′ ratio | 4.0 ± 1.0 | 4.1 ± 1.0 | 3.9 ± 1.0 | .290 |
- Abbreviations: 3D, three-dimensional; A′, tricuspid lateral annular late diastolic velocity; CTD, color tissue Doppler; E′, tricuspid lateral annular early diastolic velocity; FAC, fractional area changes; FWLS, free wall longitudinal strain; GLS, global longitudinal strain; IQR, interquartile range; IVA, isovolumetric acceleration; IVRT, isovolumetric relaxation time; PD, pulsed-wave Doppler; PTD, pulsed-wave tissue Doppler; RMPI, right ventricular myocardial performance index; RV, right ventricular; RVEF, RV ejection fraction; RVGCW, RV global constructive work; RVGWE, RV global work efficiency; RVGWI, RV global work index; RVGWW, RV global wasted work; RVMW, RV myocardial work; S′, tricuspid lateral annular peak systolic velocity; SD, standard deviation; TA, tricuspid annulus; TAPSE, tricuspid annular plane systolic excursion; TD, tissue Doppler.
- a p value differences between genders.
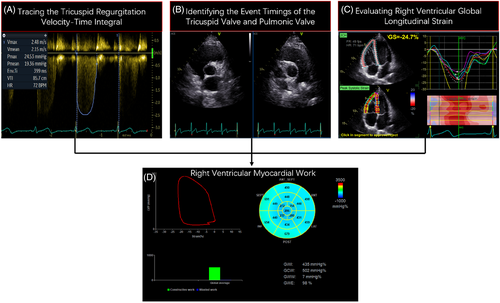
3.3 Correlations among RVGWI and other parameters of RV function
The RVGWI showed good correlation with PASP (r = 0.749; p < .0001), moderate correlations with PADP (r = 0.449; p < .0001), TD RMPI (r = −0.220; p = .024), TAPSE (r = 0.294; p = .002), TA pulsed-wave TD S′ (r = 0.234; p = .016), TA color TD S′ (r = 0.283; p = .003), RV FWLS (r = −0.321; p = .001), RV GLS (r = −0.395; p < .0001), and TA A′ (r = 0.306; p = .001), and weak correlation with TA E′ (Table 3). The multivariate analysis showed that the RVGWI was significantly correlated with PASP (standardized β-coefficient = 0.691; p < .0001), TAPSE (standardized β-coefficient = 0.143; p = .036), and RV GLS (standardized β-coefficient = −0.361; p < .0001) (Table 3 and Figure 2A–C).
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| Coefficient | p value | Standardized β-Coefficient | p value | |
| PASP (mmHg) | 0.749 | <.0001 | 0.691 | <.0001 |
| PADP (mmHg) | 0.449 | <.0001 | ||
| RV systolic and diastolic functions | ||||
| PD RMPI | −0.182 | .061 | ||
| TD RMPI | −0.220 | .024 | ||
| RV systolic function | ||||
| TAPSE (mm) | 0.294 | .002 | 0.143 | .036 |
| RV FAC (%) | 0.082 | .406 | ||
| 3D RVEF (%) | 0.101 | .302 | ||
| TA PTD S′ (cm/s) | 0.234 | .016 | ||
| TA CTD S′ (cm/s) | 0.283 | .003 | ||
| TA IVA (cm/s2) | 0.179 | .067 | ||
| RV FWLS (%) | −0.321 | .001 | ||
| RV GLS (%) | −0.395 | <.0001 | −0.361 | <.0001 |
| RV diastolic function | ||||
| Tricuspid E wave (cm/s) | 0.167 | .087 | ||
| Tricuspid A wave (cm/s) | 0.100 | .305 | ||
| Tricuspid E/A ratio | 0.079 | .424 | ||
| Tricuspid deceleration time (ms) | 0.039 | .692 | ||
| Tricuspid IVRT (ms) | −0.037 | .705 | ||
| TA E′ (cm/s) | 0.195 | .045 | ||
| TA A′ (cm/s) | 0.306 | .001 | ||
| TA E′ /A′ ratio | 0.037 | .710 | ||
| E/ E′ ratio | −0.070 | .477 | ||
- Abbreviations: 3D, three-dimensional; A′, tricuspid lateral annular late diastolic velocity; CTD, color tissue Doppler; E′, tricuspid lateral annular early diastolic velocity; FAC, fractional area change; FWLS, free wall longitudinal strain; GLS, global longitudinal strain; IQR, interquartile range; IVA, isovolumetric acceleration; IVRT, isovolumetric relaxation time; PADP, pulmonary artery diastolic pressure; PASP, pulmonary artery systolic pressure; PD, pulsed-wave Doppler; PTD, pulsed-wave tissue Doppler; RMPI, right ventricular index of myocardial performance; RV, right ventricular; RVEF, RV ejection fraction; RVGCW, RV global constructive work; RVGWE, RV global work efficiency; RVGWI, RV global work index; RVGWW, RV global wasted work; RVMW, RV myocardial work; S′, tricuspid lateral annular peak systolic velocity; SD, standard deviation; TA, tricuspid annular; TAPSE, tricuspid annular plane systolic excursion; TD, tissue Doppler.
3.4 Correlations among RVGCW and other parameters of RV function
The RVGCW showed good correlations with PASP (r = 0.810; p < .0001) and PADP (r = 0.541; p < .0001) and moderate correlations with TAPSE (r = 0.275; p = .004), TA pulsed-wave TD S′ (r = 0.230; p = .018), TA color TD S′ (r = 0.248; p = .010), TA IVA (r = 0.288; p = .003), RV FWLS (r = −0.308; p = .001), RV GLS (r = −0.330; p = .001), and TA A′ (r = 0.349; p < .0001) (Table 4). The multivariate analysis showed that the RVGWI was significantly correlated with PASP (standardized β-coefficient = 0.716; p < .0001) and RV GLS (standardized β-coefficient = −0.279; p < .0001) (Table 4 and Figure 2D,E).
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| Coefficient | p value | Standardized β-Coefficient | p value | |
| PASP (mmHg) | 0.810 | <.0001 | 0.716 | <.0001 |
| PADP (mmHg) | 0.541 | <.0001 | ||
| RV systolic and diastolic functions | ||||
| PD RMPI | −0.078 | .425 | ||
| TD RMPI | −0.159 | .104 | ||
| RV systolic function | ||||
| TAPSE (mm) | 0.275 | .004 | ||
| RV FAC (%) | 0.158 | .105 | ||
| 3D RVEF (%) | 0.096 | .329 | ||
| TA PTD S′ (cm/s) | 0.230 | .018 | ||
| TA CTD S′ (cm/s) | 0.248 | .010 | ||
| TA IVA (cm/s2) | 0.288 | .003 | ||
| RV FWLS (%) | −0.308 | .001 | ||
| RV GLS (%) | −0.330 | .001 | −0.279 | <.0001 |
| RV diastolic function | ||||
| Tricuspid E wave (cm/s) | 0.139 | .154 | ||
| Tricuspid A wave (cm/s) | 0.084 | .390 | ||
| Tricuspid E/A ratio | 0.056 | .568 | ||
| Tricuspid deceleration time (ms) | 0.055 | .575 | ||
| Tricuspid IVRT (ms) | −0.003 | .977 | ||
| TA E′ (cm/s) | 0.165 | .092 | ||
| TA A′ (cm/s) | 0.349 | <.0001 | ||
| TA E′ /A′ ratio | −0.087 | .378 | ||
| E/ E′ ratio | −0.063 | .521 | ||
- Abbreviations: 3D, three-dimensional; A′, tricuspid lateral annular late diastolic velocity; CTD, color tissue Doppler; E′, tricuspid lateral annular early diastolic velocity; FAC, fractional area change; FWLS, free wall longitudinal strain; GLS, global longitudinal strain; IQR, interquartile range; IVA, isovolumetric acceleration; IVRT, isovolumetric relaxation time; PADP, pulmonary artery diastolic pressure; PASP, pulmonary artery systolic pressure; PD, pulsed-wave Doppler; PTD, pulsed-wave tissue Doppler; RMPI, right ventricular index of myocardial performance; RV, right ventricular; RVEF, RV ejection fraction; RVGCW, RV global constructive work; RVGWE, RV global work efficiency; RVGWI, RV global work index; RVGWW, RV global wasted work; RVMW, RV myocardial work; S′, tricuspid lateral annular peak systolic velocity; SD, standard deviation; TA, tricuspid annular; TAPSE, tricuspid annular plane systolic excursion; TD, tissue Doppler.
3.5 Correlations among RVGWW and other parameters of RV function
The RVGCW showed moderate correlations with PADP (r = 0.214; p = .028), PD RMPI (r = 0.297; p = .002), TA IVA (r = 0.257; p = .008), and RV GLS (r = 0.247; p = .011; Table 5). The multivariate analysis showed that the RVGWI was significantly correlated with TA IVA (standardized β-coefficient = 0.279; p = .008) and RV GLS (standardized β-coefficient = 0.306; p = .008; Table 5 and Figure 2F,G).
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| Coefficient | p value | Standardized β-Coefficient | p value | |
| PASP (mmHg) | 0.191 | .050 | ||
| PADP (mmHg) | 0.214 | .028 | ||
| RV systolic and diastolic functions | ||||
| PD RMPI | 0.297 | .002 | ||
| TD RMPI | 0.129 | .187 | ||
| RV systolic function | ||||
| TAPSE (mm) | 0.007 | .939 | ||
| RV FAC (%) | 0.167 | .087 | ||
| 3D RVEF (%) | 0.051 | .606 | ||
| TA PTD S′ (cm/s) | −0.014 | .887 | ||
| TA CTD S′ (cm/s) | −0.044 | .655 | ||
| TA IVA (cm/s2) | 0.257 | .008 | 0.279 | .008 |
| RV FWLS (%) | 0.050 | .607 | ||
| RV GLS (%) | 0.247 | .011 | 0.306 | .008 |
| RV diastolic function | ||||
| Tricuspid E wave (cm/s) | −0.016 | .868 | ||
| Tricuspid A wave (cm/s) | −0.007 | .943 | ||
| Tricuspid E/A ratio | −0.038 | .700 | ||
| Tricuspid deceleration time (ms) | 0.113 | .249 | ||
| Tricuspid IVRT (ms) | 0.161 | .099 | ||
| TA E′ (cm/s) | −0.059 | .545 | ||
| TA A′ (cm/s) | 0.165 | .090 | ||
| TA E′ /A' ratio | −0.158 | .107 | ||
| E/ E′ ratio | 0.054 | .585 | ||
- Abbreviations: 3D, three-dimensional; A′, tricuspid lateral annular late diastolic velocity; CTD, color tissue Doppler; E′, tricuspid lateral annular early diastolic velocity; FAC, fractional area change; FWLS, free wall longitudinal strain; GLS, global longitudinal strain; IQR, interquartile range; IVA, isovolumetric acceleration; IVRT, isovolumetric relaxation time; PADP, pulmonary artery diastolic pressure; PASP, pulmonary artery systolic pressure; PD, pulsed-wave Doppler; PTD, pulsed-wave tissue Doppler; RMPI, right ventricular index of myocardial performance; RV, right ventricular; RVEF, RV ejection fraction; RVGCW, RV global constructive work; RVGWE, RV global work efficiency; RVGWI, RV global work index; RVGWW, RV global wasted work; RVMW, RV myocardial work; S′, tricuspid lateral annular peak systolic velocity; SD, standard deviation; TA, tricuspid annular; TAPSE, tricuspid annular plane systolic excursion; TD, tissue Doppler.
3.6 Correlations among RVGWE and other parameters of RV function
The RVGCW showed moderate correlations with PD RMPI (r = −0.62; p = .007), TD RMPI (r = −0.234; p = .016), RV GLS (r = −0.394; p < .0001), and tricuspid IVRT (r = −0.200; p = .040; Table 6). The multivariate analysis showed that the RVGWI was significantly correlated with TD RMPI (standardized β-coefficient = −0.232; p = .043) and RV GLS (standardized β-coefficient = −0.471; p < .0001; Table 6 and Figure 2H).
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| Coefficient | p value | Standardized β-Coefficient | p value | |
| PASP (mmHg) | 0.099 | .314 | ||
| PADP (mmHg) | 0.028 | .775 | ||
| RV systolic and diastolic functions | ||||
| PD RMPI | −0.262 | .007 | ||
| TD RMPI | −0.234 | .016 | −0.232 | .043 |
| RV systolic function | ||||
| TAPSE (mm) | 0.050 | .612 | ||
| RV FAC (%) | −0.132 | .179 | ||
| 3D RVEF (%) | −0.035 | .725 | ||
| TA PTD S′ (cm/s) | 0.062 | .526 | ||
| TA CTD S′ (cm/s) | 0.137 | .162 | ||
| TA IVA (cm/s2) | −0.054 | .581 | ||
| RV FWLS (%) | −0.127 | .193 | ||
| RV GLS (%) | −0.394 | <.0001 | −0.471 | <.0001 |
| RV diastolic function | ||||
| Tricuspid E wave (cm/s) | 0.015 | .875 | ||
| Tricuspid A wave (cm/s) | −0.004 | .970 | ||
| Tricuspid E/A ratio | 0.042 | .667 | ||
| Tricuspid deceleration time (ms) | −0.124 | .204 | ||
| Tricuspid IVRT (ms) | −0.200 | .040 | ||
| TA E′ (cm/s) | 0.011 | .912 | ||
| TA A′ (cm/s) | −0.082 | .401 | ||
| TA E′ /A′ ratio | 0.079 | .419 | ||
| E/ E′ ratio | −0.014 | .889 | ||
- Abbreviations: 3D, three-dimensional; A′, tricuspid lateral annular late diastolic velocity; CTD, color tissue Doppler; E′, tricuspid lateral annular early diastolic velocity; FAC, fractional area change; FWLS, free wall longitudinal strain; GLS, global longitudinal strain; IQR, interquartile range; IVA, isovolumetric acceleration; IVRT, isovolumetric relaxation time; PADP, pulmonary artery diastolic pressure; PASP, pulmonary artery systolic pressure; PD, pulsed-wave Doppler; PTD, pulsed-wave tissue Doppler; RMPI, right ventricular index of myocardial performance; RV, right ventricular; RVEF, RV ejection fraction; RVGCW, RV global constructive work; RVGWE, RV global work efficiency; RVGWI, RV global work index; RVGWW, RV global wasted work; RVMW, RV myocardial work; S′, tricuspid lateral annular peak systolic velocity; SD, standard deviation; TA, tricuspid annular; TAPSE, tricuspid annular plane systolic excursion; TD, tissue Doppler.
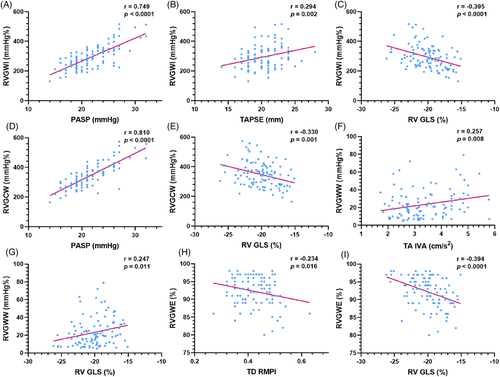
3.7 Inter-observer and Intra-observer variabilities
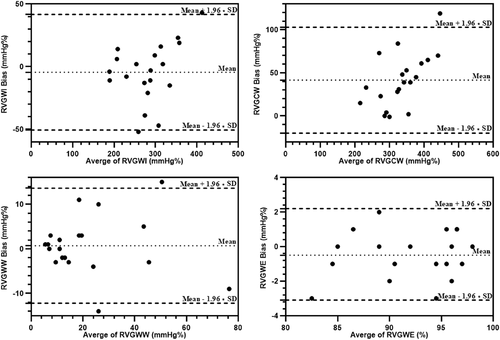
The intra-observer and inter-observer variabilities of the RVMW parameters are summarized in Table 7, Figures 3 and 4. Good intra-observer reproducibility and inter-observer reproducibility were indicated.
| Intra-observer variability | inter-observer variability | |||||
|---|---|---|---|---|---|---|
| Bias | 95% CI | ICC | Bias | 95% CI | ICC | |
| RVGWI (mmHg%) | −6.700 | −53.2; 39.9 | 0.940 | −4.500 | −50.6; 41.6 | 0.920 |
| RVGCW (mmHg%) | 0.900 | −53.8; 55.3 | 0.960 | 41.600 | −19.9; 103 | 0.920 |
| RVGWW (mmHg%) | 0.400 | −8.3; 9.1 | 0.920 | 0.700 | −12.2; 13.6 | 0.940 |
| RVGWE (%) | −0.200 | −2.9; 2.6 | 0.860 | −0.450 | −3.1; 2.2 | 0.960 |
- Abbreviations: CI, confidence interval; ICC, intraclass correlation coefficient; RV, right ventricular; RVGCW, RV global constructive work; RVGWE, RV global work efficiency; RVGWI, RV global work index; RVGWW, RV global wasted work.
4 DISCUSSION
The RVMW, derived from the pressure-strain loop, was first introduced by Butcher et al.8 as a method to assess RV function. The study showed that RVMW indices were good parameters for comparing the RV function of the healthy control group and patients with reduced LV ejection fraction. All RVMW indices were significantly correlated with the RV GLS. Moreover, RVGCW was moderately correlated with the invasive RV stroke volume. Hence, because of the growing interest in RVMW, we aimed to assess the correlations among RVMW indices and other parameters of RV systolic and diastolic functions.
In our cohort, the RVGWI, RVGCW, RV FAC, and three-dimensional RV ejection fraction were significantly lower in men than in women. This may be evidence that women have more dynamic RV systolic function than men.18 The univariate analysis showed that both the RVGWI and RVGCW significantly increased according to the PASP and PADP. However, the multivariate analysis revealed that the RVGWI and RVGCW were not significantly correlated with the PADP. The analysis showed that the RVGWW and RVGWE were not correlated with the PASP. Therefore, we speculated that the PASP only affects the RVGWI and RVGCW, and that the RVGWW and RVGWE do not change according to the PASP in the healthy population.
PD RMPI and TD RMPI are powerful and independent prognostic indicators used to analyze RV global systolic and diastolic functions.19-21 During our study, the univariate analysis showed that the PD RMPI was significantly associated with the RVGWW and RVGWE, and that the TD RMPI was significantly associated with the RVGWI and RVGWE, thus implying that higher values of PD RMPI and TD RMPI could be translated to lower RVGWI and higher RVGWW, thereby leading to a lower RVGWE. However, only TD RMPI was significantly correlated with RVGWE in the multivariate analysis.
Regarding RV systolic function, both univariate and multivariate analyses revealed that RVMW indices were significantly correlated with RV GLS. As is well known, RV longitudinal strain, derived by speckle tracking echocardiography, is less load-dependent and angle-dependent than conventional RV function indices.22 As a reproducible and sensitive index that is widely used in clinical work and research,5, 23-26 RVMW integrates RV GLS; however, other influences may reflect RV systolic function more sensitively and precisely than RV GLS. In general, the RVGWI and RVGWE could reflect RV positive mechanics and performance, similar to other parameters of RV systolic function. Our study demonstrated that the RVGWI and RVGCW were significantly correlated with RV FWLS, TAPSE, TA pulsed-wave TD S′, and TA color TD S′ in the univariate analysis. Moreover, the TA IVA is not affected by changes in preload and/or afterload and is a reliable indicator of changes in RV systolic function in clinical trials.27 During our study, both RVGCW and RVGWW were significantly correlated with the TA IVA in the univariate analysis, possibly implying that a higher TA IVA represents a higher value of the RV contribution and waste work.
Among RV diastolic functions, the univariate analysis showed that the RVMW indices correlated with the TA E′ and A′, the RVGCW correlated with the TA A′, and the RVGWE correlated with the tricuspid IVRT. However, the multivariate analysis showed that RV diastolic function parameters were not significantly associated with RVMW indices. Based on our data, RVMW indices showed weak correlations with RV diastolic function parameters. This result may be because the RVMW is derived from the RV GLS, which mainly reflects RV systolic function. Another possible explanation is that the inclusion of healthy subjects resulted in a limited range of RV diastolic function values.
Our data support RVMW indices as reliable parameters of myocardial systolic performance. Notably, the data showed excellent agreement and repeatability when assessing the RVMW indices. As a noninvasive and convenient technique, the RVMW provides a scientific basis and further information for assessing the RV function. Butcher et al.8 demonstrated that the RVGWI, RVGCW, and RVGWE of patients with heart failure decreased, and that the RVGWW increased compared to a healthy control group. Additionally, because the RV myocardial work takes into account the pulmonary pressure, it will be an excellent indicator for evaluating the RV systolic function of patients with pulmonary hypertension. Moreover, for patients with arrhythmia, congenital heart disease, and cardiomyopathy (hypertrophic cardiomyopathy, dilated cardiomyopathy, myocardial amyloidosis, and others), the RVMW changes in varying degrees. Therefore, the RVMW can be used for risk stratification of the aforementioned diseases and for the evaluation of treatment effects.
4.1 Study limitations
Acquiring and quantifying RVMW datasets using a single-provider platform may affect the applicability of these reference values to data obtained from other provider platforms. Additionally, the commercial software required to measure the RVMW is specifically designed to measure the LVMW. The RV afterload may have been inaccurate because it was estimated by calculating the pulmonary pressure rather than by performing direct measurements. Therefore, the calculation of the RVMW is not as precise as that of the LVMW because of the complicated and irregular RV anatomy and shape.28, 29 The noninvasive RV pressure–strain loop may need to be validated by the invasively derived RV pressure–strain loop in the future. Moreover, for ethical reasons, cardiac magnetic resonance and right heart catheterization were not performed to verify the validity of the RVMW. Additionally, because the TR Doppler envelope may not be acquired, and because imaging of the TR Doppler envelope is obscure in some healthy subjects, selection bias might have occurred. Furthermore, although all subjects were asymptomatic during regular examinations, we cannot rule out the possibility of subclinical cardiovascular or respiratory diseases, especially in the elderly.
5 CONCLUSIONS
This is the first comprehensive study to use echocardiography to evaluate the relationships among RVMW indices and other RV systolic and diastolic function parameters in a cohort of the healthy individuals. The results of this study show that all RVMW indices have good correlations with RV GLS. The RVMW indices may be reliable parameters of the myocardial systolic performance.
FUNDING INFORMATION
This study was supported by the Xiamen's Key Project of Medical and Health Sciences (No. 3502Z20209147) and the Science and Technology Planning Project of Xiamen (No. 3502Z20214ZD2183 and grant No. 3502Z20214ZD1166).
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.