Regenerative potential of Wharton's jelly-derived mesenchymal stem cells: A new horizon of stem cell therapy
Hossein Abbaszadeh and Farzaneh Ghorbani contributed equally to this work.
Abstract
Umbilical cord Wharton's jelly-derived mesenchymal stem cells (WJ-MSCs) have recently gained considerable attention in the field of regenerative medicine. Their high proliferation rate, differentiation ability into various cell lineages, easy collection procedure, immuno-privileged status, nontumorigenic properties along with minor ethical issues make them an ideal approach for tissue repair. Besides, the number of WJ-MSCs in the umbilical cord samples is high as compared to other sources. Because of these properties, WJ-MSCs have rapidly advanced into clinical trials for the treatment of a wide range of disorders. Therefore, this paper summarized the current preclinical and clinical studies performed to investigate the regenerative potential of WJ-MSCs in neural, myocardial, skin, liver, kidney, cartilage, bone, muscle, and other tissue injuries.
1 INTRODUCTION
Emerging data have indicated that mesenchymal stem cells (MSCs) provided a promising tool for cell therapy and regeneration of human tissues due to their differentiation multipotency, self-renewal capability, long-term ex vivo proliferation, paracrine effects, and immunomodulatory potential (El Omar et al., 2014; Wang, Yuan, & Xie, 2018b). MSCs can be collected from adult and fetal/perinatal tissues, such as bone marrow (BM), adipose tissue, endometrial polyps, dental pulp, peripheral blood as well as the placenta, endometrium, umbilical cord blood, and Wharton's jelly (Kalaszczynska & Ferdyn, 2015; Marino et al., 2019).
MSCs derived from adult tissues, especially BM, are most frequently used for therapeutic purposes, however, their use has been hampered because of some reasons such as their limited proliferative ability, low cell contents, and invasive and painful isolation procedure associated with significant morbidity and risk of infection (about 0.01–0.001% of total mononuclear cells; Mazini, Rochette, Amine, & Malka, 2019; Nancarrow-Lei, Mafi, Mafi, & Khan, 2017). Additionally, donor health, age, genetics, and exposure to environmental stress could potentially affect the proliferation and differentiation capacity of MSCs (Brown et al., 2019).
Unlike adult MSCs, Wharton's jelly derived mesenchymal stem cells (WJ-MSCs) have recently generated a tremendous level of interest for allogeneic or autologous application because of their beneficial properties including unlimited availability, low cost, large quantities, easy and noninvasive isolation procedure and higher proliferative capacity (Abbaszadeh, Ghorbani, Derakhshani, Movassaghpour, & Yousefi, 2020; Kalaszczynska & Ferdyn, 2015). WJ-MSCs are also less likely to cause graft versus host disease and appear to be nontumorigenic and do not induce teratomas after transplantation (Brown et al., 2019; El Omar et al., 2014). Additionally, these MSCs are very young cells that have affected less environmental interference (Vieira Paladino, de Moraes Rodrigues, da Silva, & Goldberg, 2019). Besides, their research does not raise any ethical concerns associated with their application in regenerative medicine. Furthermore, WJ-MSCs possess an immune-privileged status which makes them an ideal option for regenerative medical use (Marino et al., 2019).
For clinical application, WJ-MSCs should be extracted from healthy donors of full-term pregnancies over the age of 18 and who have water broken for no longer than 18 hr (Vieira Paladino et al., 2019). Furthermore, due to the higher expression of OCT-4 and DNMT1, WJ-MSCs derived from male subjects have higher and quicker differentiation potential (Balzano et al., 2019a; Balzano et al., 2019b).
Considering these advantages, in this review, we first provided a summary of the biological characteristics of WJ-MSCs. Then, we attempted to describe several recent nonclinical and clinical trials which evaluated their regenerative efficiency or safety in various disorders including neurological, cardiovascular, cutaneous, liver, and kidney diseases as well as cartilage, bone, muscle and several other tissue damages. Last, the concluding part summarized the current status, addressed existing challenges, and gave an outlook on potential future prospects.
2 ISOLATION AND CHARACTERISTICS OF WJ-MSCs
WJ is the connective tissue of the umbilical cord which was initially described by Thomas Wharton in 1656 (Davies, Walker, & Keating, 2017). The first isolation of MSCs from the WJ portion of the human umbilical cord was achieved by McElreavey and colleagues in 1991 (McElreavey, Irvine, Ennis, & McLean, 1991).
One centimeter of the umbilical cord yields approximately 1–5 × 104 MSCs (Kalaszczynska & Ferdyn, 2015). Currently, digestion-based methods are one of the most common techniques applied for the isolation of MSCs from the extracellular matrix of WJ by using collagenase, hyaluronidase, or other proteases (Liau, Ruszymah, Ng, & Law, 2019; Widowati et al., 2019). The doubling time of MSCs isolated by this technique is considerably longer, however, they may increase the risk of cellular damages and reduce cell viability. Alternatively, tissue explant can be used for WJ-MSCs isolation because of some benefits such as lower cost and higher cell yield. Due to the release of paracrine factors during the in vitro culture, the proliferative capacity of isolated WJ-MSCs through the explant method is also higher as compared to enzymatic protocols (Hassan, Kasem, Soukkarieh, & Aljamali, 2017; Kalaszczynska & Ferdyn, 2015; Liau et al., 2019).
Phenotypic investigation performed by several groups evidenced that WJ-MSCs fit the minimal criteria for MSCs as proposed by the International Society for Cellular Therapy (Dominici et al., 2006). They are spindle-shaped fibroblast-like cells expressing typical mesenchymal markers such as CD73, CD90, CD105, CD13, CD29, and CD44, while lacking expression of hematopoietic, CD45, CD34, and endothelial, CD31, markers (Corrao et al., 2013; Kalaszczynska & Ferdyn, 2015). WJ-MSCs can also be unique options for therapeutic applications due to their primitive properties, as they display several characteristics of embryonic stem cells (ESCs), such as ESC-like antigen Tra-1-60, Tra-1-81, SSEA-1, and SSEA-4, and pluripotency genes including Oct-4, Nanog, SSEA-4, and SOX-2 (Marino et al., 2019). Moreover, WJ-MSCs are safe for allogeneic therapeutic goals because of their immune-privileged status. They present a minimal expression for major histocompatibility complex (MHC) Class I and no expression for MHC-II that protect them from Natural killer cell-mediated lysis. They also lack expression of costimulatory molecules CD40, CD80, and CD86 and have high levels of immune inhibitors such as prostaglandin E2, indoleamine-2,3-dioxygenase, and HLA-G (Weiss et al., 2008; Zhou et al., 2011).
3 REGENERATIVE EFFECTS OF WJ-MSCs IN DIFFERENT TISSUES
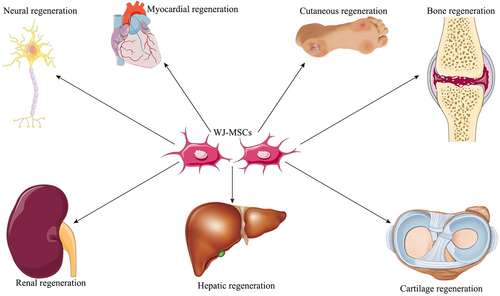
Accumulating data have recently evaluated the potential contribution of WJ-MSCs in the treatment of different diseases or tissue regeneration, which are discussed in the following parts (Figure 1).
3.1 Neural regeneration
The application of MSCs derived from human WJ has been yielded promising results in the treatment of neurological diseases. It has been established that the WJ-MSCs are capable of differentiating into neural cells (Ma et al., 2005; Peng et al., 2011). WJ-MSCs are also associated with more nerve regeneration, neuroprotection, and less inflammation following spinal cord injury (SCI) in dogs compared to adult MSCs from BM or adipose tissue (Ryu et al., 2012). In 2008, a study provided evidence that transplantation of human WJ-MSCs is an effective approach to promote the regeneration of corticospinal fibers and locomotor recovery after SCI in rats (Yang et al., 2008). Intrathecal transplantation of WJ-MSCs has demonstrated anti-inflammatory effects in SCI rat models through targeting the inflammasome complex (Mohamadi et al., 2018; Mohamadi et al., 2019). Additionally, Li et al. (2016), indicated that the recovery of motor function and integrity of the spinal cord was better in WJ-MSC transplanted rats than the control group because of reducing interleukin-1b and increasing nerve growth factor expression. It has also been concluded that the therapeutic effect of WJ-MSCs in SCI is dose-dependent and could be accelerated by repeated application (Krupa et al., 2018). Nevertheless, it has been proven by Chudickova et al. (2019) that conditioned media derived from WJ-MSCs has a superior effect than direct MSC transplantation for the treatment of SCI in rats.
In a study conducted by Fu et al (2006), human WJ-MSCs were successfully differentiated into dopaminergic neurons in vitro. Then, the administration of these differentiated MSCs into the striatum of rats with Parkinson's disease (PD) could alleviate amphetamine-induced rotation, showing their promising therapeutic effects. Transplantation of undifferentiated human WJ-MSCs was also significantly reduced amphetamine-evoked rotation in the rat model of PD (Weiss et al., 2006).
Ding et al. (2007) reported that intracerebral injection of WJ-MSCs into the stroke rat model could enhance neuroplasticity via regulating the expression of β1-integrin. Furthermore, neural differentiation of human WJ-MSCs could improve the recovery of neurological function after implantation in ischemic stroke rats (Zhang et al., 2017). Intracerebral transplantation of human WJ-MSCs has also neuroprotective effects on a rodent model of stroke through reducing inflammation and increasing the expression of trophic factors (Wu et al., 2018b).
Moreover, Wang et al. (2019) have recently investigated the therapeutic effect of human WJ-MSCs in a mouse model of transected sciatic nerves. The data showed that the human WJ-MSCs group had a significantly better functional recovery, quality of regenerated nerve, and higher neurotrophic factors in comparison with the nontreated and human adipose stem cell treated control groups.
In another study, Zhang et al. (2014a) focused on the potential of human WJ-MSCs in the treatment of neonatal rats with hypoxic-ischemic encephalopathy (HIE). The results indicated that intravenous transplantation of these MSCs at an early stage of HIE significantly improved the behavior of rats and suppressed gliosis. It has also been shown that thrombin preconditioning of human WJ-MSCs could remarkably attenuate severe HIE-induced brain infarction and improve behavioral function in neonatal rats through enhancing their anti-inflammatory, antiapoptotic and antiastroglial activities (Kim et al., 2019). Another study suggested that extracellular vesicles derived from human WJ-MSCs might protect against HI-induced apoptosis in neuronal cells by delivering let-7-5p miR (Joerger-Messerli et al., 2018).
3.2 Myocardial regeneration
The beneficial effects of WJ-MSCs in the regeneration of myocardial tissue have been shown in several studies. For instance, Lopez et al. (2013) suggested that intravenous administration of WJ-MSCs might be more beneficial than BM-MSCs as an off-the-shelf therapy for myocardial ischemia. Liu et al. (2016) found that intracoronary transplantation combined with multiple intravenous deliveries of WJ-MSCs may enhance left ventricular function, perfusion, and remodeling in the porcine model of chronic myocardial infarction. The impact of WJ-MSCs has also been evaluated in acute myocardial infarction (AMI) porcine models and followed-up to 6 weeks (Zhang et al., 2013). The transplanted MSCs were able to differentiate into cardiomyocytes, induce angiogenesis, reduce apoptosis and fibrosis, decrease infarct size, and consequently enhanced ventricular remodeling and function. Moreover, WJ-MSC therapy was shown to attenuate interstitial fibrosis and cardiac dysfunction in a dilated cardiomyopathy rat model by decreasing tumor necrosis factor-alpha and transforming growth factor-beta 1 (TGF-β1) expression and ERK1/2 signaling activation (Zhang et al., 2018b). Bhuvanalakshmi, Arfuso, Kumar, Dharmarajan, and Warrier (2017) reported that epigenetic modification could enhance the differentiation of WJ-MSCs into the cardiomyocyte lineage through regulation of Wnt mediators in cardiac injury mice model. It has also been proposed that combinatory therapy with human WJ-MSCs and insulin-like growth factor-1 significantly enhanced myocardial regeneration, angiogenesis, reduced fibrosis, and improved cardiac function in a rabbit model of MI (Rabbani et al., 2018). Furthermore, WJ-MSCs modified to overexpress antifibrotic factors provided a novel strategy for protecting cardiac fibrosis in vitro (Nimsanor, Phetfong, Kitiyanant, Kamprom, & Supokawej, 2019). It has also been shown that WJ-MSCs could be a more suitable substitute of endothelial and interstitial cells in cardiovascular regenerative medicine as compared to amniotic membrane because of their higher viability, proliferation, and superior collagen deposition properties (Pu et al., 2017).
Martin-Rendon et al. (2008) compared the differentiation potential of MSCs derived from BM, umbilical cord, and cord blood into cardiomyocytes in vitro. In spite of other studies, their result indicated that WJ and cord blood MSCs did not express cardiac-specific markers either spontaneously or after treatment with 5-azacytidine and may not able to generate an acceptable amount of cardiomyocytes in MI cell therapy without pharmacological or genetic modification.
3.3 Cutaneous regeneration
WJ-MSCs have also been broadly studied as a promising source for skin wound healing. For example, as described by Azari et al. (2011) in their article, caprine WJ-MSCs showed complete re-epithelialization of the wounds with minimum inflammation and scar formation on Day 7. However, no complete epithelialization was observed in the untreated control group after 12 days. Administration of human WJ-MSCs has also improved wound healing in an excisional full-thickness skin murine model through enhancing re-epithelialization, vascularization, proliferation, survival, and migration of skin fibroblasts (Arno et al., 2014). An animal model of burn has also been employed to confirm the potential of WJ-MSC therapy in this pathology. Subcutaneous injection of the WJ-MSCs suppressed secondary inflammation via reducing inflammatory cytokines and, therefore, promoted burn healing process and skin repair in rat burn models (Zhang et al., 2015). Sun, Zhang, Song, Zhu, and Zhu (2019) assessed the healing effects of these MSCs in radiation-induced skin injury in rats. They found that WJ-MSCs improved wound healing quality by promoting cell proliferation, sebaceous glands regeneration, and angiogenesis. Another animal study showed that WJ-MSCs primed with poly I:C or Interferon-gamma have enhanced anti-inflammatory potential in atopic dermatitis (Park et al., 2019). The impact of heterologous WJ-MSCs has also been investigated on a nonhealing large chronic wound in a filly. In this study, the application of WJ-MSCs contributed to complete wound healing with no side events or scar tissue formation (Lanci, Merlo, Mariella, Castagnetti, & Iacono, 2019). Recently, Martin-Piedra et al. (2019) also reported that because of their epidermal differentiation capability and lack of HLA antigens, WJ-MSCs are more suitable sources for the generation of bioengineered human skin substitute than MSCs derived from adipose tissue, dental pulp, and BM. Additionally, two studies have been demonstrated that a mixture of WJ-MSCs and skin microparticles could remarkably elevate the quality of cutaneous wound regeneration in mice models (Shi, Jia, Liu, & Chen, 2015; Zhang, Hao, Liu, Fu, & Han, 2012b). WJ-MSCs administrated on a decellularized amniotic membrane scaffold into the wound bed, showed reduced scar formation with hair growth (Sabapathy, Sundaram, Mankuzhy, & Kumar, 2014). Similarly, the combination of WJ-MSCs and silk fibroin scaffold exhibited significant enhancement in wound re-epithelization and reduced fibrotic scar formation (Millan-Rivero et al., 2019). Besides, the association of human WJ-MSCs and poly (vinyl alcohol) hydrogel membrane resulted in the promotion of wound healing in two dogs with chronic skin wounds where the standard treatments failed (Ribeiro et al., 2014).
3.4 Hepatic regeneration
The potential of WJ-MSCs to differentiate into the endodermal lineage, such as hepatocyte-like cells, makes them an attractive alternative for the treatment of liver diseases (Buyl et al., 2014; Mortezaee et al., 2015; Vojdani et al., 2015; Zhang, Lie, & Wei, 2009). The impact of WJ-MSCs has been investigated in a liver fibrosis rat model by Tsai et al. (2009). They reported that the administration of human WJ-MSCs could significantly reduce liver fibrosis by decreasing the collagen deposition, levels of serum glutamic oxaloacetic transaminasea, glutamic pyruvate transaminase, as well as TGF-β1 and increasing mesenchymal-epithelial transition factor–phosphorylated type and hepatocyte growth factor (HGF). Lin et al. (2010) also determined that intravenous injection of human WJ stem cells downregulate liver collagen and thus could alleviate liver fibrosis in rat models. In addition, WJ-MSCs have been proven to have the capacity in the enhancement of sepsis-associated liver damage in rats (Condor et al., 2016). Li et al. (2015) also loaded WJ-MSCs into poly scaffolds and administrated into liver-injured mice. One month after WJ-MSC transplantation, the liver morphology significantly promoted and looked similar to a normal one. Furthermore, one report has indicated that WJ-MSC therapy is able to improve liver function and rescue the hepatotoxicity induced by D-Galactosamine in acute liver injury mice model (Ramanathan et al., 2017). Zhang et al. (2012a) found that human WJ-MSCs could be a potential source for cell therapy of acute liver failure when compared to human hepatocytes, because of their ability in stimulating endogenous liver regeneration through paracrine effects. It has been also shown that intrauterine xenotransplantation of WJ-MSCs successfully relived liver injury in rabbit fetuses through inducing the expressions of albumin, α-fetoprotein, hepatic nuclear Factor 4, and CYP2B6 messenger RNA (Rezaeian et al., 2018). Another study suggested that the application of praziquantel in combination with WJ-MSCs has more beneficial effects in the treatment of the Schistosoma mansoni-induced liver fibrosis, presumably via enhancing differentiation capacity of the transplanted WJ-MSCs to functioning liver-like cells (Hammam et al., 2016).
Nevertheless, Rengasamy et al. (2017) suggested that human BM-MSCs alleviate CCl4-induced liver fibrosis more effectively than WJ-MSCs in rat models which could be associated with their expression of certain matrix metalloprotease and angiogenic factors.
3.5 Renal regeneration
With a rat model of unilateral ischemia-reperfusion injury (IRI), a single intravenous administration of WJ-MSCs exerted beneficial effects on IRI-induced acute and chronic kidney injury via an endocrine mechanism (Du et al., 2012). According to the results of this study, activated Akt signal in tubular epithelial cells (TECs) resulted in a decrease of apoptosis, the elevation of proliferation, and the induction of endogenous HGF. Similarly, another animal study demonstrated that these MSCs contributed to the induction of native and foreign HGF in damaged TECs at the initial stage of acute kidney injury (AKI), which subsequently resulted in the EMT delay and mitigation of renal fibrosis (Du et al., 2013). It has also been shown that human WJ-MSCs seeded in a decellularized kidney scaffold could ameliorate renal fibrosis through decreasing EMT by the TGF-β/Smad signaling pathway after subtotal nephrectomy in rats (Hu et al., 2020). Moreover, the human WJ-MSC potential has been proven in the promotion of renal injury in streptozotocin-induced diabetic mice (Maldonado, Huang, Yang, Xu, & Ma, 2017).
Several studies also indicated that microvesicles derived from WJ-MSCs ameliorate renal IRI through various mechanisms including regulating Erk1/2 signaling, enhancing renal cell proliferation, mitigating apoptosis and inflammation, and suppressing CX3CL1 (Chen, Yan, Song, Ding, & Du, 2017; Wu et al., 2018a; Zou et al., 2014). Zhang et al. (2014b) reported that a single infusion of human WJ-MSC-microvesicles could prevent renal injury by alleviating oxidative stress in the early stage of IRI through downregulating NOX2 expression. Moreover, extracellular vesicles released from human WJ-MSCs protected against AKI via antioxidation by improving Nrf2/ARE activation in rats (Zhang et al., 2016).
3.6 Cartilage regeneration
It has been established that human WJ-MSCs could be better sources for fibrocartilage tissue engineering compared to BM-MSCs (Wang, Tran, Seshareddy, Weiss, & Detamore, 2009). It has been shown that WJ-MSCs could be an appealing source, when combined with appropriate scaffolds, for cell therapy in cartilage disorders. Recently, Zhang et al (2019) revealed that coculture of human WJ-MSCs and primary articular cartilage cells in acellular cartilage extracellular matrix-oriented scaffold could successfully construct engineered hyaline articular acrtilage in vitro. Moreover, a study conducted by Paduszyński et al. (2016), assessed changes in transcriptional activity of cartilaginous genes through in vitro chondrogenic differentiation of WJ-MSCs on 3D poly (l-lactide-co-glycolide, PLGA) scaffolds. Their findings suggested that the chondrogenic capacity of WJ-MSCs cultured on the PLGA scaffolds could be used as a promising cell-based cartilage repair therapy. Similarly, combining WJ-MSCs with 3D HyStem hydrogel and hybrid scaffolds promoted cartilage regeneration (Aleksander-Konert, Paduszynski, Zajdel, Dzierzewicz, & Wilczok, 2016; Shie et al., 2017). Besides, WJ-MSCs embedded into collagen hydrogel underwent enhanced chondrogenic differentiation by elevating the expression of cartilage-specific matrix proteins (Chen et al., 2013). A combination of WJ-MSCs and acellular cartilage extracellular matrix scaffold also provided better quality in repair and regeneration of cartilage in comparison with microfracture in a caprine model (Zhang et al., 2018a).
It has also been indicated that WJ-MSCs have great potential for fabricating tissue-engineered cartilage without scaffold (Liu et al., 2014). Modulation of metalloproteinase gene expression in synovium and prevention of cartilage degradation reported in 30 rabbits with osteoarthritis (OA), following intra-articular administration of WJ-MSCs into the knee joint (Saulnier et al., 2015). Cheng et al. (2019) have found that combined extracorporeal shockwave therapy and WJ-MSCs are more effective for the treatment of early OA in rat knee.
3.7 Bone regeneration
Growing evidences have demonstrated that WJ-MSCs are potentially valuable candidates for bone regeneration as an alternative to BM-MSCs (Ansari et al., 2018; Cabrera-Perez et al., 2019; Kang et al., 2012; Lim et al., 2018). In a recent report, Bustos et al.(2017) have found that modulation of RUNX2/p57 expression via inhibition of JARID1B histone demethylase is associated with the upregulation of WJ-MSC osteoblastic potential. Likewise, RUNX2/p57, but not SP7 gene expression, has demonstrated to be strongly activated upon induction of WJ-MSC osteoblast differentiation (Sepulveda et al., 2017). Another study conducted by Shi, Zhou, Huang, Zhang, and Wang (2018) provided additional insight about the interactions of hydroxyapatite nanoparticles with WJ-MSCs and suggested their promising therapeutic potential in bone repair.
Todeschi et al. (2015) proposed that subcutaneous implantation of WJ-MSCs loaded onto scaffolds in mice with bone defects could result in bone regeneration by the enhancement of angiogenesis. Human WJ-MSCs seeded into hierarchical fibrous scaffolds were also shown as an appropriate strategy for bone tissue engineering (Canha-Gouveia et al., 2015). Moreover, human WJ-MSCs-loaded nano-hydroxyapatite/chitosan/gelatin scaffolds were shown as an ideal bone substitute (Jamalpoor, Taromi, Soleimani, Koudehi, & Asgari, 2019).
A recent systematic review conducted by Ansari et al. (2018) systematically analyzed the osteogenic induction capacity of WJ-MSCs. They concluded that WJ-MSCs are potential stem cell sources which could be used as an alternative to BM-MSCs for bone fracture healing.
3.8 Muscular regeneration
Recently, Su et al. (2019) reported that WJ-MSCs could restore functional impairment postmuscle injury in mice via downregulating neutrophil-mediated acute inflammation and antifibrotic effects. Kwon et al. (2016) elucidated that human WJ-MSCs and human WJ-MSC-derived XCL1 protein could be used as novel therapeutic approaches for the treatment of myopathies by their antiapoptotic effects. In addition, human WJ-MSCs successfully attenuated sarcopenia in aged mice model associated with skeletal muscle cell activation, and downregulation of apoptosis and inflammation (Wang et al., 2018a). It has also been demonstrated that TGF-β1 and ascorbic acid are effective in differentiating WJ-MSCs towards smooth muscle cells (Mesure, Huber-Villaume, Menu, & Velot, 2017). The pretreatment of WJ-MSCs with Sdf-1 was proven to play a key role in increasing their migration ability during skeletal muscle regeneration in vitro (Kowalski et al., 2017). Moreover, WJ-MSCs are associated with an increased neuro-muscular regeneration when combined with biodegradable and biocompatible biomaterials, enhancing the recovery of sensory and motor function in neurotmesis injuries (Caseiro et al., 2017).
4 THERAPEUTIC APPLICATION OF WJ-MSCs IN CLINICAL TRIALS
In a controlled case clinical trial, a 16-year-old boy diagnosed with HIE received an intrathecal, intramuscular, and intravenous infusion of WJ-MSCs. The clinical outcomes progress suggested the feasibility and safety of the triple route WJ-MSC transplantations in the HIE patient (Kabatas et al., 2018). One clinical study has also been recently investigated the safety of intrathecal administration of WJ-MSCs in 43 patients with amyotrophic lateral sclerosis (Barczewska et al., 2019). No serious adverse effects were observed during the 6-month follow-up period. Recently, Hashemi et al. (2019) reported a randomized clinical trial where acellular amniotic membrane seeded with WJ-MSCs were used for 9 days, every 3 days in five patients with chronic diabetic ulcers. This treatment accelerated wound healing through a significant decrease of the wound size and time of healing (Hashemi et al., 2019). Zhang et al. (2012a, 2012c) conducted a nonrandomized controlled trial involving 45 chronic hepatitis B patients with decompensated liver cirrhosis. Thirty patients received WJ-MSC therapy and the remaining 15 patients received saline as the control. The authors revealed that treatment with WJ-MSCs is clinically safe and mediated a significant decrease in the volume of ascites and enhanced liver function. Safety and efficacy of WJ-MSC transfusion in patients with hepatitis B virus-associated acute-on-chronic liver failure (ACLF) have been reported in an open-labeled, Phase I/II trial. No serious adverse effects were observed during this study and there was a significant increase in survival rates, improvements in liver function, and reduction in a model of end-stage liver disease scores in ACLF patients (Shi et al., 2012). Sadlik et al. (2017, 2018) presented a novel, one-stage, and minimally invasive strategy for knee cartilage regeneration in a patient using WJ-MSCs and collagen scaffold under dry arthroscopy technique. Musialek et al. (2015) treated 10 patients with AMI using WJ-MSCs, indicating the feasibility and safety of these MSCs as an off-the-shelf therapeutic agent. Likewise, a double-blind, randomized controlled trial has been performed by Gao et al. (2015) to investigate the efficacy and safety of WJ-MSCs in the treatment of patients with ST-elevation AMI. A total of 116 patients were recruited and randomly received an intracoronary injection of WJ-MSCs or placebo repeatedly, and followed-up to 18 months. It was concluded that WJ-MSCs were safe in AMI therapy and successfully improved myocardial viability and heart function.
5 CONCLUSION AND FUTURE PERSPECTIVE
As compared with adult MSCs, WJ-MSCs have prominent implications in regenerative medicine because of their several unique properties, including multipotent differentiation ability, unlimited availability, high amount, easy and noninvasive separation process, superior proliferation, and cost-effectiveness. Additionally, their immuno-privileged status, nontumorigenic features, along with no ethical issues make them a promising candidate for tissue regeneration or repair. The increasing number of studies have been evaluated the feasibility of WJ-MSCs in various diseases, however, more clinical trials are still required to warrant the safety and efficacy of this therapeutic strategy before their routine use in the clinic. Application of the WJ-MSCs in combination with scaffolds provide a three-dimensional structure which promotes their adhesion and proliferation and subsequently enhancing the therapeutic results. Besides, more understanding of the mechanisms through which the advantageous effects of WJ-MSCs are reached can facilitate the modification of these MSCs to improve their future clinical application.
ACKNOWLEDGMENTS
This work has been done as part of the M.Sc. thesis for Hossein Abbaszadeh and supported by the stem cell research center at Tabriz University of Medical Sciences, Iran (grant/award number: 60928).
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
H. A. and F. G. wrote the manuscript. M. T. drew the schematic figure. M. D. and M. Y. wrote some parts of the manuscript and edited the final version. A. M. and K. S. designed and supervised the study, whole correspondence during the paper submission.




