Novel Homozygous Mutation of the Internal Translation Initiation Start Site of VHL is Exclusively Associated with Erythrocytosis: Indications for Distinct Functional Roles of von Hippel-Lindau Tumor Suppressor Isoforms
Communicated by John McVey
ABSTRACT
Congenital secondary erythrocytosis is a rare disorder characterized by increased red blood cell production. An important cause involves defects in the oxygen sensing pathway, in particular the PHD2–VHL–HIF axis. Mutations in VHL are also associated with the von Hippel-Lindau tumor predisposition syndrome. The differences in phenotypic expression of VHL mutations are poorly understood. We report on three patients with erythrocytosis, from two unrelated families. All patients show exceptionally high erythropoietin (EPO) levels, and are homozygous for a novel missense mutation in VHL: c.162G>C p.(Met54Ile). The c.162G>C mutation is the most upstream homozygous VHL mutation described so far in patients with erythrocytosis. It abolishes the internal translational start codon, which directs expression of VHLp19, resulting in the production of only VHLp30. The exceptionally high EPO levels and the absence of VHL-associated tumors in the patients suggest that VHLp19 has a role for regulating EPO levels that VHLp30 does not have, whereas VHLp30 is really the tumor suppressor isoform.
von Hippel-Lindau disease (VHL; MIM #193300) is an autosomal-dominant benign and malignant tumor syndrome caused by heterozygous germline mutations in the VHL gene. Tumors typically develop upon somatic inactivation of the wild-type allele, consistent with a classic two-hit tumor suppressor [Frantzen et al., 1993]. In addition to the role of the VHL gene in tumor development [Friedrich, 2001; Richards, 2001; Maina et al., 2005; Nordstrom-O'Brien et al., 2010], specific VHL mutations have been described in congenital secondary erythrocytosis [Lee and Percy, 2011]. Congenital erythrocytosis is a rare disorder characterized by increased red blood cell mass. It can be classified into primary and secondary erythrocytosis discriminated by, respectively, an intrinsic defect in erythroid precursor cells accompanied by increased sensitivity to erythropoietin (EPO) levels (primary erythrocytosis), or an extrinsic defect with excessive EPO production and normal EPO sensitivity (secondary erythrocytosis) [Cario, 2005]. Some forms of erythrocytosis show features of both the primary and secondary type [Ang et al., 2002; Lanikova et al., 2013]. The precise mechanism involved in increased sensitivity to EPO remains to be determined [Lanikova et al., 2013; Tomasic et al., 2013].
With regard to pathophysiological mechanisms underlying erythocytosis, studies have revealed that hypoxia-inducible factor (HIF) plays an important role in congenital secondary erythrocytosis. HIF is an essential transcription factor regulating a cascade of genes involved in cellular and systemic responses to hypoxia, including EPO [Kaelin, 2007; Semenza, 2007]. In this pathway, the protein encoded by the VHL gene (pVHL) represents the substrate-binding subunit of an E3 ubiquitin ligase, involved in proteosomal degradation of the alpha subunit of HIF [Safran and Kaelin, 2003]. Apart from HIF and VHL, the ubiquitination process depends on proper function of prolylhydroxylase-2 (PHD2). Consequently, mutations in either HIF-2α, VHL, or PHD2 ultimately disrupt the ubiquitination process causing stabilization of HIF-2α, which dimerizes with HIF-β and promotes transcription of a high number of genes involved in the response to hypoxia [Lee and Percy, 2011].
Until recently, only two homozygous VHL mutations associated with isolated erythrocytosis had been reported. Both these mutations are located in the distal part of exon 3, encoding the C-terminal portion of pVHL. These mutations are p.Arg200Trp, also known as the mutation responsible for Chuvash polycythemia [Ang et al., 2002] and p.(His191Asp), which has been described in people of Croatian descent [Pastore et al., 2003; Tomasic et al., 2013]. Based on this, it was believed that homozygous VHL mutations associated with erythrocytosis were exclusively located at the C-terminal end of pVHL [Richards, 2001]. However, very recently, three novel missense mutations were reported affecting residues 126 (p.Asp126Asn), 138 p.(Pro138Leu), and 196 (p.Lys196Glu), resulting in congenital erythrocytosis without VHL-associated tumors [Bento et al., 2013; Lanikova et al., 2013; Sarangi et al., 2014].
We recently had the opportunity to study three patients with congenital secondary erythrocytosis. Peripheral blood samples were collected during regular controls at the outpatient clinic. Informed consent was obtained from all individuals, and procedures were performed in agreement with the declaration of Helsinki. The study was approved by the Institutional Medical Ethical Review Board.
The first patient is a 13-year-old boy of Moroccan descent, who was referred to our clinic at the age of 6 years with unexplained erythrocytosis. He presented with a history of frequent vomiting as a single symptom. His growth was normal. Full blood count showed marked erythrocytosis, including reticulocytosis (Table 1). There were no signs of hemolysis, whereas we did observe signs of iron deficiency as illustrated by high zinc protoporphyrin (ZPP) levels, low ferritin, and low serum iron levels (data not shown). Other cell lineages were normal. Erythrocytosis was accompanied by an extremely high EPO level of 13,500 IU/l (Table 1). The 2-year-old brother (patient 2) also demonstrated erythrocytosis with reticulocytosis, iron deficiency, and no signs of hemolysis. He had no clinical symptoms. Similar to his brother, he also showed an extremely high EPO level of 12,500 IU/l (Table 1). Patients 1 and 2 (Family 1, Supp. Fig. S1A) both stem from Nador in the province Al Hoceima and the region Taza-Al Hoceima-Taounate in Morocco. The third patient is a 21-year-old girl of Moroccan descent who presented at the age of 18 years with pulmonary embolism. There were no risk factors for thrombosis (normal weight, no smoking, no oral contraception, and no family history of thrombosis). Laboratory tests demonstrated erythrocytosis accompanied by reticulocytosis, Similar to patients 1 and 2, also her EPO level of 9,300 was extremely high (Table 1). This patient (Family 2, Supp. Fig. S1A) stems from Beni Bouayach in the Galaya province, which is adjacent to the province of descent of Family 1. Neither of these patients or their family relatives showed VHL-related tumors.
| Reference range | Pt 1 | Pt 2 | Pt 3 | |
|---|---|---|---|---|
| Hb (g/dl) | <12y: 11.9–14.5 | 15.9 | 18.0 | 15.9 |
| >12y: 11.9–15.5 | ||||
| Ht (l/l) | M: 0.41–0.50 | 0.58 | 0.62 | 0.57 |
| F: 0.36–0.46 | ||||
| RBC (x10^12/l) | M: 4.2–5.5 | 9.2 | 10.1 | 7.8 |
| F: 3.7–5.0 | ||||
| MCV (fl) | 80–97 | 63 | 62 | 72 |
| MCH (fmol) | 1.75–2.25 | 1.07 | 1.11 | ND |
| MCHC (mmol/l) | 19.0–23.0 | 17.1 | 17.9 | ND |
| Reticulocytes (x10^9/l) | 25–120 | 150 | 260 | 130 |
| Leucocytes (x10^9/l) | 4–10 | 6.3 | 16.8 | 4.6 |
| Trombocytes (x10^9/l) | 150–450 | 196 | 175 | 118 |
| Haptoglobin (g/l) | 0.3–2.0 | 0.3 | ND | 0.9 |
| Bilirubine (μmol/l) | 3–21 | 16 | 17 | 22 |
| EPO (IU/l) | 3–20 | 13,500 | 12,500 | 9,300 |
| ZPP (mmol/mmolHb) | 0.00–0.21 | 2.21 | 2.67 | 2.11 |
| Ferritin (μ/l) | M: 25–255 | 42 | ND | 7 |
| F: 20–150 | ||||
| Serum iron (umol/l) | 8–33 | 9 | ND | 6.2 |
| Transferrin (g/l) | 2.00–4.00 | 1.64 | ND | 2.3 |
| Hepcidin (nM) | M: 4.5 | <0.5 | ND | ND |
| F: 2.0 (premenopausal) |
- ND, not determined.
To establish the molecular basis of erythrocytosis in the three patients, we performed DNA sequence analysis of the genes encoding hemoglobin (HBA1, NM_000558.4; HBA2, NM_000517.4; HBB, NM_000518.3), bisphosphoglycerate mutase (BPGM, NM_199186.2), HIF-prolyl hydroxylase 2 (EGLN1, NM_022051.2), von Hippel-Lindau tumor suppressor (VHL, NM_000551.3), and HIF-2α (EPAS1, NM_001430.4) [Bento et al., 2014]. No mutations were detected in HBA1, HBA2, HBB, BPGM, EGLN1, and EPAS1 in all three patients. DNA sequence analysis of VHL demonstrated a homozygous G>C nucleotide substitution at cDNA nt 162 in exon 1 of VHL (Supp. Fig. S1B) in all three patients (mutation submitted to http://www.lovd.nl/VHL). The c.162G>C mutation encodes the substitution of methionine by isoleucine at position 54 of the long isoform of VHL, VHLp30 (Fig. 1). Homozygosity in all patients was confirmed by demonstrating heterozygosity for the c.162G>C change in the parents’ DNA. Patient 3 has two brothers and one sister. One brother and one sister were found to be heterozygous for the same mutation. The other brother was normal. All these siblings were clinically and biochemically normal.
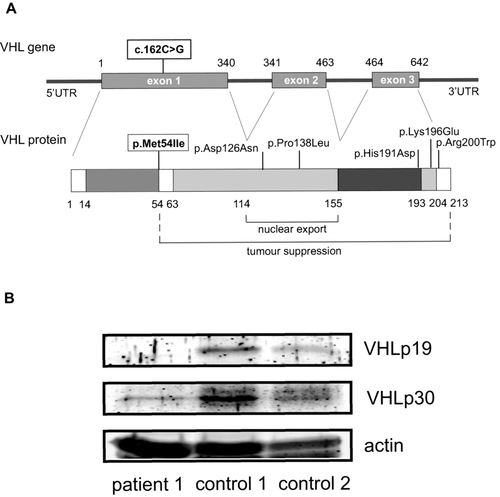
The p.(Met54Ile) substitution concerns a conservative amino acid substitution that may be well tolerated, as predicted by in silico analysis using SIFT (predictions for nonsynonymous amino acid substitutions, http://sift.jcvi.org; accessed December 15, 2014) [Kumar et al., 2009] and PolyPhen-2 (http://genetics.bwh.harvard.edu/pph2/, accessed December 15, 2014) [Adzhubei et al., 2010]. However, apart from encoding a methionine to isoleucine change, c.162G>C affects the internal translational start site from which translation of the short isoform of VHL (VHLp19) is initiated [Schoenfeld et al., 1998]. Hence, this mutation is predicted to abolish VHLp19 expression. To confirm this, we analyzed the expression of both VHL isoforms in peripheral blood mononuclear cells from patient 1 and two healthy controls, isolated from whole blood samples. We observed a comparable expression of VHLp30 in all three subjects. However, VHLp19 expression was not detected in cells from patient 1, whereas it was clearly expressed in both controls (Fig. 1B). This confirms that VHL c.162G>C completely abolishes VHLp19 protein expression.
The c.162G>C p.(Met54Ile) substitution is associated with congenital secondary erythrocytosis, yet not with the VHL-associated tumor syndrome. The unique nature of the mutation implies that the patients described here can be regarded as natural “knock-outs” for the VHLp19 isoform. Hence, they provide us with the opportunity to study the functions of the VHLp30and VHLp19 isoforms and their physiological significance in the human context [Lisztwan et al., 1999; Lolkema et al., 2005; Frew et al., 2013]. The knowledge concerning the role of VHL in congenital erythrocytosis is predominantly derived from patients homozygous for the p.(Arg200Trp) mutation in VHL (Chuvash polycythemia). In patients with Chuvash polycythemia, increased EPO levels are accompanied by increased sensitivity of their erythroid progenitors to EPO [Ang et al., 2002]. To investigate whether the VHL p.(Met54Ile) substitution was also associated with increased sensitivity to EPO, we cultured peripheral blood mononuclear cells isolated from whole blood samples of patients 1 and 3 on methylcellulose media in the absence or presence of various concentrations of EPO. Compared with healthy controls, we observed no differences in EPO sensitivity in erythroid progenitors from patients 1 and 3 (Supp. Fig. S2). In particular, no spontaneous colony formation was observed in the absence of EPO. This suggests that the p.(Met54Ile) mutation is not associated with EPO hypersensitivity. As stated, this contrasts with features of the VHL p.(Arg200Trp) mutation, but is similar to what is seen with cells harboring the Croatian erythrocytosis mutation p.(His191Asp) [Tomasic et al., 2013].
Chuvash polycythemia is accompanied by a variety of complications, including an increased risk of thrombotic and hemorrhagic strokes and pulmonary hypertension (PHT) that together result in a decreased survival [Gordeuk and Prchal, 2006]. Studies in a murine model of Chuvash polycythemia correlated PHT to increased HIF2 activity [Hickey et al., 2010; Tan et al., 2013], and not exclusively to the clinical effects of erythrocytosis. The oldest patient in our study (Patient 3, 21 years old) presented with pulmonary embolism. While diagnostic evaluation suggested the presence of PHT, this has not been confirmed. Nevertheless, one can speculate that PHT results from recurrent pulmonary embolisms secondary to erythrocytosis, or involves modulation of the VHL-HIF axis, comparable to what has been suggested for Chuvash polycythemia [Hickey et al., 2010; Tan et al., 2013].
Intriguingly, EPO levels detected in our patients were extremely high (range 9,300–13,500 IU/l), which is on average 80 times higher than EPO levels reported from Chuvash patients, and also considerably higher than EPO levels in the Croatian patient population [Tomasic et al., 2013]. This suggests that feedback regulation of EPO levels, involving the PHD2–VHL–HIF axis, at least partially depends on VHLp19 function.
None of the patients, or family members, harboring the c.162G>C p.(Met54Ile) mutation was diagnosed with VHL-associated tumors. Even when considering the relatively young age of the patients, the absence of tumors suggests that VHLp30 represents the true tumor suppressor isoform. The c.162G>C p.(Met54Ile) mutation affects a residue in close proximity to the N-terminal end of VHL. Apart from the p.Glu10* nonsense mutation, reported only in the heterozygous state [Bento et al., 2014], it is the most upstream homozygous mutation identified thus far in congenital erythrocytosis. Previously, it was postulated that VHL mutations associated with isolated erythrocytosis were exclusively located at the C-terminal end of the VHL gene [Richards, 2001], and VHL mutations associated with tumor syndromes were spread throughout the gene [Nordstrom-O'Brien et al., 2010]. In particular, families with nonsense mutations, as well as cases with somatic mutations specifically affecting the VHLp30 isoform (e.g., c.3G>A) have been described. They manifest with typical VHL tumor development, and isolated renal carcinoma, respectively [Olschwang et al., 1998; Gallou et al., 2001; Dollfus et al., 2002]. Recent findings [Bento et al., 2014] and this report demonstrate, however, that this perception is inaccurate, and that homozygous VHL mutations associated with congenital erythrocytosis can be located throughout the coding region of VHL. Intriguingly, the combination of VHL tumor syndrome, together with erythrocytosis is a rare finding. The nature of the causative mutation, and concomitantly altered protein function and expression levels, or additional mutations may play a role in the ultimately resulting phenotype. In order to better understand genotype–phenotype correlations, further investigations are required.
Taken together, we describe a new homozygous mutation in VHL. Homozygosity for this mutation, p.(Met54Ile), results in the loss of VHLp19 protein expression, which we have confirmed in patient-derived cells. The exceptionally high EPO levels and the absence of VHL-associated tumors suggests, for the first time, two distinct functional roles of the two VHL isoforms: VHLp19 is a key regulator of EPO levels, whereas VHLp30 predominantly functions as a potent tumor suppressor.
The patients described here all originate from a distinct area (distance within 80 km) in northern Morocco. Haplotype analysis of VHL [Liu et al., 2004] showed that all patients homozygous for the p.(Met54Ile) mutation have an identical haplotype (rs1056286:T, rs722509:T, rs779805:A, rs779808:T, rs1678606G, 1149A>G:A, rs696356:C, rs378630:A). Therefore, similar to the Chuvash and Croatian VHL mutations, the p.(Met54Ile) mutation reflects a new ethnic erythrocytosis syndrome (“Moroccan erythrocytosis”), probably derived from a single founder.
Acknowledgments
The authors sincerely wish to thank the family members for their kind cooperation.
Disclosure statement: The authors have no conflict of interest to declare.




