Immunoglobulin G4-related sclerosing cholangitis
Potential conflict of interest: Nothing to report.
Abbreviations
-
- AIP
-
- autoimmune pancreatitis
-
- CBD
-
- common hepatic duct
-
- CCA
-
- cholangiocarcinoma
-
- CHD
-
- common hepatic duct
-
- ERCP
-
- endoscopic retrograde cholangiopancreaticography
-
- Ig
-
- immunoglobulin
-
- IgG4-RD
-
- IgG4-related disease
-
- IgG4-SC
-
- IgG4-related sclerosing cholangitis
-
- PSC
-
- primary sclerosing cholangitis
-
- Th
-
- T helper
A 64 year-old Caucasian gentleman presented with abnormal liver biochemistry (alkaline phosphatase: 212 IU/L; alanine aminotransferase: 75 IU/L; gamma-glutamyl transpeptidase: 301 IU/L; albumin, 38 g/L; bilirubin, 55 umol/L; international normalized ratio: 1.1). He was asymptomatic with no history of weight loss. He had a history of well-controlled ulcerative colitis. Axial imaging and an endoscopic retrograde cholangiopancreaticography (ERCP) performed at his local hospital demonstrated a complex stricture at the liver hilum suggestive of cholangiocarcinoma (CCA), but brushings were inconclusive for malignancy. A serum Ca 19-9 was normal. The patient underwent an ERCP and direct cholangioscopy, which demonstrated a stricture in the common hepatic duct (CHD) extending into the left and right hepatic ducts (Fig. 1A). The common bile duct (CBD) appeared thin and narrowed throughout its length, but endoscopic views failed to identify a clear area of stricturing or abnormality. Cholangioscopy-directed biopsies taken from the hilum demonstrated no evidence of malignancy, but evidence of ulceration with a plasma cell infiltrate with more than 20 plasma cells per high-power field positive for immunoglobulin (Ig)G4 immunostaining (Fig. 1B,C). Serum IgG4 levels were normal (1.03 g/L; normal range: 0-1.3). In accord with the HISORt diagnostic criteria1 (Table 1), the patient was diagnosed with IgG4-related sclerosing cholangitis (IgG4-SC). He was commenced on prednisone 30 mg once-daily for 4 weeks and then tapered by 5 mg every 2 weeks. Three months after starting prednisone, liver biochemistry and ERCP features improved (Fig. 2). The patient remains off prednisone and well to date.
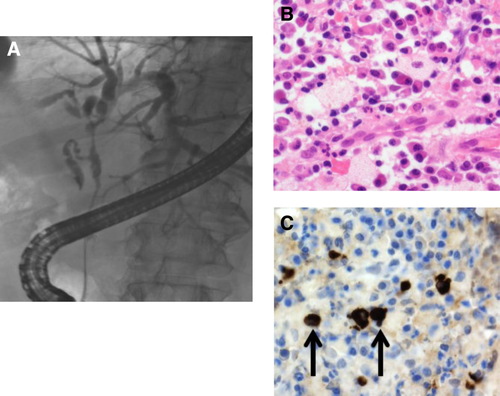
(A) ERCP demonstrating a CHD stricture, a CBD stricture extending into the left and right hepatic ducts. (B) Hematoxylin and eosin demonstrating extensive fibrous stroma with plasma cell infiltrate. (C) IgG4 immunostaining showing >20 IgG4+ plasma cells (arrows) per high-power film.
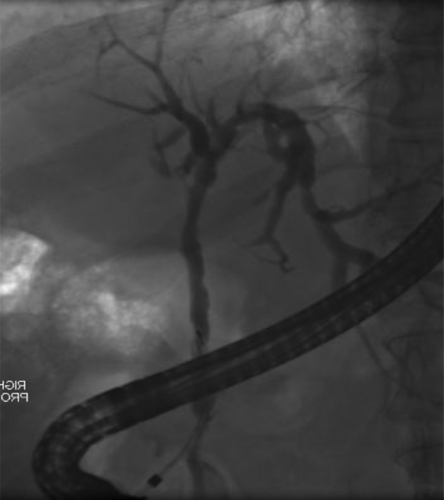
ERCP performed 3 months after commencement of prednisone demonstrating improvement of stricturing.
| Feature | Characteristics |
|---|---|
| Histology of bile duct | Lymphoplasmacytic scelorising cholangitis on resection specimens (lymphoplasmacytic infiltrate with >10 IgG4-positive cells/high-powered field within and around bile ducts with associated obliterative phlebitis and storiform fibrosis) |
| Imaging of bile duct | - One or more strictures involving intrahepatic, proximal extrahepatic or intrapancreatic bile ducts |
| - Fleeting/migrating biliary strictures | |
| Serology | Increased levels of serum IgG4 |
| Other organ involvement | Pancreatic, retroperitoneal fibrosis, renal lesion, salivary/lacrimal gland |
| Response to steroid therapy | Normalisation of liver enzymes or resolution of stricture (radiologically) |
The biliary manifestation of IgG4-related disease (IgG4-RD) is IgG4-SC. IgG4-RD is a multisystemic disorder affecting the pancreas, kidneys, liver, salivary glands, lungs, pericardium, meninges, and pituitary.2 IgG4-RD encompasses previously recognized conditions, such as retroperitoneal fibrosis, Riedel's thyroiditis, Mikulicz's disease, and sclerosing sialadenitis. The multisystemic involvement was first described in 2003 in patients with autoimmune pancreatitis (AIP).3 It is common for patients to present with tumefactive (mass-forming) lesions and are suspected to have malignancy. The pathogenesis of IgG4-RD is poorly understood, but inflammation and fibrosis appears to be driven by T helper (Th)2 and regulatory T cells, compared to Th1 or Th17 subsets in other autoimmune diseases.4, 5
There is a male preponderance with presentation commonly in the fifth or sixth decade of life with jaundice, weight loss, or abdominal pain. The HISORt criteria are used to make the diagnosis of IgG4-SC. As in our case, axial imaging can identify biliary strictures with associated thickening and inflammation evident on computed tomography. Serum IgG4 levels should be performed, but can be normal in up to 20% of patients with active disease. In addition, raised serum IgG4 levels have been reported in 9% of patients with PSC (primary sclerosing cholangitis) and 1% of patients with other liver diseases.6 Our case highlights the key role ERCP plays in the investigation and management of patients with suspected IgG4-SC, including direct cholangioscopy.7 The three histological hallmarks of IgG4-RD are an IgG4-positive lymphoplasmacytic tissue infiltrate (>10 IgG4-positive cells per high-power field), storiform fibrosis, and obliterative phlebitis.8 Important differential diagnoses of IgG-SC include CCA, pancreatic carcinoma, PSC, and secondary sclerosing cholangitis.
Corticosteroids are the mainstay of treatment in IgG4-SC, although randomized, controlled studies are lacking. Prednisone (30-40 mg) for 4 weeks followed by a reducing course (5 mg every 14 days) is recommended. A response to steroids can also help in establishing the diagnosis of IgG4-SC. A clinical and cholangiographic improvement should be evident within 4-6 weeks of commencing treatment. Our practice is to repeat imaging and blood tests in 4 weeks. Nonresponse to steroid therapy may be suggestive of “burnt-out disease” or a more fibrotic phenotype or an alternative diagnosis. Relapse is common in patients with IgG4-SC either after stopping treatment or during the taper and more common in patients with proximal strictures and increased IgG4 levels.1, 9 Patients that do relapse can be retreated with an additional course of steroids followed by the introduction of additional immunomodulatory drugs (i.e., azathioprine 1-2 mg/kg/day). Rituximab has also been used in patients that are intolerant of immunomodulatory drugs and steroid dependent.10 The natural history of IgG4-RD and IgG4-SC remains unclear, and the long-term risk of malignancy remains poorly delineated.
In conclusion, IgG4-SC should be considered in patients that present with cholangiopathy or hilar stricturing. A comprehensive clinical, radiological, histological, and endoscopic evaluation is required, in particular, direct cholangioscopy.




