Biocompatibility and tissue integration of a novel shape memory surgical mesh for ventral hernia: In vivo animal studies
Abstract
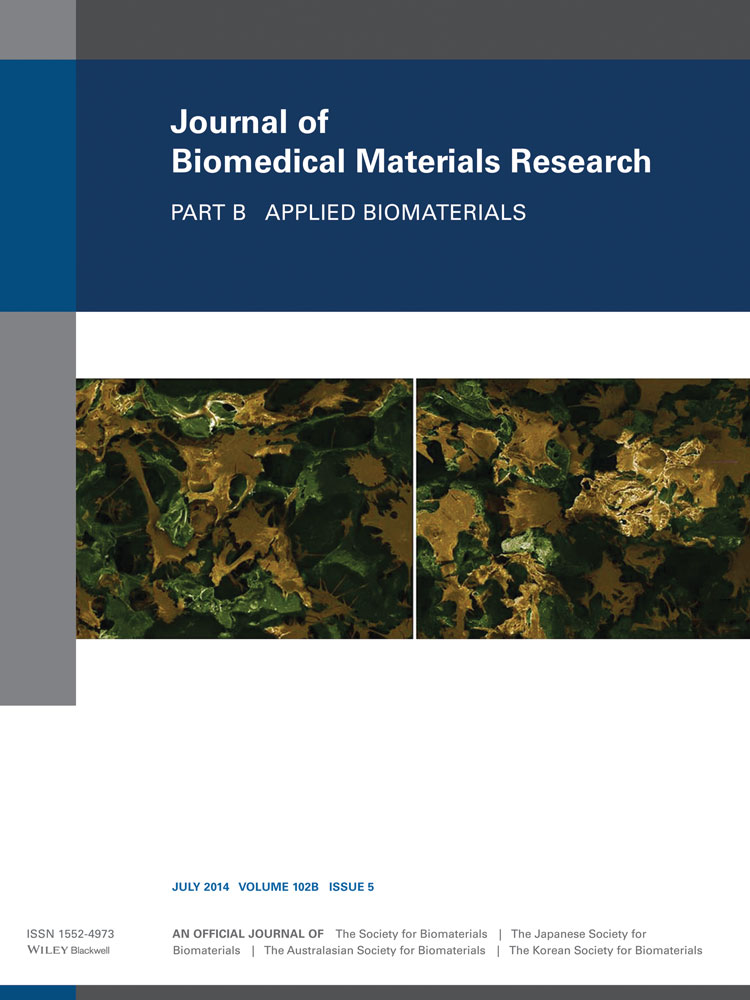
Approximately 400,000 ventral hernia repair surgeries are performed each year in the United States. Many of these procedures are performed using laparoscopic minimally invasive techniques and employ the use of surgical mesh. The use of surgical mesh has been shown to reduce recurrence rates compared to standard suture repairs. The placement of surgical mesh in a ventral hernia repair procedure can be challenging, and may even complicate the procedure. Others have attempted to provide commercial solutions to the problems of mesh placement, but these have not been well accepted by the clinical community. In this article, two versions of shape memory polymer (SMP)-modified surgical mesh, and unmodified surgical mesh, were compared by performing laparoscopic manipulation in an acute porcine model. Also, SMP-integrated polyester surgical meshes were implanted in four rats for 30–33 days to evaluate chronic biocompatibility and capacity for tissue integration. Porcine results show that the modified mesh provides a controlled, temperature-activated, automated deployment when compared to an unmodified mesh. In rats, results indicate that implanted SMP-modified meshes exhibit exceptional biocompatibility and excellent integration with surrounding tissue with no noticeable differences from the unmodified counterpart. This article provides further evidence that an SMP-modified surgical mesh promises reduction in surgical placement time and that such a mesh is not substantially different from unmodified meshes in chronic biocompatibility. © 2013 Wiley Periodicals, Inc. J Biomed Mater Res Part B: Appl Biomater, 102B: 1093–1100, 2014.