Assessing How Reduced Expression Levels of the Mismatch Repair Genes MLH1, MSH2, and MSH6 Affect Repair Efficiency
Contract grant sponsors: European Research Council (2008-AdG-232635); European Research Council (2012-PoC-324604).
Communicated by Finlay A. Macrae
ABSTRACT
Lynch syndrome (LS), the most common familial colon cancer, is associated with mismatch repair (MMR) malfunction. As mutation carriers inherit one normal and one defected MMR gene allele, cancer risk can be considered as limited amount of normal MMR gene product. How reductions in different MMR gene expressions affect MMR capability is, however, not known. The in vitro MMR assay is a method for the pathogenicity assessment of MMR gene variants causing functional or expressional defects and thus also suitable to evaluate the effects of reduced expression of normal mRNA. Here, the assay was applied to quantify repair efficiencies of human cells retaining varying expression levels (25%/50%/75%) of the main LS susceptibility genes MLH1, MSH2, or MSH6. Compared with the shRNA knockdown control, already a 50% reduction in mRNA levels could be detected as decreased MMR function although without statistical significance in MLH1. In MSH2 and MLH1, total loss of MMR was achieved with 25% expression, whereas in MSH6 and MSH2, the repair capability decreased significantly already with 75% expression. Our results provide a preliminary indication of relative expressions required for wild-type function and suggest that the in vitro MMR assay could be used to recognize expression levels indicative of LS.
Introduction
Lynch syndrome (LS, previously referred to as hereditary nonpolyposis colorectal cancer; HNPCC; MIM #120435) is an inherited cancer predisposition syndrome caused by defected DNA mismatch repair (MMR). The majority of LS causing mutations are found in MLH1 (MIM #120436), MSH2 (MIM #609309), MSH6 (MIM #600678), and PMS2 (MIM #600259) [Vasen et al., 2013], and the cancer predisposition is inherited through one defective MMR gene allele. Although MMR gene haploinsufficiency may affect the MMR mechanism prior to cancer onset [Alazzouzi et al., 2005; Muller et al., 2008], tumorigenesis is though to require the loss of the second allele [Knudson, 1971; de la Chapelle, 2004]. Thus, the primary identification of an LS family and LS diagnosis currently relies on the mutation analysis of an affected family member with microsatellite instability (MSI) and/or the lack of an MMR protein in the tumor tissue. However, the inability for MSI analysis to distinguish between MSI positive LS and sporadic cancers presents a challenge in LS diagnosis as approximately 15%–20% of sporadic colorectal cancers (CRCs) present MSI as well [Benatti et al., 2005; Merok et al., 2013]. Furthermore, the tumor MSI phenotypes vary greatly. Depending on the MMR gene affected, MSI may be characterized by mono- and/or dinucleotide repeat instability and it may be detected by all (MSI-H), one (MSI-L), or none (microsatellite stable) of the markers used [Umar et al., 2004]. On the other hand, protein expression detected by immunohistochemical (IHC) staining is not an indication of the proteins ability to function in MMR, which may falsely prevent LS from being recognized. Finally, in mutation analysis the detection of a variant of uncertain significance (VUS), whose effect on the protein expression and function is not known complicates the LS diagnosis as varying alterations can have a significantly different effect on the tumor phenotype [Ellison et al., 2001; Raevaara et al., 2005; Kansikas et al., 2011].
Because of these limitations in the current diagnostic methods and the knowledge that cancer risk in LS is associated with decreased expression of normal MMR gene, we aimed to study how well the functional deficiency caused by decreased, but not yet lost mRNA expression could be detected. Here, using an in vitro MMR assay, we assess the MMR efficiency of noncancerous human cells stably retaining varying mRNA expression levels of the most commonly mutated LS predisposition genes MLH1, MSH2, or MSH6 and the ability to functionally distinguish decreased expressions.
Materials and Methods
Establishing Knockdown Cell Lines with shRNA Stable Transfection
Mismatch repair gene specific stable knockdown (KD) lineages were made with SureSilencing™ shRNA plasmid DNA (SABiosciences/QIAGEN, Valencia, CA, USA) according to manufacturer's instructions. For that, human hTERT-1604 immortalized fibroblasts [Ouellette et al., 2000; McDaid et al., 2009] were grown in high glucose DMEM supplemented with 2% penicillin streptomycin, 10% fetal bovine serum, and 2× nonessential amino acids (Invitrogen, Carlsbad, CA, USA). Lipofectamine 2000 (Invitrogen) was used for reverse transfection of the advanced endofree purified plasmid DNA (QIAGEN). MMR genes MLH1, MSH2, and MSH6 were targeted individually with one of four different target sequences for establishing cell lines with varying expression levels of gene of interest (GOI). A control cell line (NC) was transfected with a shRNA vector with no known target specificity in the human genome. Transfected cells were selected with hygromycin B (Invitrogen) at 150 μg/μl and a minimum of two rounds of clonal isolation was carried out to ensure a homogenous cell line population.
RNA Extraction and RT-Q-PCR
All shRNA transfected clonally isolated cell lineages were expanded to 3 × 106 cells and homogenized with QIAshredder (QIAGEN). Total RNA was extracted with RNeasy Plus Kit (QIAGEN) according to manufacturer's instructions and the quality and quantity of extracted RNA was measured using a spectrophotometer (Nanodrop 2000; Thermo Scientific, Pittsburgh, PA, USA). Reverse transcription of 2.5 μg of RNA was carried out with the Superscript® VILO cDNA synthesis kit (Invitrogen). The absence of genomic DNA was confirmed by conventional S15 PCR methods (primer sequences and cycling conditions are available upon request). Quantitative PCR (Q-PCR) with provider recommended TaqMan® assays (Applied Biosystems, Pleasanton, CA, USA) for MLH1 (Hs00179866_m1), MSH2 (Hs00953523_m1), and MSH6 (Hs00264721_m1) was carried out using GAPDH (MIM #138400, Hs02758991_g1), HPRT1 (MIM #308000, Hs02800695_m1), and ACTB (MIM #102630, Hs01060665_g1) as reference genes. A geNorm analysis was carried out to confirm the stability of the reference genes in the hTERT fibroblasts [Vandesompele et al., 2002]. The assays were run using TaqMan® Universal PCR Master Mix (Applied Biosystems) on a StepOnePlusTM machine (Applied Biosystems). For each shRNA transfected cell line, expression levels of the GOI were quantified by normalization to the reference genes and calculated according to the 2−ΔΔCT method [Bustin, 2000]. All Q-PCR assays were performed in triplicates together with NC as a reference sample (positive control). Clones retaining approximately 25%, 50%, and 75% of the GOI expression compared with NC were chosen for functional analysis.
Nuclear Protein Extraction and Quantification
To assess the functional effects of MMR gene expression changes, the nuclear proteins of KD cell lines and NC controls were extracted in parallel as previously described [Holmes et al., 1990; Kantelinen et al., 2010]. Approximately 2 × 108 cells were collected and disrupted. The nuclei were collected and proteins extracted prior to sample dialysis. The nuclear protein extracts (NE) were quantified with the Qubit 1.0 fluorometer (Invitrogen) and a Western blot (WB) analysis was performed to verify the presence of the protein of interest as previously described [Kantelinen et al., 2010]. α-Tubulin was used as a loading control.
In Vitro MMR Assay
The repair efficiency of each selected KD cell line and its respective NC control was measured at 100, 75, and 50 μg of nuclear proteins in the in vitro MMR assay [Nyström-Lahti et al., 2002; Kariola et al., 2004; Ollila et al., 2008]. A mock sample with no added nuclear proteins served as negative control. A previously described heteroduplex molecule including a GT mismatch and shown to be the most efficient DNA substrate in MMR [Thomas et al., 1991; Drummond et al., 1995; Kantelinen et al., 2010] was used in excess (100 ng) in all reactions. Moreover, our previous study has shown that the protein complex of MSH2 and MSH3 (MutSβ) does not contribute to the repair of GT mismatches allowing the functional assessment of MutSα subunits without functional redundancies [Palombo et al., 1996; Kantelinen et al., 2010]. The repair efficiency of the nuclear proteins can be measured through a restriction analysis that detects the presence of a novel restriction site created by the conversion of the GT heteroduplex to an AT homoduplex [Lahue et al., 1989]. Absolute repair efficiencies (AR%) were measured as the amount of repaired DNA of the total amount of DNA in the sample as detected by the Image-Pro 4.0 analysis and processing software (Media Cybernetics, Rockville, MD, USA). Relative repair efficiencies (RR%) were calculated by comparing the AR% values of KD NE to corresponding NC extracts in the assay. Statistical student's t-test analysis was performed on 2–3 repetitions.
Results
MLH1, MSH2, and MSH6 KD Cell Lines
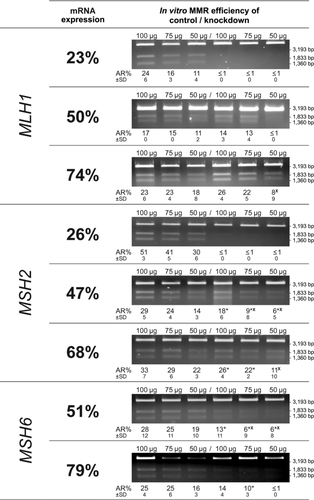
To study the effect of reduced mRNA expression on the in vitro MMR efficiency 24 MLH1, 16 MSH2, and 19 MSH6 KD fibroblast clones were first characterized by RT-Q-PCR. For MLH1, we selected cell lines retaining 23%, 50%, and 74%, for MSH2 cell lines retaining 26%, 47%, and 68%, and for MSH6 only two cell lines, retaining 51% and 79% of GOI expression, as MSH6 expression below 46% was not achieved despite testing clones from multiple rounds of transfection using four different shRNA target sequences (Supp. Fig. S1, available online). Although the protein expression was not used for quantification, the presence of the protein of interest in each nuclear protein extract was verified with a WB analysis. Here, especially the KD clones retaining 50% or less of mRNA expression revealed a lowered amount of GOI protein compared to the respective NC (Supp. Fig. S2). Only the reduction of MSH2 protein in the KD clone with 26% MSH2 mRNA expression was not clear. The clone with 50% MLH1 mRNA expression was shown to have an unexpectedly low amount of the MLH1 protein. Similar enormous decrease in MLH1 protein was also seen in another clone with 46% MLH1 mRNA expression.
The Effect of Decreased MMR Gene Expression on the MMR Efficiency
In order to investigate the effects of reduced mRNA expression on the MMR, nuclear proteins extracted from KD cells were analyzed in the in vitro MMR assay. The average absolute repair (AR%) efficiencies of KD cells and their controls, calculated from 2 to 3 repetitions, are illustrated in Figure 1. As the optimal amount of NE used in the MMR assay, to reveal even the slightest repair capability of the tested protein extract, is 75 μg or more [Nystrom-Lahti et al., 2002; Raevaara et al., 2003; Kantelinen et al., 2010], here, by using different amounts of NE (100, 75, or 50 μg) in the reaction, we demonstrated that the optimal amount of NE for MMR deficiency detection depends on the GOI. The key MMR genes, MLH1 and MSH2, caused total MMR deficiency when their expression was reduced to 25% of NC expression. This MMR deficiency was not reversed by increasing the amount of NE in the assay. Similarly, a significant decrease in the MMR efficiency was observed with clones retaining 50% of MSH2 or MSH6 mRNA expression and using either 100 μg (P = 0.001 and P = 0.002, respectively), 75 μg (P = 0.009 and P = 0.003, respectively), or 50 μg (P = 0.013 and P = 0.004, respectively) of NE. Regardless of the low level of MMR efficiency even in the controls, a decrease in the cells retaining 50% of MLH1 mRNA expression could also be detected with 100 μg of protein extract although here the decrease was not found to be statistically significant (P = 0.06). However, by reducing the amount of the extract to 50 μg the cells totally lost their repair capability. Interestingly, the cells retaining as much as 75% of MSH2 or MSH6 mRNA expression repaired significantly less efficiently than the control cells when using 100 μg (P = 0.006) or 75 μg (P = 0.043) of MSH2 NE or 75 μg (P = 0.03) of MSH6 NE in the assay, and not at all if only 50 μg of the MSH6 extract was used. The average absolute and relative repair efficiencies of KD cells assayed with 100 μg of protein extract are illustrated in Figure 2. The individual absolute repair efficiencies of all KD and NC clones are listed in Supp. Table S1.

Discussion
Individuals predisposed to LS inherit one normal and one defected MMR gene allele leading to a condition where the amount of the mRNA coding for functional MMR protein is reduced to approximately half in all the cells of a mutation carrier. Here, the in vitro MMR assay was used to evaluate whether this kind of reduction could be recognized by the decreased repair efficiency in noncancerous cells.
Our findings suggest that the level of MMR gene mRNA expression in the cell is proportional to its MMR efficiency. While the mRNA quantification results correlated well with the respective in vitro MMR efficiencies across all three genes, the MMR gene mRNA expression did not always correlate with the protein expression detected in WB analysis. This may indicate for example degradation or aggregation of the protein molecules, which affect antibody recognition, binding and detection during WB. Overall, our results suggest that WB is not sufficient to indicate MMR efficiency. Assessing how reduced mRNA levels affect repair efficiency we show that irrespective of the amount of NE used in the assay, the MMR capability was lost in cells retaining only 25% of MLH1 or MSH2 mRNA expression, whereas 50% of each, MLH1, MSH2, or MSH6 mRNA expression, is sufficient to maintain slight MMR. This may implicate that the efficient KD of one MMR gene disturbs the correct relative amount of proteins involved in the MMR mechanism in a manner that is not rescued by simply increasing the amount of the extract in the repair reaction. Similar to a previous study demonstrating that quite a low level of MLH1 protein is sufficient for MMR [Cejka et al., 2003], we show that even though 25% of MLH1 mRNA expression is not enough, cells retaining 50% of expression show higher relative repair efficiency than the cells retaining similar levels of MSH2 or MSH6 mRNA expression. Our results are also in accordance with a study demonstrating that lymphoblasts from MSH2 mutation carriers have significantly reduced MMR efficiencies and an increased tolerance to methylating agents, whereas most of the lymphoblasts from MLH1 carriers behaved similarly to normal lymphoblasts [Marra et al., 2001]. Indeed, by using the cytoplasmic proteins of human lymphocytes in an Escherichia coli based MMR assay, it was also shown that the MMR efficiency of cells retaining approximately 50% of the MSH2 protein is significantly reduced. Furthermore, similar to a previous study where the MSH2 protein depletion to 10%–50% of the wild type resulted in MSI [Mendez-Bermudez and Royle, 2011], our results suggest that the MMR mechanism is highly sensitive to MSH2 expression changes.
Currently, the primary identification of LS is highly dependent on the IHC and MSI analyses of a putative LS patient's tumor tissue and according to the two-hit hypothesis, on tumor phenotype indicating that both alleles of an affected MMR gene are inactivated in a tumor [Vasen et al., 2013; Knudson, 1971]. MSI analyses effectively identify MMR deficient tumors, however, the sensitivity is highly dependent on the panel of markers used and up to 20% of sporadic CRCs are also MSI-H, due to MLH1 promoter hypermethylation [Kane et al., 1997; Benatti et al., 2005]. IHC has shown to be effective in identifying LS among high risk CRC patients [Caldes et al., 2004; Shia, 2008]. Especially the correlation between negative MSH2 staining and variant pathogenicity has been shown to be high [Ollila et al., 2006]. Nevertheless, protein expression is not always indicative of the proteins ability to function as is seen, for example, with nontruncating deleterious MLH1 mutations [Raevaara et al., 2005]. In fact, a notable amount of MMR gene variations are nontruncating with uncertain significance, whose effect on the protein expression and function may vary from complete elimination to little or no effect [Raevaara et al., 2005; Ollila et al., 2006; Kantelinen et al., 2012]. Hence, in addition to evaluating the effect of LS carrier-like clones with 50% expression, we functionally assayed clones retaining mRNA expression levels above and below it to account for variable expression levels due to different types and locations of LS causing alterations. The identification of LS is challenging not only due to variable degrees of mutation pathogenicity but also varying penetrance needing specific methods for segregation analysis [Moller et al., 2011]. Recently an enormous collaborative effort was accomplished by The International Society for Gastrointestinal Hereditary Tumours (InSiGHT, www.insight-group.org) to gather all available clinical and functional data of over 2300 unique constitutional MMR gene variants. The data was used to develop, test, and apply a standardized five-tiered system for VUS classification, which will help in their pathogenicity interpretation and will greatly facilitate the consistent management of families carrying VUS [Thompson et al., 2014]. However, the VUS interpretation process remains very labor intensive.
Because of these complexities in LS identification, we wanted to study how different mRNA expression levels of the MMR genes MLH1, MSH2, and MSH6 affect repair efficiency and whether the reduction in MMR gene expression comparable to LS mutation carriers could be detected as a quantitative decrease in repair efficiency. Our results provide the first indications that the assay is sensitive enough to identify different degrees of pathogenicity and show that with all three genes even a 50% decrease in mRNA expression is detectable with the in vitro MMR assay although the optimal detection levels and assay conditions vary between genes. Thus, by providing a preliminary indication of gene-specific thresholds that reflect the amount of mRNA required for repair proficiencies, we suggest that the in vitro MMR assay could be used to recognize expression levels indicative of LS.
Acknowledgments
We thank Walsh Column for kindly providing the fibroblast cell line and Marjaana Pussila for her guidance with the RT-Q-PCR analyses. This study was supported by grants from the European Research Council (2008-AdG-232635, Proof of Concept Grant 2012-324604) and The Graduate Program in Biotechnology and Molecular Biology.
Disclosure statement: M.N. and M.K. are inventors on patent number PCT/EP2012/062708. M.N. is a shareholder and M.K. is an employee of LS CancerDiag Ltd.




