Pentraxin-3 modulates lipopolysaccharide-induced inflammatory response and attenuates liver injury
Potential conflict of interest: Nothing to report.
Supported by grants from Fondo de Investigación Sanitaria Carlos III, cofinanced by Fondo Europeo de Desarrollo Regional, Unión Europea, “Una manera de hacer Europa” (FIS PI14/00320, PI12/00330, and FIS PI12/01265, to P.S.-B., P.G., and J.C.); the National Institute on Alcohol Abuse and Alcoholism (1U01AA020821 and 1U01AA021908-01-33490); Instituto de Salud Carlos III, Miguel Servet, cofinanced by Fondo Europeo de Desarrollo Europeo, Unión Europea, “Una manera de hacer Europa” (CP11/00071, to P.S.-B.); Agencia de Gestió d'Ajuts Universitaris I de Recerca (2014 SGR 708), Centro de Investigación en Red Enfermedades Hepaticas y Digestivas (CIBEReHD) and Institució Catalana de Recerca i Estudis Avançats (to P.G.); Instituto de Salud Carlos III (Sara Borrell, to M.C.; Rio Hortega, to I.G.; and Miguel Servet CPII 14/00021, to M.R.S.); Fundació Marató de TV3 (2013-3610, to M.C., I.G., and M.R.S.); CONACyT (Mexico City, Mexico, to J.A.); and Ministerio de Educación, Cultura y Deporte, FPU Program (to B.A. and D.R.-T.).
Abstract
Acute-on-chronic liver injury is characterized by an important inflammatory response frequently associated with endotoxemia. In this context, acute-phase proteins such as Pentraxin-3 (PTX3) are released; however, little is known about their role in chronic liver disease. The aim of this study was to elucidate the role of PTX3 in liver injury. The role of PTX3 was evaluated in cultured human cells, liver tissue slices, and mice with acute-on-chronic liver injury. PTX3 expression was assessed in tissue and serum samples from 54 patients with alcoholic hepatitis. PTX3 expression was up-regulated in animal models of liver injury and strongly induced by lipopolysaccharide (LPS). Liver cell fractionation showed that macrophages and activated hepatic stellate cells were the main cell types expressing PTX3 in liver injury. Ex vivo and in vivo studies showed that PTX3 treatment attenuated LPS-induced liver injury, inflammation, and cell recruitment. Mechanistically, PTX3 mediated the hepatic stellate cell wound-healing response. Moreover, PTX3 modulated LPS-induced inflammation in human primary liver macrophages and peripheral monocytes by enhancing a TIR domain–containing adapter-inducing interferon–dependent response and favoring a macrophage interleukin-10-like phenotype. Additionally, hepatic and plasma PTX3 levels were increased in patients with alcoholic hepatitis, a prototypic acute-on-chronic condition; and its expression correlated with disease severity scores, endotoxemia, infections, and short-term mortality, thus suggesting that expression of PTX3 found in patients could be a counterregulatory response to injury. Conclusion: Experimental and human evidence suggests that, in addition to being a potential biomarker for alcoholic hepatitis, PTX3 participates in the wound-healing response and attenuates LPS-induced liver injury and inflammation; therefore, administration of PTX3 could be a promising therapeutic strategy in acute-on-chronic conditions, particularly those associated with endotoxemia. (Hepatology 2017;66:953–968).
Abbreviations
-
- ABIC
-
- age, serum bilirubin, international ratio, and serum creatinine
-
- AH
-
- alcoholic hepatitis
-
- CD14
-
- cluster of differentiation 14
-
- CCL20
-
- chemokine (C-C motif) ligand 20
-
- FcγR
-
- Fc gamma receptor
-
- HSC
-
- hepatic stellate cell
-
- IL
-
- interleukin
-
- LDH
-
- lactate dehydrogenase
-
- LPS
-
- lipopolysaccharide
-
- MD2
-
- myeloid differentiation factor 2
-
- MELD
-
- Model for End-Stage Liver Disease
-
- PTX3
-
- pentraxin-3
-
- rPTX3
-
- recombinant PTX3
-
- siRNA
-
- small interfering RNA
-
- TLR4
-
- toll-like receptor 4
-
- TNF-α
-
- tumor necrosis factor alpha
-
- TRIF
-
- TIR domain–containing adapter-inducing interferon
Chronic liver diseases are characterized by a persistent inflammatory response as well as a progressive wound-healing process that usually lead to fibrosis.1 Advanced liver diseases are associated with increased gut permeability, leading to increased endotoxemia and lipopolysaccharide (LPS) levels in serum.2-4 Moreover, patients with advanced diseases are prone to developing acute events of inflammation and infections,5 which are the main causes of the development of acute-on-chronic liver failure.6, 7 One of the triggers of acute-on-chronic liver failure is alcoholic hepatitis (AH), which is characterized by an important inflammatory response, hepatocellular injury, and liver failure and is frequently associated with increased endotoxemia.
By binding to LPS, toll-like receptor (TLR) 4 is one of the main receptors driving the inflammatory response.8, 9 The TLR4 response to LPS is dependent on accessory proteins, among them myeloid differentiation factor 2 (MD2) and cluster of differentiation 14 (CD14).10 TLR4 downstream signaling and cytokine production are mainly governed by myeloid differentiation primary response 88,11 with early activation of nuclear factor κB and production of proinflammatory cytokines,12 and TIR domain–containing adapter-inducing interferon (TRIF), essential for late activation of nuclear factor κB, interferon regulatory factor 3, and production of interferon-inducible genes.9, 12, 13 Activation of TLR4 has been shown to enhance cytokine production, macrophage polarization,14 inflammatory cell recruitment, and hepatic stellate cell (HSC) activation.15
Pentraxin-3 (PTX3) is a member of the humoral arm of innate immunity and is involved in the modulation of inflammation and tissue remodeling.16 Moreover, PTX3 can also act in response to pathogens by acting as a soluble pattern-recognition receptor16 or binding to pathogens.16-19 PTX3 is the long member of the pentraxin family together with C-reactive protein and the serum amyloid P component.20, 21 Short components of this family are mainly produced by hepatocytes in response to inflammation and act as acute-phase response proteins. Conversely, PTX3 is broadly expressed and can be produced in different organs after injury, infection, or inflammation, mainly by mesenchymal and inflammatory cells.20, 21
PTX3 exerts its pleiotropic functions through interaction with a variety of soluble ligands; however, although PTX3 can interact with Fc receptors, no specific receptors have been identified.19, 22 PTX3 was shown to be protective in models of tissue injury mediated by infection, increased LPS, as well as sterile inflammation.23-28 Recently, the role of PTX3 in tissue repair and remodeling was reported.29 PTX3 deficiency was found to be associated with dysfunctional tissue repair and with increased collagen deposition and scar formation in liver and other organs.29 In the context of liver diseases, circulating levels of PTX3 were found to be elevated in nonalcoholic steatohepatitis and associated with disease progression.30, 31 However, the expression and role of PTX3 in liver injury and in response to inflammation are not well understood.
In this study we show that PTX3 expression and serum levels are strongly associated with liver disease progression and endotoxemia. PTX3 is locally produced by activated HSCs in chronic liver injury, and administration of PTX3 attenuated LPS-induced liver injury and inflammation by modulating cytokine production induced by TLR4 activation.
Materials and Methods
PATIENTS
Samples from 54 patients with clinical, analytical, and histological features of AH were selected. These cases are part of our historic cohort of patients with AH and controls with cirrhosis admitted to the Liver Unit of the Hospital Clinic of Barcelona from July 2009 to January 2015. The study was approved by the Ethics Committee of the Hospital Clinic of Barcelona, and informed consent was obtained from all patients before inclusion. Inclusion and exclusion criteria have been described.4
IN VITRO STUDIES
Human primary HSCs were isolated from control patients and cultured as described.32 For gene expression analysis by quantitative PCR, total RNA was isolated using the RNeasy Mini Kit (Qiagen) per the manufacturer's protocol.
EFFECT OF PTX3 IN HUMAN MONOCYTE INFLAMMATORY RESPONSES AND POLARIZATION
Buffy coats, provided by the Blood and Tissue Bank (Barcelona, Spain), were obtained from healthy blood donors following the institutional standard operating procedures for blood donation and processing. Peripheral blood mononuclear cells were isolated from donors as described.33 The percentage of CD14+ cells (peripheral blood monocytes) routinely obtained was 5% (±3%).
EXPERIMENTAL MOUSE MODELS OF LIVER DAMAGE
Experimental models were performed using male C57BL/6 mice 6-12 weeks old (Charles River, l'Arbresle, France). All animal studies were approved by the Ethics Committee of the University of Barcelona. To induce chronic liver injury, mice were treated with CCl4 injected intraperitoneally at a dose of 0.5 mL/kg twice a week; control mice were injected with corn oil. In order to study the effects of acute-on-chronic liver injury, we performed a model combining the damage of chronic CCl4 with administration of LPS (Sigma-Aldrich), mimicking the outcome of endotoxemia in the situation of chronic liver disease.34
The role of PTX3 during acute-on-chronic liver injury was investigated in vivo in chronic CCl4 (0.5 mL/kg twice a week for 2 weeks)–treated mice. Intraperitoneal administration of recombinant PTX3 (rPTX3; 5 mg/kg body weight) was performed 2 hours before intravenous injection of LPS (2.5 mg/kg); control mice were injected intraperitoneally with corn oil and intravenously with vehicle. Mice were sacrificed 24 hours after LPS injection, and blood, livers, lungs, and kidneys were removed for subsequent analysis.
See the Supporting Information for more details.
Results
PTX3 EXPRESSION IS INCREASED IN EXPERIMENTAL MODELS OF CHRONIC AND ACUTE-ON-CHRONIC LIVER INJURY
PTX3 is rapidly induced after injury in several tissues; therefore, we evaluated the expression of PTX3 in animal models of chronic liver disease and acute-on-chronic liver injury. Administration of CCl4 to mice, a well-established animal model of chronic liver injury and fibrosis, induced a time-dependent increase in PTX3 liver expression (Fig. 1A). Liver cirrhosis is frequently associated with increased gut permeability and endotoxemia with elevated circulating levels of LPS.2, 3 Therefore, we evaluated the effect of LPS administration on PTX3 expression. Interestingly, while the administration of LPS to healthy animals did not induce PTX3 expression (Fig. 1B), LPS infusion in CCl4-treated animals, a model of acute-on-chronic liver injury, induced a marked increase in hepatic PTX3 expression (Fig. 1C). Interestingly, Tlr4 hepatic expression was increased in CCl4-treated animals but not further increased by LPS stimulation (Supporting Fig. S1). These results suggest that preexisting liver injury may be necessary to mediate LPS-induced PTX3 expression.
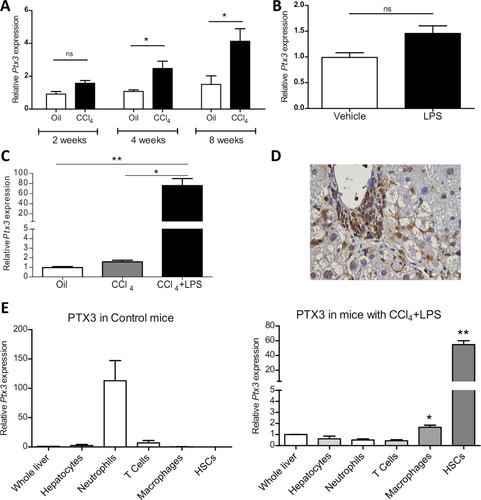
In order to elucidate the cell source of PTX3 in chronic liver injury, we evaluated PTX3 expression by immunohistochemistry. PTX3 expression in mice with CCl4-induced chronic liver injury plus LPS was mainly localized at inflammatory areas and sinusoidal cells (Fig. 1D). Furthermore, we assessed Ptx3 gene expression in different liver cell sorted populations, namely hepatocytes, HSCs, macrophages, neutrophils, and T cells isolated from healthy mice and those with acute-on-chronic liver injury. Interestingly, while the main producing cell type in healthy livers was neutrophils, macrophages and particularly HSCs were the main cell types expressing PTX3 in injured livers (Fig. 1E). In order to evaluate the purity of sorted populations, we evaluated the gene expression of Alb, Mpo, Cd3e, F4/80, and Col1a1 in each of the populations obtained, which showed high enrichment (Supporting Fig. S2).
PTX3 ENHANCES HSC ACTIVATION AND IS EXPRESSED IN ACTIVATED HSCs
HSCs are the main cell type producing PTX3 in mouse models of liver injury. Therefore, we assessed the expression and effects of PTX3 in human HSCs, the main cell type responsible for the wound-healing response of the liver.35 We first evaluated the expression of PTX3 in human quiescent HSCs freshly isolated from normal livers, followed by their activation in culture. Upon culture activation, HSCs strongly increased the expression of PTX3 compared to quiescent HSCs (Fig. 2A). Moreover, proinflammatory mediators such as tumor necrosis factor alpha (TNF-α), interleukin 1β (IL-1β), and LPS enhanced PTX3 expression in human primary activated HSCs compared to vehicle (P < 0.05) (Fig. 2B).
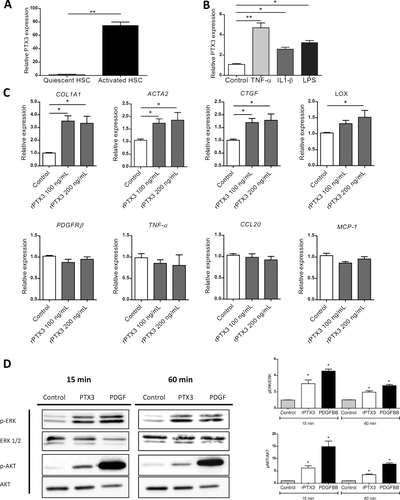
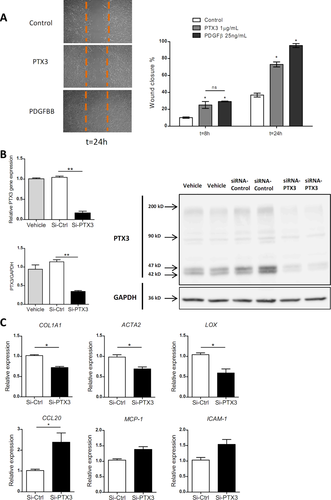
Stimulation of human primary activated HSCs with rPTX3 induced an up-regulation of HSC activation marker and extracellular matrix genes (COL1A1, ACTA2, CTGF, LOX) (Fig. 2C) but did not significantly change the expression of proinflammatory genes (TNF-α, chemokine [C-C motif] ligand 20 [CCL20], MCP-1) (Fig. 2C). Moreover, rPTX3 induced extracellular signal–regulated kinase 1/2 and AKT phosphorylation in HSCs, suggesting that PTX3 induces intracellular signaling in HSCs (Fig. 2D). To further investigate the biological effect of PTX3 on HSCs, we performed a wound-healing assay with primary HSCs. As a positive control, cells were stimulated with platelet-derived growth factor subunit B, a main mitogen for HSCs. Incubation with rPTX3 increased HSC migration and wound closure (Fig. 3A). Next, we evaluated the effects of silencing PTX3 in the LX2 human HSC cell line by small interfering RNA (siRNA). Transfection of HSCs with an siRNA targeting PTX3 reduced PTX3 mRNA and protein expression compared to scramble siRNA (Fig. 3B). HSCs treated with PTX3 siRNA significantly reduced the expression of activation genes such as COL1A1, ACTA2, and LOX but did not reduce the expression of inflammatory mediators (Fig. 3C). Results from recombinant PTX3 stimulation and silencing of endogenous PTX3 expression suggest that both exogenous as well as endogenous PTX3 induce HSC activation. In order to elucidate if PTX3 might exert its role on HSCs through Fc gamma receptors (FcγRs), we investigated their expression in primary human HSCs. Gene expression of FcγR-1 and FcγR-2 was not detected in cultured HSCs. Expression of FcγR-3, the FcγR with the highest affinity for PTX3,22 was assessed by flow cytometry, with no expression shown in cultured HSCs (Supporting Fig. S3A). Taken together, these results indicate that PTX3 is expressed in HSCs and involved in their activation, reinforcing its potential role in the liver wound-healing response.
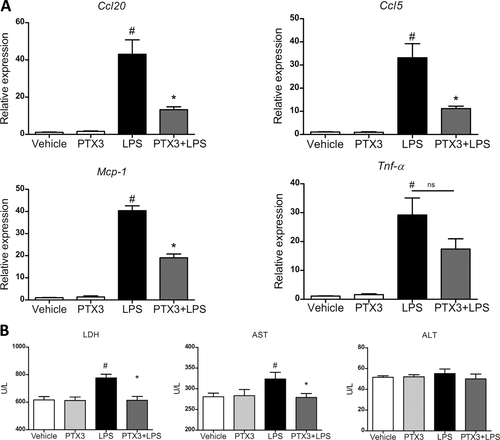
PTX3 MODULATES LPS-INDUCED LIVER INJURY AND INFLAMMATION
PTX3 was highly expressed in LPS-induced acute-on-chronic liver injury. Therefore, we explored the potential role of PTX3 in LPS-induced inflammation in the context of chronic injury. First, we evaluated the effect of PTX3 in high precision-cut liver slices from mice treated with CCl4. Liver slices were incubated in the presence or absence of rPTX3 and stimulated with LPS. rPTX3 alone did not induce any significant effect; however, incubation with rPTX3 was able to attenuate the expression of inflammatory mediators such as Ccl20, Ccl5, and Mcp-1 induced by LPS (Fig. 4A). Moreover, incubation with rPTX3 also reduced lactate dehydrogenase (LDH) and aspartate aminotransferase levels in tissue culture supernatant (Fig. 4B). Taken together, these results suggest that PTX3 may protect against LPS-induced liver damage by attenuating the expression of proinflammatory cytokines and hepatocellular damage.
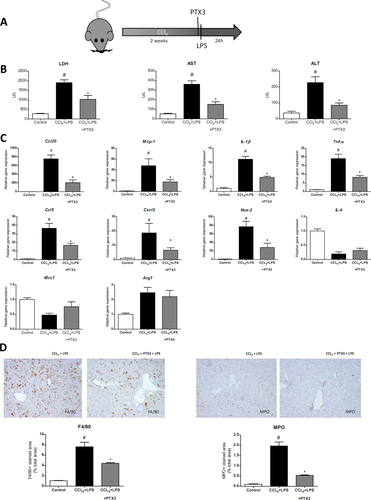
Next we evaluated the role of PTX3 in vivo in an acute-on-chronic hepatic injury model of CCl4-induced liver injury plus LPS (Fig. 5A). Treatment with rPTX3 before LPS stimulation substantially reduced liver damage as assessed by LDH, aspartate aminotransferase, and alanine aminotransferase serum levels (Fig. 5B). In addition, PTX3 treatment reduced the inflammatory response by down-regulating Ccl20, Mcp-1, Ccl5, IL-1β, Tnf-α, Cxcl2, and Nos-2 gene expression (Fig. 5C). Moreover, macrophage M1 inflammatory mediators (i.e., Mcp-1, IL-1β, Tnf-α) but not M2 markers (Mrc1, Arg1, and IL-4) were reduced in PTX3-treated animals (Fig. 5C). Moreover, histological evaluation showed a significant reduction of neutrophil and macrophage liver infiltration in mice treated with rPTX3 (Fig. 5D). This reduction in recruitment was not associated with changes in Fcγ receptor expression between experimental groups (Supporting Fig. S3B). It is important to note that chronic liver injury and endotoxemia are associated with extrahepatic organ injury.6 In this regard, rPTX3 administration significantly reduced the expression of LPS-induced inflammatory mediators and neutrophil infiltration in the kidney and the lung (Supporting Fig. S4A-C). Together, the results from ex vivo and in vivo experiments suggest that PTX3 administration exerts a hepatoprotective effect and modulates LPS-induced liver injury and inflammation.
PTX3 REGULATES INFLAMMATION BY TARGETING MONOCYTES AND LIVER MACROPHAGES
Our data suggest that PTX3 is able to attenuate inflammatory responses to LPS in liver as well as the inflammatory cell infiltrate. However, because no direct anti-inflammatory effect was observed on HSCs, we analyzed whether PTX3 could be targeting macrophages. First, we evaluated whether PTX3 was able to block the TLR4-LPS response in peripheral blood monocytes isolated from healthy donors. Interestingly, while rPTX3 clearly reduced the early response to LPS by decreasing TNF-α and IL-1β production, it increased the production of CCL5 (Fig. 6A). Second, we evaluated the effect of rPTX3 in human liver macrophages. As shown in monocytes, stimulation of liver macrophages with rPTX3 reduced LPS-induced TNF-α and IL-1β secretion in cell culture media and induced a marked increase in CCL5 production (Fig. 6B). It has been shown that in macrophages PTX3 modulates the inflammatory response to infection by Aspergillus conidia by binding to MD2, the TLR4 accessory protein.26 We therefore studied the ability of PTX3 to interfere with MD2 activity in a widely used cellular system. We transfected human embryonic kidney (HEK-293) cells stably expressing TLR4 or TLR4 plus CD14 with MD2. rPTX3 did not significantly affect the LPS response in TLR4 and TLR4/CD14 human embryonic kidney cells transfected with MD2, suggesting that in this system PTX3 may not prevent an MD2 contribution to LPS activation through TLR4 and TLR4–CD14 complexes (Supporting Fig. S5).
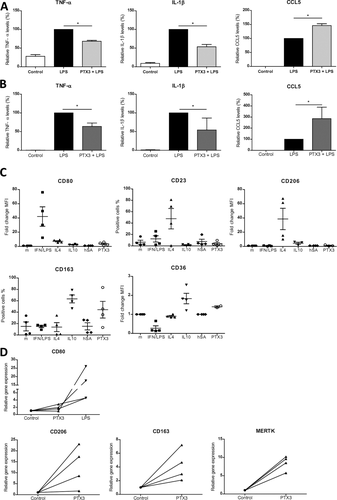
Next, we evaluated whether PTX3 influenced the polarization of monocytes into macrophages. As control stimuli, we treated macrophages with interferon/LPS to induce an M1 phenotype (CD80-positive); IL-4 (M-IL-4) to induce an M2a phenotype (CD2-positive and CD206-positive); and IL-10 (M-IL-10) to induce M2c (CD163-positive and CD36-positive).36 As observed by comparison with all the different stimulations, rPTX3 modulated the expression of polarization markers in a similar way as IL-10: it induced an increase in CD163 and CD36 expression, suggesting that it may enhance the acquisition of an IL-10-like macrophage phenotype. Conversely, the use of human albumin as a negative control protein did not substantially alter the macrophage phenotype (Fig. 6C). Moreover, we also evaluated the potential of PTX3 to induce M2 phenotype in liver macrophages. Human liver macrophages stimulated with rPTX3 showed an increase in expression of M2 markers CD206, CD163, and Mertk and did not induce M1 marker CD80 (Fig. 6D).
Taken together, these results suggest that PTX3 may modulate the LPS signaling response in monocytes and liver macrophages.
PTX3 IS UP-REGULATED IN PATIENTS WITH ACUTE-ON-CHRONIC LIVER DISEASE AND ASSOCIATED WITH DISEASE SEVERITY
AH is an acute-on-chronic condition characterized by liver injury, fibrosis, and important inflammatory responses, in which endotoxemia is associated with a bad outcome.2, 3 Therefore, PTX3 liver expression and plasma levels were evaluated in patients with alcoholic cirrhosis and AH.
PTX3 gene expression was increased in liver tissue from alcoholic patients with cirrhosis and strongly up-regulated in AH patients (P < 0.01) (Fig. 7A), consistent with PTX3 expression in experimental models of liver injury (Fig. 1A,B).37, 38 Plasma levels of PTX3 were also increased in compensated alcoholic patients with cirrhosis and further increased in patients with both mild and severe AH (Fig. 7B). Interestingly, PTX3 hepatic gene expression and peripheral plasma levels showed a positive correlation, suggesting that the liver may be an important source of circulating PTX3 (Fig. 7C). PTX3 staining in alcoholic cirrhosis was localized in septal areas with fibrosis and inflammation (Fig. 7D). We next assessed the association of PTX3 plasma levels with clinical parameters and scores of disease severity. We found a positive correlation of PTX3 plasma levels with the Model for End-Stage Liver Disease (MELD) (P < 0.001) and age, serum bilirubin, international normalized ratio, and serum creatinine (ABIC) scores (P < 0.01) (Fig. 7E). Moreover, PTX3 plasma levels positively correlated with Maddrey score (P < 0.01) and procalcitonin but not with ultrasensitive C-reactive protein serum levels and the hepatic venous pressure gradient. Importantly, PTX3 plasma levels correlated with LPS serum levels (Fig. 7F), indicating a potential association of PTX3 expression with endotoxemia. However, PTX3 plasma levels did not correlate with IL-10, suggesting that PTX3 may not be associated with IL-10 expression and immune exhaustion (Supporting Fig. S6C). Additionally, PTX3 levels were higher in patients with infection at admission and in those who developed in-hospital infections compared to noninfected patients (Supporting Fig. S6B). Next, we evaluated the association of PTX3 plasma level with 6-month mortality. PTX3 serum levels showed an area under the receiver operating characteristic curve of 0.76 (95% confidence interval 0.69-0.89; P = 0.002) for predicting 6-month mortality. The Kaplan-Meier analysis showed that PTX3 levels >10 ng/mL were associated with a higher mortality at 180 days (Fig. 7G). This cutoff showed a sensitivity of 78% and a specificity of 60%. Finally, to evaluate the potential prognostic impact of PTX3 on 180-day mortality, we fitted a bivariate Cox regression (hazard ratio) analysis, adjusting PTX3 plasma levels for AH severity-scoring systems at admission (e.g., ABIC score, MELD, and Lille model). PTX3 plasma levels were independently associated with 180-day mortality after adjusting for the well-validated scoring systems (P < 0.05 for all cases; Supporting Table S2).
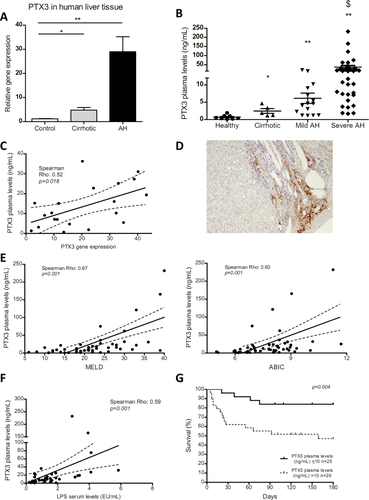
These results suggest that PTX3 is strongly associated with disease severity, and its expression may be enhanced as a result of acute-on-chronic liver injury and endotoxemia.
Discussion
In this study, we show that PTX3 is highly up-regulated in chronic liver diseases and particularly in acute-on-chronic conditions such as AH, in which it correlates with disease severity, adverse outcome, and endotoxemia. We have identified activated HSCs as the main cell source of PTX3 in chronic liver disease. Moreover, PTX3 exerts a positive loop on HSCs, enhancing HSC activation and thereby promoting PTX3 synthesis. Interestingly, besides its effects on the wound-healing response, we show that PTX3 reduces LPS-induced acute-on-chronic tissue injury and inflammatory cell recruitment. Moreover, PTX3 has a modulatory effect on liver inflammation and particularly on LPS-induced responses.
Although there was a clear positive correlation of PTX3 with disease progression, our in vitro, ex vivo, and in vivo data suggest that PTX3 exerts a hepatoprotective and a modulatory effect on acute-on-chronic inflammatory events, taking into account that PTX3 protein and regulation are conserved between mice and humans.37, 38 This apparently contradictory result suggests that PTX3 might be expressed as a local response to injury and infection by modulating an exacerbated inflammatory response. Moreover, high PTX3 levels in patients could be a counterregulatory response to disease severity. In the context of chronic liver injury, the level of PTX3 expression may be determined by injury, inflammation, and endotoxemia. Additionally, PTX3 levels were associated with infection. Although interesting, this latter result should be taken with caution because the number of patients is low and significance is likely mainly due to the small number of patients with very high plasma levels of PTX3. The current data suggest that PTX3 plasma levels may have potential as a prognostic biomarker in AH patients. However, future studies with larger cohorts of patients should specifically evaluate the potential of PTX3 as a biomarker for chronic liver diseases.
Interestingly, in patients with AH, there was a good correlation between liver expression and circulating levels of PTX3, suggesting that the liver may be the main source of PTX3 in chronic liver diseases. Although PTX3 production and release are local at the site of injury, PTX3 is secreted and detected in the circulation, suggesting that it may exert its effects at a systemic level. Indeed, from our therapeutic approach in which PTX3 was administered systemically, we could detect its effects in the liver but also in the lungs and kidneys. This is an important finding for the potential use of PTX3 administration as a therapeutic intervention because in acute-on-chronic conditions extrahepatic organs are frequently affected. Moreover, infections and endotoxemia are the main cause of acute-on-chronic liver failure, a syndrome recently associated with multiorgan failure and high mortality.6
PTX3 has been reported to participate in the wound-healing response in different organs, including the liver.29 In this regard, we showed that while PTX3 is mainly expressed in neutrophils in healthy liver, in injury it is mainly expressed in HSCs, the main cell type responsible for the liver wound-healing response and liver fibrosis.35 Human HSCs do not express the main receptors identified for PTX3. This is not surprising because the existence of potential PTX3 receptors has been extensively investigated in other cell types with little success. It has been proposed that unidentified receptors for PTX3 may exist; however, most reports suggest that PTX3 exerts its biological functions by indirect binding to other proteins such as TSG-6, fibroblast growth factor 2, C1q, Ficolin-1, and inter-α-trypsin inhibitor and not by direct interaction with a specific receptor.39-44 Besides the role of HSCs in the production of extracellular matrix components for the wound-healing response, HSCs are important players in the inflammatory response of the liver, mainly by promoting inflammatory cell recruitment and expression of inflammatory mediators. Although PTX3 does not modulate inflammatory gene expression in HSCs, the important expression of PTX3 by activated HSCs suggests that it may have paracrine effects to modulate liver inflammation and to control inflammatory responses in the liver. The differential expression of PTX3 in healthy and injured liver together with the data that show that PTX3 drives HSC activation suggest that in response to injury PTX3 released by neutrophils may promote HSC activation. However, in chronic liver disease, activated HSCs would become the main cell type producing PTX3, which may enhance the wound-healing response and exert protective and immune modulatory effects. Neutrophils serve as a reservoir of PTX3 for a rapid release in response to microbial or inflammatory signals, when PTX3 acts as an acute-phase protein.45 Once neutrophils activate, they stop or reduce PTX3 production. During injury, different cell types may also contribute to PTX3 production.46 In this study we describe that HSCs express PTX3 during activation and in response to injury and inflammatory signals. One of the transcription factors that regulate the constitutive expression of PTX3 is activator protein 1,47 but no information is available regarding the regulation of PTX3 expression in liver injury. Further studies will need to address the regulation of PTX3 in HSCs.
Our data together with previous reports showing the role of PTX3 in tissue repair29 suggest that PTX3 expression may be associated not only with fibrogenesis but also with a correct tissue wound-healing response and modulation of inflammation. Further studies would have to determine the potential beneficial effects of long-term PTX3 treatment in chronic liver diseases and fibrogenesis.
Acute administration of PTX3 has a clear protective effect on hepatocellular injury as well as inflammatory response. The well-known pleiotropic nature of PTX3 suggests that it may exert this complex protective effect by a combination of mechanisms. In other organs it is reported that PTX3 binds to p-selectin, preventing inflammatory cell recruitment and thereby attenuating the inflammatory response.43 In addition, it is known that PTX3 opsonizes apoptotic cells and contributes to their clearance, preventing autoimmune reactions in inflamed tissues.18, 39, 48 Therefore, in the context of liver injury, PTX3 reduces the inflammatory response by reducing inflammatory cell infiltration and potentially by directly targeting inflammatory cells, modulating their phenotype and response. Notably, in this study we identified an unrecognized novel mechanism of action of PTX3 that may be of critical relevance in the context of chronic liver disease. We found that PTX3 modulates TLR4 downstream responses, reducing myeloid differentiation primary response 88–dependent cytokines (TNF-α and IL-1β)12 and enhancing the production of TRIF-dependent CCL512 in human monocytes and in liver macrophages. This is in agreement with a previous report that PTX3 binds to MD2 and needs TRIF to promote TRIF-dependent protection in aspergillosis.26 Moreover, our data suggest that PTX3 favors the acquisition of an anti-inflammatory IL-10-like phenotype in human monocyte-derived macrophages and expression of M2 markers in isolated liver macrophages. These results suggest that PTX3 may target peripheral monocytes and liver macrophages, modulating the inflammatory response and macrophage differentiation and polarization. Although we show a clear effect of PTX3 on macrophages, we cannot conclude that the PTX3 effect on macrophages is the only or the main mechanism conferring hepatoprotection. Altogether, these results suggest that the effects observed for PTX3 are certainly not exclusively mediated by a single mechanism but rather by a combination of biological roles leading to a hepatoprotective effect and attenuation of inflammatory recruitment and response.
The results of the present study show the liver expression of PTX3 by activated HSCs and the role of PTX3 in liver injury and inflammation. Besides its well-recognized role in bacterial opsonization and clearance, we identified a mechanism of action of PTX3 in the context of LPS-induced liver injury and endotoxemia. Moreover, we describe its immunomodulatory effects in human macrophages in the context of liver injury and disease. These results, together with the human data provided, suggest that PTX3 may be an important local and systemic player in chronic liver disease and that PTX3 administration may be a promising therapeutic strategy in acute-on-chronic liver disease.
Acknowledgment
This work was performed in the Centre Esther Koplowitz. We thank Cristina Millán for her excellent technical support. We are indebted to the Genomics Unit, Biobank Unit, and Cytometry and Cell Sorting Facility of the Institut d'Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS) for their technical help.
REFERENCES
Author names in bold designate shared co-first authorship.