Persisting risk of hepatocellular carcinoma after hepatitis C virus cure monitored by a liver transcriptome signature
Potential conflict of interest: Dr. Finn consults for Bayer, Pfizer, Bristol-Myers Squibb, Novartis, and Eisai. Dr. Ono received grants from Bristol-Myers Squibb.
Supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases (DK099558), the European Union (ERC-2014-AdG-671231HEPCIR), the Irma T. Hirschl Trust, the US Department of Defense (W81XWH-16-1-0363, to Y.H.), and the National Institutes of Health Loan Repayment Program (to G.Y.I.).
Abbreviations
-
- AFP
-
- alpha-fetoprotein
-
- DAA
-
- direct-acting antiviral
-
- HCC
-
- hepatocellular carcinoma
-
- HCV
-
- hepatitis C virus
-
- LT
-
- liver transplantation
-
- MELD
-
- Model for End-stage Liver Disease
-
- SVR
-
- sustained virological response
While direct-acting antivirals (DAAs) for hepatitis C virus (HCV) have substantially improved sustained virologic response (SVR) rates, the risk of developing hepatocellular carcinoma (HCC) persists over a decade.1 HCC incidence will keep rising over the next two decades even with DAAs unless HCV diagnosis and treatment uptake rates are drastically improved.1 HCC risk prediction with clinical risk factors such as older age, liver fibrosis, and metabolic disorders is not accurate enough; and there is still no clinically established strategy of HCC screening in the post-SVR population.1 Applying biannual HCC screening recommended in the guideline to the whole post-SVR population will not be a practically feasible option given the already overburdened HCC screening capability as evidenced by the low rate of use, <15%.1 Post-SVR HCC risk prediction by means of a transcriptome signature-based HCC risk score may address the challenge, as suggested in our recent study.2
Case Presentation
A 63-year-old Caucasian man with chronic HCV genotype 1 cirrhosis (Model for End-stage Liver Disease score [MELD] 8), type 2 diabetes, and hypertension developed three small HCC tumors (7-mm and 11-mm tumors in segment 7 and 19-mm tumor in segment 8). He underwent transcatheter arterial chemoembolization, resulting in a complete radiologic response, and was subsequently listed for liver transplantation (LT) based on MELD exception for HCC (Fig. 1A). The serum alpha-fetoprotein (AFP) level was decreased from 9.8 ng/mL at baseline to 4 ng/mL. He was then regularly followed up with contrast-enhanced computed tomography or magnetic resonance imaging and AFP every 3 months. While on the transplant waiting list, he underwent HCV treatment with ledipasvir 90 mg and sofosbuvir 400 mg daily for 24 weeks and achieved an SVR at the age of 66.
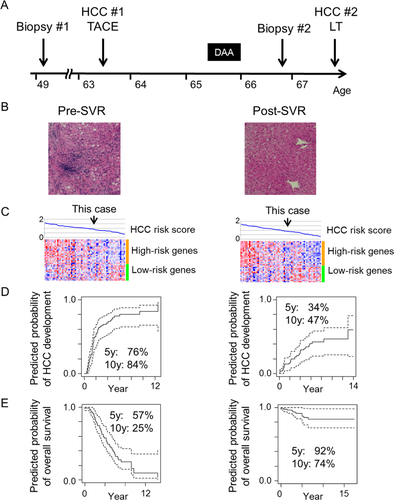
The patient had been hesitant to receive LT due to anticipated complications and well-preserved liver function without any sign of HCC for 3 years and sought to assess his HCC recurrence risk and future need for regular HCC screening and LT by our HCC risk gene signature.2 At the time, there was no evidence of HCC, and the AFP level was consistently <10 ng/mL since the transcatheter arterial chemoembolization. Liver biopsy tissue was obtained and compared with pre-SVR liver tissue. His transaminase levels improved, and synthetic function remained stable after SVR (Table 1). Hematoxylin and eosin staining revealed almost complete regression of liver fibrosis and inflammation (Fig. 1B). The HCC risk signature in a Food and Drug Administration–approved platform was analyzed as described.2, 3 The profiles were projected onto two reference series of HCC patients with active HCV infection (n = 63) and after SVR (n = 64) treated with curative surgery and followed for up to 15 years (Fig. 1C).2, 3 His predicted long-term HCC risk was improved after SVR but remained substantial (Fig. 1D,E). Therefore, HCC screening was continued at 3-month intervals.
| Variable | Pre-SVR | Post-SVR |
|---|---|---|
| White blood cell (/mm3) | 3,500 | 6,900 |
| Hemoglobin (g/dL) | 16.1 | 15.2 |
| Platelet count (× 103/mm3) | 125 | 161 |
| Total bilirubin (mg/dL) | 0.5 | 0.5 |
| Albumin (g/dL) | 4.1 | 4.5 |
| AST (IU/L) | 61 | 22 |
| ALT (IU/L) | 69 | 16 |
| Prothrombin time (INR) | 1.1 | 1.1 |
| AFP (ng/mL) | 10.6 | 4 |
| MELD score | 8 | 9 |
- Abbreviations: ALT, alanine transaminase; AST, aspartate transaminase; INR, international normalized ratio.
Despite the significant improvement of liver histology and biochemistry after SVR, a 22-mm lesion in segment 7 with a typical contrast enhancement pattern for HCC was determined by magnetic resonance imaging (Organ Procurement and Transplantation Network [OPTN] class 5B) at the age of 67. The AFP level remained low. This early-stage HCC tumor (American Joint Committee on Cancer [AJCC] stage I) was successfully treated by LT. The explanted liver demonstrated this tumor to be a poorly differentiated HCC but with no sign of microvascular invasion, i.e., local disease progression, supporting that the tumor was detected at an earlier stage without dissemination by the close follow-up as recommended from the gene signature assessment.
Discussion
HCV will remain a major cause of HCC in the coming decades, and HCC incidence may be higher in DAA-based SVR compared to interferon-based SVR.1 Given the anticipated exponential growth of a post-DAA-based SVR patient population, identification of a subset of SVR patients at risk of HCC is an urgent unmet need. Allocating HCC screening resources to high-risk patients will enable more cost-effective and practically feasible management of the patients. This case report suggests that molecular risk biomarker-based cancer risk prediction is a viable option, which is readily applicable for HCC risk prediction after surgical resection without changing clinical practice to obtain the sample and will also serve as the basis to explore serum surrogate biomarkers for nonsurgery post-SVR patients.
Acknowledgements
We thank Dr. Laurence Bennett for providing invaluable clinical information and critical reading of the manuscript.
REFERENCES
Author names in bold designate shared co-first authorship.




