Expanding and Underscoring the Hepato-Encephalopathic Phenotype of QIL1/MIC13
Abbreviations
-
- 3MCGA
-
- 3-methylglutaconic acid
-
- ALF
-
- acute liver failure
-
- ARDS
-
- acute respiratory distress syndrome
-
- EM
-
- electron microscopy
-
- GGT
-
- gamma-glutamyl transferase
Mitochondrial disease can present with rapid infantile liver failure. Two sibling pairs with variants in QIL1, a gene important for mitochondrial contact site and cristae organizing system (MICOS) function, were recently reported on. They had intermittent liver disease, mild cardiac hypertrophy, cerebellar atrophy, acquired microcephaly, neurological impairment, and death before age 5 (12 months to 5 years). Patients also had lactic acidosis and urinary excretion of 3-methylglutaconic acid (3MCGA).1, 2 An additional case had renal stones, liver failure, and progressive neurological decline with death at 22 months.3 We discuss 7 unreported patients.
Clinical History
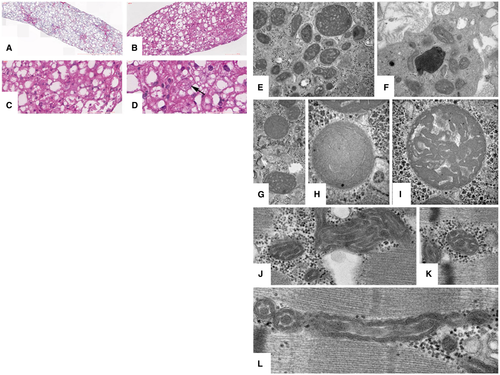
Patients 1 and 2 were monozygotic twin sisters who presented with fulminant liver failure at 3 months (Table 1). Electron microscopy (EM) demonstrated unusual cristae configurations in hepatocytes and Kupffer cells, but subtle abnormalities in skeletal muscle mitochondria initially interpreted as normal (Fig. 1). Their mild neurological findings were attributed to liver disease, so they were listed for transplant but died of liver failure. A younger sister (patient 3) had elevated liver function studies at birth. At 9 months, her liver disease was stable. She died at 13 months. Patient 4 had neonatal onset of transient liver disease with death at 10 months from acute respiratory distress syndrome (ARDS). His older sister (patient 5) exhibited a similar course. Liver histology showed enlarged mitochondria (Fig. 1). A sister of the father (patient 6) had a similar course 24 years earlier. Patient 7 had neonatal onset of transient liver failure. She had bouts of liver disease with severe diarrhea and neurological deterioration and died at age 3 in the course of acute liver disease with vomiting and seizures.
| Patients | Birth Parameters | Presentation | Laboratory Findings | Medical Course |
|---|---|---|---|---|
| 1 (Family 1) | Gestation: 34 weeks | Month 2: elevated liver enzymes | Month 2: ALT 131 (12-49 u/L); AST 227 (20-98 u/L); total Bili 4.2 (0.1-10.3 mg/dL); direct Bili 3.6 (0.0-0.4 mg/dL) | Day 1: poor feeding; 17-day NICU stay |
| Female | Weight: 1,800 g | Month 3: ALT 1,206; AST 2,153; ALP: 923 (81-316 u/L); GGT 88 (7-168 u/L); total Bili 12.4; ammonia <10 (<49 µmol/L); lactic acid: 2.7 (1.0-3.5 mmol/L); INR: 2.5; fibrinogen: 96 (200-400 mg/dL); factor V: 27.04 (50%-150%) | Month 1: newborn screen with elevated tyrosine, repeat with methionine elevated | |
| Hispanic | Monozygotic twins | Urine 3MCGA | Month 2: elevated liver enzymes without jaundice or coagulopathy | |
| d. 4 mo | Month 3: Jaundice with worsening liver enzymes and coagulopathy developing into ALF; poor feeding; brain MRI with normal spectroscopy | |||
| Genetic variant: c.260del (p.Gly87Alafs*3) | Month 4: decompensated quickly in the OR with anesthesia and line placement; liver transplant aborted and returned intubated; died 10 days later at 4 months old with multiorgan failure | |||
| 2 (Family 1) | Gestation: 34 weeks | Month 2: elevated liver enzymes | Month 2: ALT 229 (12-49 u/L); AST 296 (20-98 u/L); total Bili 3.3 (0.1-10.3 mg/dL); direct Bili: 2.7 (0.0-0.4 mg/dL) | Day 1: poor feeding; 17-day NICU stay |
| Female | Weight: 1,990 g | Month 3: ALT 829; AST 1,372; ALP 974 (81-316 u/L); GGT 80 (7-168 u/L); total Bili 7.5; ammonia <10 (<49 µmol/L); lactic acid 4.4 (1.0-3.5 mmol/L); INR: 2; fibrinogen 129 (200-400 mg/dL); factor V 30.02 (50%-150%) | Month 1: newborn screen with elevated tyrosine, repeat with methionine elevated | |
| Hispanic | Monozygotic twins | Urine 3MCGA | Month 2: elevated liver enzymes without jaundice or coagulopathy | |
| d. 4 mo | Month 3: jaundice with worsening liver enzymes and coagulopathy developing into ALF; poor feeding; liver biopsy with subacute massive hepatic necrosis with collapse, prominent giant cell transformation of residual parenchyma with early micronodular cirrhosis; normal muscle and skin biopsy and brain MRI spectroscopy | |||
| Genetic variant: c.260del (p.Gly87Alafs*3) | Month 4: unlisted for liver transplant given biopsy and sister's clinical course; died at 4 months with worsening coagulopathy | |||
| 3 (Family 1) | Gestation: 40 weeks | Day 1: poor feeding, hypoglycemia, hypothermia; ALF with elevated liver enzymes on day 2 | Day 2: low glucose 40 (47-110 mg/dL); ALT 85 (12-49 u/L); AST 332 (20-98 u/L); ALP 438 (81-316 u/L); GGT 598 (7-168 u/L); total Bili 10.7 (0.1-10.3 mg/dL); direct Bili 0.6 (0.0-0.4 mg/dL); ammonia 60 (<49 µmol/L); lactic acid 8.6 (1.0-3.5 mmol/L); PT 29.1 (9.6-11.6 seconds); INR 2.94; fibrinogen <70 (200-400 mg/dL); Factor V 22.57 (50%-150%) | Day 1: poor feeding and hypoglycemia requiring gavage feeds and intravenous fluids |
| Female | Weight: 3,005 g | Urine 3MCGA | Day 2: elevated liver enzymes and coagulopathy with ALF | |
| Hispanic | Length: 50.8 cm | Week 1: brain MRI with subtle bilateral cerebral white matter signal abnormality and slight broadening/undersulcation of the frontal lobe gyri | ||
| d. 13 mo | APGAR: 9/10 | Week 3: severe obstructive sleep apnea with associated hypoxemia and oxygen at night; coagulopathy normalized; home with palliative care avoidance of surgery or anesthesia | ||
| Genetic variant: c.260del (p.Gly87Alafs*3) | Month 9: all oral feeds, developmental delays | |||
| Died at 13 months | ||||
| 4 (Family 2) | Gestation: 40 weeks | Day 3: hypoglycemia, ALF | Day 3: low glucose 29 (47-110 mg/dL); ALT 742 (5-110 u/L); AST 365 (5-55 u/L); ALP 653 (117-270 u/L); AFP 50,480 (150-15,000 ng/mL); GGT 445 (10-270 u/L); total Bili 18.5 (0.1-10.3 mg/dL); direct Bili 2.2 (0.0-0.4 mg/dL); ammonia 67 (<50 µmol/L); lactic acid 6 (1.5-2.0 mmol/L); PT ratio: 23% (70%-100%); factor V 27 (50-150%) | Month 6: mild elevation of liver enzymes with normal coagulation profile, mild cholestasis, mild hypotonia; microcephaly (–2 SDs) |
| Male | Weight: 2,840 g | Day 6: ALT 120; AST 76; ALP 802; GGT 276; total Bili 7.5; direct Bili 3.5; lactic acid 1.2; normal PT and factor V | Month 9: respiratory insufficiency and ARDS | |
| Tunisian | Length: 47 cm | Month 9: ALT 52; AST 122; ALP 391; GGT 317; normal Bili, PT, and factor V | Died at 10 months from ARDS | |
| d. 10 mo | Urine 3MCGA | |||
| Genetic variant: c.143dupT (p.Ala51Argfs*32) | ||||
| HC: 35 cm | ||||
| APGAR: 10/10 | ||||
| 5 (Family 2) | Gestation: 40 weeks | Month 1.5: cyanosis | 1.5 mo: ALT 109 (5-110 u/L); AST 190 (5-55 u/L); ALP 630 (117-270 u/L); GGT 237 (10-270 u/L); normal total Bili; PT ratio 100% (70%-100%) | Month 2: respiratory distress and hepatomegaly |
| Female | Weight: 2,820 g | Month 2: ALT 152; AST 165; ALP 458; GGT 297; AFP 1,990 (150-15,000 ng/mL) | Month 4: feeding difficulty with psychomotor regression and microcephaly (HC –2 SDs); breathing difficulties leading to ARDS | |
| Tunisian | Length: 46.5 cm | Month 4: ALT 147 IU/L; AST 78 IU/L; GGT 490 IU/L; ALP 433 IU/L; lactic acid 2-4 (1.5-2.0 mmol/L); no lactaturia; CSF lactate 2.2 (<2 mmol/L); PT ratio 100% | Died at 5 months from ARDS | |
| d. 5 mo | HC: 34 cm | Urine 3MCGA | ||
| Genetic variant: c.143dupT (p.Ala51Argfs*32) | APGAR: 10/10 | |||
| 6 (Family 2) | Gestation: 39 weeks | Month 8: psychomotor regression, microcephaly | Month 8: ALT 537 (5-110 u/L); AST 418 (5-55 u/L); ALP 760 (117-270 u/L); total Bili 3.5 (0.1-10.3 mg/dL); direct Bili 1.8 (0.0-0.4 mg/dL); lactic acid 2 (1.5-2.0 mmol/L); CSF lactate 2.5 (<2 mmol/L); PT ratio 100% (70%-100%) | Month 8: psychomotor regression, microcephaly at –2.5 SDs, optic atrophy, white matter changes, and cerebellar atrophy; muscle biopsy showed lipidosis, mitochondrial aggregates, and respiratory chain complexes (II + III) and intravenous deficiencies; in liver: deficiency of respiratory chain complexes (II + III) |
| Female | Weight: 3,270 g | Urine 3MCGA | Died at 9.5 months of age from respiratory distress | |
| Tunisian | APGAR: 10/10 | |||
| d. 9.5 mo | ||||
| Genetic variant: c.143dupT (p.Ala51Argfs*32) | ||||
| 7 (Family 3) | Gestation: 41 weeks | Day 1.5: liver failure, hypotonia | Day 1.5: glucose very low; liver enzymes not done; AFP 20,000-50,000 (150-15,000 ng/mL); lactic acid 5 (1.5-2.0 mmol/L); PT ratio 29% (70%-100%); factor V 28% (50%-150%) | Day 10: liver biopsy with multiple respiratory chain complexes deficiency and mtDNA depletion |
| Female | Weight: 3,440 g | Day 10: ALT 30 (5-110 u/L); AST 88 (5-55 u/L); GGT 237 (10-270 u/L); ALP 392 (117-270 u/L); total Bili 4.6 (0-15 mg/dL); direct Bili 2.3 (0.0-0.7 mg/dL); lactic acid 5 mmol/L; ammonia 10 (<50 µmol/L); PT ratio 80%; factor V 183% | Month 2: psychomotor delay with cerebellar and optic atrophy on brain MRI | |
| Tunisian | Length: 52 cm | 2 yo 10 mo: ALT 1,440; AST 999; GGT 85; PT ratio 50%; factor V 66%; no metabolic acidosis | Intermittent liver failure when febrile | |
| d. 3 yo | HC: 35 cm | Urine 3MCGA | 2 years 10 months: fever, vomiting, neurological deterioration, and associated seizures | |
| Genetic variant: c.143dupT (p.Ala51Argfs*32) | APGAR: 10/10 | Died at age 3 from severe neurological deterioration and liver disease |
- All families are of consanguinous descent. The proband in each familiy was identified on exome sequencing or mitochondrial nuclear gene panel by next-generation sequencing (patients 4-6) with Sanger confirmation for the proband and all affected relatives.
- Abbreviations: AFP, alpha-fetoprotein; ALP, alkaline phosphatase; ALT, alanine aminotransferase; APGAR, Appearance, Pulse, Grimace, Activity, and Respiration; AST, aspartate aminotransferase; CSF, cerebrospinal fluid; d., died; direct Bili, direct bilirubin; HC, head circumference; INR, international normalized ratio; mo, months; MRI, magnetic resonance imaging; mtDNA, mitochondrial DNA; NICU, neonatal intensive care unit; OR, operating room; PT, prothrombin; total Bili, total bilirubin; yo, years old.
Discussion
Extrahepatic manifestation of QIL1 hepato-encephalopathy varies, but all 7 patients had liver disease with acute liver failure (ALF) in all but 2 patients (5 and 6). In patients 1 and 2, ALF initially appeared to be isolated prompting evaluation for liver transplantation. However, given the high rate of neurological deterioration, mitochondrial hepatopathy attributed to QIL1 ought to be a contraindication for transplantation. Whereas liver disease was the entry point in all patients, its characteristics and severity varied even within the same family. Patients 3, 4, and 7 exhibited neonatal-onset ALF. At presentation, cholestatic jaundice was present in all but 1 patient (patient 5), and gamma-glutamyl transferase (GGT) was normal in 4 patients (1, 2, 5, and 7) and elevated in the other 3. Ammonia was normal or mildly elevated. Lactic acid ranged from 2.7 to 8.6 mmol/L. All patients exhibited urinary excretion of 3MCGA. Therefore, a consistent QIL1 clinical scenario is of early onset and recurrent liver disease of variable severity, most often with cholestatic jaundice and elevated or normal GGT. In that setting, subsequent extrahepatic findings (neurological disease, optic atrophy, and ARDS) and 3MCGA are highly suggestive of QIL1.
For patients 1 and 2, anesthesia exposure likely contributed to their decline given that their sister survived 13 months without anesthesia. ARDS was striking (patients 4 and 5), along with respiratory failure in the literature.3 This may reflect poor brainstem function with aspiration or be part of the QIL1 phenotype given that QIL1 is expressed in lung tissue.4
Characteristic findings on liver EM helps to differentiate this condition. The stacking dysmorphia of the mitochondrial cristae may allow one to distinguish QIL1-related pathology from other metabolic or mitochondrial (mitochondrial DNA depletion syndromes) conditions. However, EM findings vary in different cell types and can be subtle. Although it is not always routine to attain biopsies, multiple images of muscle and liver tissue should be evaluated when attained.
Ultimately, whole-exome sequencing or next-generation sequencing mitochondrial panel (patients 4-6) identified the causative variants in all three families. Because there are only 5 reported cases, QIL1 is not yet on infantile liver failure gene panels. Based on the clinical and management implications of an early diagnosis, we propose that the evaluation of an infant with ALF should include broader genetic testing, especially in the setting of transplant evaluation.




