Three-dimensional time of flight magnetic resonance angiography at 5.0T: Visualization of the superior cerebellar artery
Abstract
Background
To explore the utility of 5.0T ultra-high field magnetic resonance (MR) for the assessment of the superior cerebellar artery (SCA).
Methods
Imaging data from 55 patients (19 men and 36 women) who underwent three-dimensional time of flight MR angiography (3D-TOF-MRA) with 5.0T MRI in the Shandong University Affiliated Shandong Provincial Third Hospital from May 22, 2023 to June 16, 2023 were retrospectively analyzed. The origin, caliber, and course of the SCA were recorded. An independent sample t-test was used to compare the differences in quantitative indexes between the two groups.
Results
A total of 123 superior cerebellar arteries were detected in 55 patients. We found that 86.99% of superior cerebellar arteries were longer than the P3 segment of the posterior cerebral artery. The superior cerebellar arteries were divided into nine types according to the origin of the SCA, with Type A accounting for the highest proportion (approximately 49.09%). The mean diameter of the SCA was 1.11 ± 0.22 mm, while the mean diameters of the right and left sides were 1.13 ± 0.24 mm and 1.07 ± 0.27 mm, respectively. There were no differences in SCA diameters between the two sides (p > 0.05).
Conclusions
3D-TOF-MRA with ultra-high field 5.0T MR can effectively evaluate the SCA, and provides a new effective imaging evaluation method for clinical practice.
Abbreviations
-
- 3D
-
- three-dimensional
-
- BA
-
- basilar artery
-
- FOV
-
- field of view
-
- MR
-
- magnetic resonance
-
- MRA
-
- MR angiography
-
- P3
-
- quadrigeminal segment
-
- PA
-
- pontine artery
-
- PCA
-
- posterior cerebral artery
-
- SCA
-
- superior cerebellar artery
-
- TE
-
- echo time
-
- TI
-
- inversion time
-
- TOF
-
- time of flight
-
- TR
-
- repetition time
1 INTRODUCTION
The superior cerebellar artery (SCA), which is a crucial branch of the vertebrobasilar artery system, plays an essential role in the vascular network of the infratentorial cerebellar artery. The SCA has a consistent origin and vascularization, which makes it an invaluable anatomical landmark in neuroimaging and neurosurgical procedures of the cerebellum and brainstem. In particular, the SCA is an ideal marker for delineating the path and position of the trochlear nerve [1].
In the 1990s, Barker et al. first highlighted the clinical significance of the SCA, particularly in the context of trigeminal neuralgia. In that study of 1185 cases of microvascular decompression of trigeminal nerve roots, 75% of trigeminal neuralgia cases were associated with the SCA [2]. Additionally, ischemic cerebellar strokes involving the SCA region account for approximately 36% of cerebellar infarctions [3]. As such, detailed imaging of the anatomy of the SCA is critical in diagnosing and treating cerebellar infarction, trigeminal neuralgia, hemifacial spasm, and tumors at the cerebellopontine angle.
Conventionally, assessment of the SCA involves autopsy and digital subtraction angiography (DSA), although the invasive nature and associated risks (e.g., X-ray radiation and contrast agent allergies) of DSA limit its suitability, especially for patients with mild symptoms. As such, there is increasing need for noninvasive imaging modalities for the SCA [4].
Magnetic resonance angiography (MRA), and more specifically three-dimensional time-of-flight MRA (3D-TOF-MRA), has become a prevalent noninvasive technique for examining the intracranial arteries [5, 6]. 3D-TOF-MRA has a high spatial resolution, signal-to-noise ratio, and soft tissue clarity, which provide detailed visualization of the cerebral vascular structures [7, 8]. Advances in 5.0T ultra-high field magnetic resonance (MR) scanning have significantly improved image quality [9, 10], especially for distal intracranial and small branch arteries. The high spatial resolution of 3D-TOF-MRA at 5.0T, which is based on inflow enhancement for bright blood imaging, ensures minimal phase flow loss, reduced turbulence effects, and enhanced image quality post-processing [10]. The improved contrast-to-noise ratio with this method is essential for visualizing small branch arteries [10-13]. The aim of the present study was to examine the feasibility of 3D-TOF-MRA at 5.0T for detailed analysis and visualization of the SCA.
2 MATERIALS AND METHODS
2.1 Study design
We performed a retrospective analysis on imaging data of 55 patients from Shandong University Affiliated Shandong Provincial Third Hospital, who underwent 5.0T MRA examination of the brain between May 22, 2023 and June 16, 2023 for suspected cerebrovascular diseases. This cohort included 19 men and 36 women (age range, 36−81 years). The inclusion criteria were: signed informed consent for 5.0T MR examination, completion of 3D-TOF-MRA head examination, and no history of brain trauma or brain tumor. The ethics committee of the Third Hospital of Shandong Province approved this study.
2.2 Imaging examination
2.2.1 Magnetic resonance imaging
Imaging was performed using a 5.0T ultra-high field MR system (uMR Jupiter, United Imaging Healthcare) with a two-channel transmit and 48-channel receiver head coil. All patients underwent 3D-TOF-MRA. The imaging parameters were as follows: TR = 20 ms, TE = 3.8 ms, FOV = 230 mm × 200 mm, NSA = 1, flip angle = 15°, voxel size = 0.6 mm × 0.6 mm × 0.6 mm, and acquisition time = 4 min 15 s. Both the original and post-processed images were analyzed using the SYNAPSE PACS SYSTEM, FUJIFILM.
2.2.2 Evaluation and measurement of the SCA
Four experienced radiologists independently evaluated the images. The origin, number of branches, and internal diameter at the site of the SCA origin were initially assessed by two attending radiologists, which was followed by a review by two deputy-chief radiologists. Vessels that were longer than the P3 segment of the posterior cerebral artery (PCA) were recorded [14]. The mean vessel diameter at the SCA origin was measured using the SYNAPSE PACS built-in tool.
2.3 Data analysis
Data analysis was conducted using SPSS 23.0 software (IBM). Count data are presented as n (%). The Kolmogorov−Smirnov test was used to assess the normality of the measurement data. Normally distributed data are presented as mean ± standard deviation. A p-value <0.05 was considered statistically significant. Given the nature of our data, no t-tests or additional figures for statistical analysis were required.
3 RESULTS
The 5.0T 3D-TOF-MRA effectively displayed the origin and shape of the SCA (Figures 1 and 2). Approximately 87% of patients showed an SCA that was longer than the P3 segment of the PCA. A total of 123 superior cerebellar arteries were identified in 55 patients (61 on the right and 62 on the left side of the basilar artery, BA). There was no significant difference in the diameters of the left and right vessels (t = 1.345, p = 0.184; Table 1).
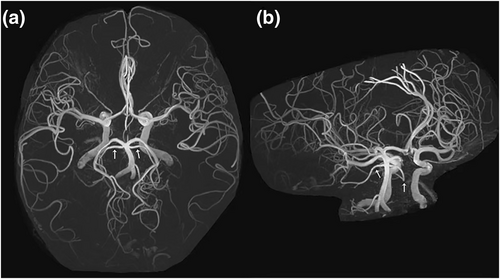
The SCA at 5.0T MR (a) posterior anterior view, (b) oblique view. Patient information: Female, 56 years old. 5.0T MRA showed a bilateral SCA originating from near the end of the BA (white arrows), with the SCA beyond the P3 segment clearly visible. BA, basilar artery; MRA, MR angiography; P3, quadrigeminal segment; SCA, superior cerebellar artery.
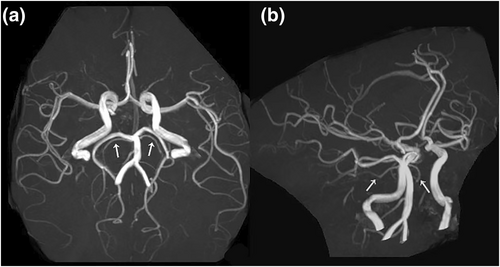
The SCA at 3.0T MR (a) posterior anterior view, (b) oblique view. Patient information: Female, 64 years old. 3.0T MRA showed a bilateral SCA originating from the BA (white arrows), with the SCA beyond the P3 segment not clearly visible. BA, basilar artery; MRA, MR angiography; P3, quadrigeminal segment; SCA, superior cerebellar artery.
| Location | Number(n) | Number of length longer than PCA-P3 segment (%) | Diameter (mm) |
|---|---|---|---|
| On the right side of basilar artery | 61 | 52 (85.25) | 1.13 ± 0.24 |
| On the left side of basilar artery | 62 | 55 (88.71) | 1.07 ± 0.27 |
| Total | 123 | 107 (86.99) | 1.11 ± 0.22 |
- Abbreviations: P3, quadrigeminal segment; PCA, posterior cerebral artery.
Based on the origin of the SCA and its relationship with the PCA, the 55 patients were categorized into nine SCA-origin types (Figure 3). Type A was the most common (approximately 49% of cases), followed by type b (approximately 24%). The proportions of the other types are detailed in Table 2.

Depiction of the nine types of origin of the superior cerebellar artery.
| Type | a | b | c | d | e | f | g | h | i | Total |
|---|---|---|---|---|---|---|---|---|---|---|
| Number (n) | 27 | 13 | 5 | 3 | 2 | 1 | 1 | 2 | 1 | 55 |
| Proportion (%) | 49.09 | 23.64 | 9.09 | 5.45 | 3.64 | 1.82 | 1.82 | 3.64 | 1.82 | 100 |
4 DISCUSSION
In the present study, we performed a retrospective analysis of the SCA using 3D-TOF-MRA at 5.0T. Because of its superior spatial resolution, we found that this technique was an excellent noninvasive tool for detailed evaluation of the SCA, which included clear delineation of its origin, caliber, and course.
The SCA is recognized for its consistent vascularization in the infratentorial cerebellar artery. It typically originates from the BA near the superior margin on the pons, and then courses around the cerebral peduncle to supply blood to key cerebellar regions [15]. The SCA is divided into distinct segments based on its distribution, and its accurate identification and clear display are crucial, especially when evaluating cerebellar infarction, trigeminal neuralgia, hemifacial spasm, and cerebellopontine angle tumors.
Previous morphological studies of the SCA were largely based on autopsy findings [11, 16, 17], although there is now increasing use of computed tomography angiography (CTA) [4, 18]. However, to our knowledge only one other study has used MRA to observe SCA morphology [19], in which 145 images were examined using a 1.5T MRI and 3D-TOF. Previous autopsy studies also reported the transverse diameter of the starting part of the SCA [1, 18]. Importantly, the SCA diameter measured by 5.0T MRA in the present study was consistent with those CTA and anatomical studies. Note that the variation in SCA diameter depending on its origin suggests a link to ischemic events, particularly post-surgical manipulations [4], which indicates the importance of cautious imaging.
Our study categorized the SCA origins into nine types, which provides valuable insight into their anatomical and clinical significance. Type a was the most common type (49.09% of patients), in which the SCA originated directly from the BA [16, 18]. Type b, which was the second most common type (23.64%), had origins from the PCA, which highlights that variations may influence the vascular supply during PCA-related pathologies or surgeries [16]. The less common types (e.g., Type c: 9.09%, Types d, e, f, g, h, and i: 1.82%–5.45%) highlight the diversity in SCA anatomy, which is critical for anticipating anatomical variations during diagnostic and therapeutic interventions [15, 16, 18].
In surgical procedures involving the cerebellum and the cerebellopontine angle, as well as in trigeminal microvascular decompression, SCA treatment was traditionally guided by clinical experience, which poses a risk for injury. Therefore, noninvasive imaging of the origin and shape of the SCA is important for early diagnosis and choosing appropriate treatment methods for SCA-related diseases. The diversity in the origin and morphology of the SCA, and its potential involvement in trigeminal neuralgia, is increasingly recognized. A number of studies have confirmed that the SCA plays a role in trigeminal nerve compression previously [20-22]. The classification of the origins of the SCA into nine types [4] (with Type A being the most common) was somewhat reflected in the present study, although we saw differing proportions, which was likely because of our smaller sample size.
Venti reported that cerebellar infarction caused by SCA lesions accounts for approximately 36% of all ischemic cerebellar strokes [3], with common symptoms including gait or saccade disorders [23]. Note that in that study, 5.0T MRA was also effective for evaluating the SCA in patients with isolated gait instability or acute attacks. The high-resolution imaging capacity of 5.0T MRA allows for detailed visualization of the SCA, which aids in the early diagnosis and management of these conditions. Compared with CTA, which is also a viable option for SCA evaluation [4, 18], 5.0T MRA avoids the risks associated with radiation and contrast agent allergies, and thus provides a safer and noninvasive alternative for these patients.
The development of 5.0T ultra-high field whole-body MR imaging has facilitated extensive clinical research, particularly in cerebrovascular applications [9, 10]. Our research demonstrates that 5.0T MR 3D-TOF-MRA imaging can effectively visualize the origin and shape of the SCA, with high consistency through anatomical findings. Our findings also suggest that 5.0T MRA is an effective strategy for diagnosing and differentiating diseases related to the SCA. The high spatial resolution and enhanced image quality of 5.0T MRA enables precise visualization of the SCA anatomy, which is crucial for identifying variations and abnormalities. These capabilities can improve the diagnosis and differentiation of conditions such as cerebellar infarction, trigeminal neuralgia, hemifacial spasm, and tumors at the cerebellopontine angle, which allows more accurate and effective clinical decision-making.
There are a number of limitations in our study. First, the limited number of patients may have restricted the statistical significance and generalizability of our results. Nevertheless, our detailed imaging and consistent methodology provide valuable insight into the anatomy and pathology of the SCA, which contributes to the existing body of knowledge in neurovascular imaging. Second, we did not perform a quantitative analysis of SCA signal strength. Nonetheless, our qualitative assessments provide substantial clinical value by improving our understanding of the anatomical variations of the SCA, as well as their potential implications in various cerebrovascular diseases. Third, the absence of further investigation into SCA-related diseases in this study limits the scope of clinical applicability. Exploring the direct correlation between SCA abnormalities and specific cerebrovascular diseases could provide more comprehensive insight. Finally, we did not validate our findings with CTA/DSA or compare with 3.0T systems. However, our study highlights the capacity of advanced 5.0T technology for high-resolution imaging and provides a basis for future comparative studies.
5 CONCLUSION
In summary, 5.0T ultra-high field 3D-TOF-MRA provides clear visualization of the origin, diameter, and course of the SCA. Thus, 5.0T 3D-TOF-MRA represents a new strategy for diagnosing and differentiating SCA-related diseases, which is a significant step forward in neurovascular imaging.
AUTHOR CONTRIBUTIONS
Ning Tian: Writing—original draft (lead). Xiangsen Jiang: Data curation (supporting). Lei Yu: Investigation (equal). Zudong Yin: Methodology (equal). Dan Yu: Writing—review & editing (supporting). Jie Gan: Supervision (lead).
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflict of interest.
ETHICS STATEMENT
Not applicable.
INFORMED CONSENT
Not applicable.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.