Identifying a competency improvement strategy for infection prevention and control professionals: A rapid systematic review and cluster analysis
Nuo Chen, Shunning Li, Zhengling Kuang, and Ting Gong contributed equally to this study.
Abstract
Remarkable progress has been made in infection prevention and control (IPC) in many countries, but some gaps emerged in the context of the coronavirus disease 2019 (COVID-19) pandemic. Core capabilities such as standard clinical precautions and tracing the source of infection were the focus of IPC in medical institutions during the pandemic. Therefore, the core competences of IPC professionals during the pandemic, and how these contributed to successful prevention and control of the epidemic, should be studied. To investigate, using a systematic review and cluster analysis, fundamental improvements in the competences of infection control and prevention professionals that may be emphasized in light of the COVID-19 pandemic. We searched the PubMed, Embase, Cochrane Library, Web of Science, CNKI, WanFang Data, and CBM databases for original articles exploring core competencies of IPC professionals during the COVID-19 pandemic (from January 1, 2020 to February 7, 2023). Weiciyun software was used for data extraction and the Donohue formula was followed to distinguish high-frequency technical terms. Cluster analysis was performed using the within-group linkage method and squared Euclidean distance as the metric to determine the priority competencies for development. We identified 46 studies with 29 high-frequency technical terms. The most common term was “infection prevention and control training” (184 times, 17.3%), followed by “hand hygiene” (172 times, 16.2%). “Infection prevention and control in clinical practice” was the most-reported core competency (367 times, 34.5%), followed by “microbiology and surveillance” (292 times, 27.5%). Cluster analysis showed two key areas of competence: Category 1 (program management and leadership, patient safety and occupational health, education and microbiology and surveillance) and Category 2 (IPC in clinical practice). During the COVID-19 pandemic, IPC program management and leadership, microbiology and surveillance, education, patient safety, and occupational health were the most important focus of development and should be given due consideration by IPC professionals.
Abbreviations
-
- COVID-19
-
- coronavirus disease 2019
-
- lPC
-
- infection prevention and control
-
- lPCP
-
- infection prevention and control professional
-
- HAl
-
- healthcare-acquired infection
-
- HAls
-
- healthcare-associated infections
-
- PPE
-
- personal protective equipment
-
- WHO
-
- World Health Organization
1 INTRODUCTION
Infection prevention and control (IPC) is the taking of effective measures and nonpharmaceutical interventions to reduce the spread of illnesses such as coronavirus disease 2019 (COVID-19) and is an essential prerequisite for general medical treatment [1, 2]. Infection prevention and control professionals (IPCPs) have dual managerial and operational responsibilities [3]. The World Health Organization (WHO) publication, “Minimum requirements for infection prevention and control programmes” describes the minimum requirements for IPC programs at the national level [4]. However, despite this publication, significant gaps remain in practice around the world. A survey of 106 countries about the national minimum standards for IPC showed that only four countries met the WHO requirements [5]. In another survey, only five (45.45%) of the 11 nations studied had IPC physician training programs [6]. In a separate study of 20 low-income countries, only nine countries (45%) had a national IPC program, only four (20%) reported the existence of documents on implementing IPC strategies, and only one (5%) monitored adherence to IPC practices, highlighting deficits in IPC management systems and leadership [7]. A study of 65 hospitals found that 17 (26.15%) showed insufficient microbiological and surveillance capability for IPC [8]. The same situation exists in China. For example, a study there found that only 24.03% of IPCPs had enough knowledge to be prepared to face the COVID-19 pandemic, indicating deficiencies in education and training resources [9]. The Chinese IPC program has advanced significantly, but further training and educational resources are still needed. Other gaps include insufficient functioning IPC programs with annual work plans, lack of expertise in conducting IPC monitoring, inadequate IPC training, need for construction of a COVID-19-safe environment, and need to secure adequate IPC supplies, particularly personal protective equipment (PPE) [4].
COVID-19 no longer constitutes a public health emergency of international concern, but the pandemic provided insights into where current IPC efforts are working or insufficient. We conducted a systematic scoping review of lessons from the pandemic and carried out cluster analysis to provide practice recommendations for IPCP training and core competencies.
2 METHODS
2.1 Literature search strategy
A comprehensive systematic literature search was conducted without restrictions on region, publication type, or language. We searched the PubMed, Embase, Cochrane Library, Web of Science, CNKI, WanFang Data, and CBM databases using the terms provided in Table 1. The study period was from January 1, 2020 to February 7, 2023. To provide more evidence, we also searched the reference lists of the included studies and the relevant clinical practice guidelines.
| Databases | Search strategies |
|---|---|
| PubMed | #1 “hospitals” [Mesh] OR hospital OR ward OR hospital setting OR infirmary OR health care OR healthcare OR nosocomial [Title/Abstract] |
| #2 Covid-19 [Mesh] OR coronavirus diseases 2019 OR SARS-CoV-2 OR 2019-nCoV [Title/Abstract] | |
| #3 “infection control practitioners” [Mesh] OR practitioner, infection control OR practitioners, infection control OR infection control practitioner [Title/Abstract] | |
| #4 competency OR capacity OR ability OR capability OR competence [Title/Abstract] | |
| #5 #1 AND #2 AND #3 AND #4 | |
| WanFang data | #1 medical institutions OR hospital OR nosocomial OR ward OR healthcare [Title/Abstract] |
| #2 Covid-19 OR coronavirus disease 2019 OR SARS-CoV-2 OR 2019-nCoV [Title/Abstract] | |
| #3 infection preventionists OR infection control professionals OR infection prevention and control professionals OR infection prevention and control practitioners [Title/Abstract] | |
| #4 ability OR skill OR competency OR capacity [Title/Abstract] | |
| #5 #1 AND #2 AND #3 AND #4 |
2.2 Inclusion and exclusion criteria
Studies with the following characteristics were included: (1) an original article on IPCP core competencies during the COVID-19 pandemic; (2) in English or Chinese; and (3) using qualitative, cross-sectional, before–after, retrospective, or prospective observational study designs. Exclusion criteria included inappropriate study design, letters, conference abstracts, commentaries, case reports, and reviews with limited data, or inaccessible literature.
2.3 Data extraction
- (a)
Publication data: name of first author, publication year, geographic location, and literature types (qualitative, cross-sectional, before–after, retrospective, or prospective observational studies).
- (b)
Technical terms related to IPCPs' core competencies: the WHO guideline was imported to Weiciyun software (https://fenci.weiciyun.com/) to search for technical terms and to combine the domains of IPC core competencies (Table 3 of the WHO guideline) [10]. Following the integration, 80 technical terms were included in the analysis (Supporting Information S1: Tables S1 and S2).
- (c)
Frequency of technical terms: The included literature was imported into the Weiciyun software and the frequencies of technical terms in each paper were extracted using a general analysis function.
2.4 Statistical analysis
- (a)
Data integration: First, technically synonymous terms were normalized and combined, and overly vague terms were removed. Second, the list of technical terms was ordered by the frequency of each word in the literature.
- (b)
Acquisition and classification of high-frequency terms: First, high-frequency terms were defined using the following formula proposed by Donohue in 1973 [10]:
()where T is the dividing frequency of the high-frequency and low-frequency terms, and I1 is the number of technical terms mentioned only once.Second, high-frequency terms for the same role were classified as a single core competency following the WHO guidelines [11]. The frequency of each core competency was then calculated.
- (c)
Cluster analysis: First, the word frequency matrix table is constructed by the occurrence of high-frequency words related to core competence in each paper and their corresponding article numbers. Second, we used SPSS software (version 26, IBM) to perform hierarchical clustering using the within-group linkage method on the matrix results. The approximate matrix was obtained after hierarchical clustering (Supporting Information S1: Table S3), and the competencies with similar difference values were grouped into a single category. The squared Euclidean distance was used as the metric in the clustering approach, and the clustering was visualized using a dendrogram.
3 RESULTS
3.1 Literature search
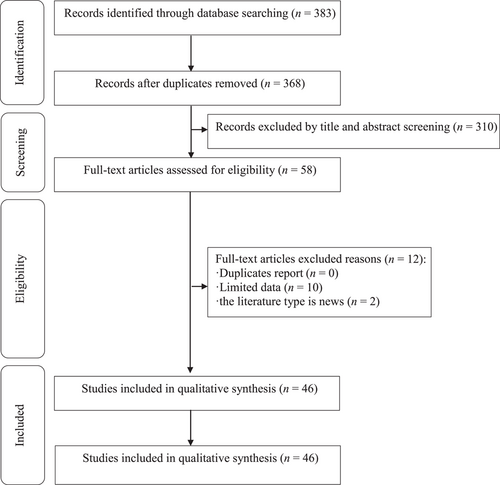
The initial database search yielded 383 unique citations, of which nine were from PubMed, 10 from Embase, two from the Cochrane Library, 193 from Web of Science, 158 from CNKI, five from WanFang Data, and six from CBM. Fifteen duplicates were removed. After excluding studies whose titles and abstracts suggested that they did not meet the inclusion criteria, 58 publications remained. Of these, 10 had limited data and two were inappropriate types of paper. The final meta-analysis therefore included 46 eligible studies. The list of excluded studies and the reasons for their exclusion are shown in Figure 1.
3.2 Study characteristics
Of the 46 studies included in the analysis, 14 were carried out in the United States [12-25], 11 in China [26-36], four in each of the United Kingdom [27, 37, 39, 38] and Switzerland [6, 7, 40, 41], three in Italy [42-44], two in South Africa [45, 46] and one in each of Germany [8], Saudi Arabia [47], Finland [48], the Netherlands [49], Australia [50], Ghana [51], Pakistan [52], and Singapore [53]. There were 20 cross-sectional studies [8, 15-17, 24, 25, 31, 32, 34-37, 39-41, 49-52, 54], 15 qualitative studies [6, 7, 13, 14, 19, 21, 23, 26, 28, 29, 38, 42, 45, 46, 48], eight before–after studies [12, 20, 22, 27, 30, 33, 47, 53], two retrospective studies [18, 44] and one prospective observational study [43] (Table 2).
| Study | Country | Article type | High-frequency terms |
|---|---|---|---|
| Tsioutis 2020 [6] | Basel, Switzerland | Qualitative research | IPC training, Microbiology, Waste management |
| Tomczyk 2021 [7] | Geneva, Switzerland | Qualitative research | IPC training, Hand hygiene, Device-associated infection |
| Aghdassi 2020 [8] | Berlin, Germany | Cross-sectional study | IPC training, Antimicrobial resistance, Hand hygiene |
| Alsuhaibani 2021 [12] | Iowa, USA | Before–after study | Hand hygiene, Occupational health, Central line-associated bloodstream infections, Catheter-associated urinary tract infections |
| Herstein 2021 [13] | Nebraska, USA | Qualitative research | Emergency management, Isolation rooms |
| Holdsworth 2020 [14] | Norcross, USA | Qualitative research | Use of PPE |
| Rebmann 2021 [15] | Missouri, USA | Cross-sectional study | Use of PPE, Hand hygiene |
| Rebmann 2020 [16] | Missouri, USA | Cross-sectional study | Use of PPE, Hand hygiene |
| Schildhouse 2022 [17] | Michigan, USA | Cross-sectional study | Use of PPE, Central line-associated bloodstream infections, Catheter-associated urinary tract infections |
| Fakih 2021 [18] | Missouri, USA | Retrospective study | Central line-associated bloodstream infections, Catheter-associated urinary tract infections |
| Tadavarthy 2020 [19] | Philadelphia, USA | Qualitative research | Hand hygiene, Waste management |
| Penna 2022 [20] | Georgia, USA | Before–after study | Antibiotic resistance, IPC training, Hand hygiene |
| Rebmann 2021 [21] | Missouri, USA | Qualitative research | Ventilator-associated pneumonia, Catheter-associated urinary tract infections |
| Pokrajac 2020 [22] | California, USA | Before–after study | Use of PPE, Hand hygiene |
| Collins 2021 [23] | Washington, USA | Qualitative research | Use of PPE, IPC training |
| Rebmann 2021 [24] | Missouri, USA | Cross-sectional study | Use of PPE, Occupational health |
| Cole 2020 [25] | California, USA | Cross-sectional study | Hand hygiene, Use of PPE |
| Cui 2021 [26] | Hangzhou, China | Qualitative research | Occupational health, IPC training |
| Li 2022 [27] | Chengdu, China | Before–after study | Emergency management, Isolation rooms, IPC training |
| Zhang 2020 [28] | Wuhan, China | Qualitative research | Emergency management, IPC training |
| Du 2021 [29] | Chengdu, China | Qualitative research | Occupational health, IPC training |
| Tan 2020 [30] | Beijing, China | Before–after study | Use of PPE, Hand hygiene |
| Yao 2021 [31] | Guizhou, China | Cross-sectional study | Emergency management, IPC training, Antimicrobial resistance |
| Zhang 2021 [32] | Xian, China | Cross-sectional study | Waste management, Antimicrobial resistance, HAI surveillance |
| Zang 2021 [33] | Nanjing, China | Before–after study | Hand hygiene, Use of PPE, Emergency management, Occupational health, IPC training |
| He 2020 [34] | Anhui, China | Cross-sectional study | Hand hygiene, Antimicrobial resistance, Waste management, IPC training |
| Chen 2021 [35] | Guangdong, China | Cross-sectional study | Catheter-associated urinary tract infections, Ventilator-associated pneumonia, Surgical site infection, Antimicrobial resistance, Hand hygiene, IPC training |
| Cui 2022 [36] | Shanghai, China | Cross-sectional study | Antimicrobial resistance, Emergency management, Microbiology, Epidemiology, Occupational health, IPC training |
| Castro-Sánchez 2020 [54] | London, UK | Cross-sectional study | Use of PPE, Patient safety, Hand hygiene, IPC training |
| Chater 2022 [37] | London, UK | Cross-sectional study | Antimicrobial resistance |
| Kamere 2022 [38] | London, UK | Qualitative research | Antimicrobial resistance, Healthcare-associated infections (HAIs) surveillance, Hand hygiene, IPC training |
| Norton 2020 [39] | Bury St Edmunds, UK | Cross-sectional study | Use of PPE, IPC training, Hand hygiene |
| Tomczyk 2022 [40] | Geneva, Switzerland | Cross-sectional study | IPC training, Hand hygiene |
| Tartari 2020 [41] | Geneva, Switzerland | Cross-sectional study | Antimicrobial resistance, IPC training, HAI surveillance, Hand hygiene |
| Puro 2022 [42] | Rome, Italy | Qualitative research | IPC training, Disinfection and sterilization of tools and equipment, Hand hygiene |
| Cattelan 2020 [43] | Padova, Italy | Prospective observational study | Use of PPE, HAI surveillance, Hand hygiene |
| Mauro 2021 [44] | Naples, Italy | Retrospective study | Emergency management, Pre-checking and triage |
| Mehtar 2020 [45] | Cape Town, South Africa | Qualitative research | Surgical site infection |
| Patel 2020 [46] | Johannesburg, South Africa | Qualitative research | Use of PPE |
| Lingawi 2022 [47] | Makkah, Saudi Arabia | Before–after study | Use of PPE, Hand hygiene |
| Lohiniva 2022 [48] | Helsinki, Finland | Qualitative research | Hand hygiene, Use of PPE |
| Dekker 2020 [49] | Amsterdam, Netherlands | Cross-sectional study | Hand hygiene |
| Sotomayor-Castillo 2021 [50] | NSW, Australia | Cross-sectional study | Use of PPE, Emergency management |
| Oppong 2022 [51] | Accra, Ghana | Cross-sectional study | Standard precautions, Hand hygiene, Waste management, IPC training |
| Savul 2020 [52] | Islamabad, Pakistan | Cross-sectional study | Standard precautions, Transmission-based precautions, Hand hygiene, IPC training |
| Wee 2020 [53] | Singapore | Before–after study | Standard Precautions, Hand hygiene, Central line-associated bloodstream infections |
- Abbreviations: HAI, healthcare-associated infection; IPC, infection prevention and control; PPE, personal protective equipment.
3.3 Technical terms related to IPCPs' core competencies
Overall, 39 technical terms related to IPCPs' core competencies were extracted in this study, including four words with a frequency of two and six words with a frequency of one. Using the Donohue formula, the threshold of the high-frequency terms was defined as 3 (T = 3), indicating that the high-frequency terms should occur more than twice. This gave a total of 29 high-frequency technical terms. Some of these had similar meanings, and we therefore added them together. Other terms were not included because of their relatively low frequency but were still considered.
Figure 2 shows that “IPC training” occurred with the highest frequency (184 times, 17.3%), followed by “hand hygiene” (172 times, 16.2%). The least common phrase was “pre-checking and triage” (three times, 0.3%). The core competency category “IPC in clinical practice” contained the highest number of high-frequency terms (13), and “education” contained the lowest number (one). A higher frequency suggests that this competency is more valued. The importance of these low-frequency competencies should thus be strengthened in future research and clinical practice.
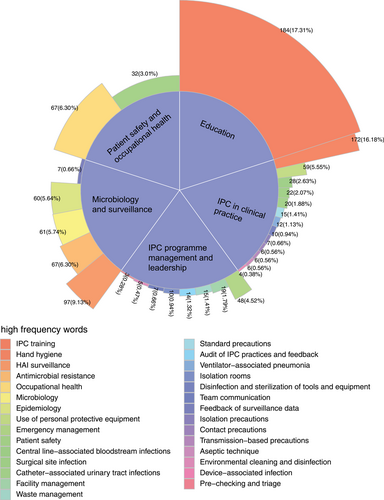
The innermost blue part of the circular Manhattan plot indicates the five core competencies of IPCPs. The multicolored middle layer shows all the high-frequency terms categorized into the five core competencies. The numbers show the total frequency and proportion of the total of each high-frequency term. The legends top to bottom and left to right correspond to the frequency data from most to least.
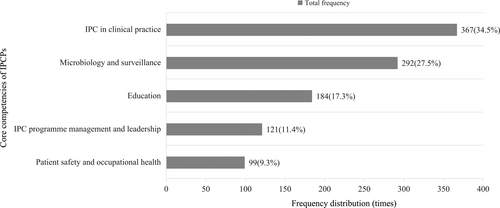
Figure 3 shows that the core competency “IPC in clinical practice” had the highest frequency (367 times, 34.5%), followed by “Microbiology and surveillance” (292 times, 27.5%). The frequency of “Patient safety and occupational health” was the lowest (99 times, 9.3%). The maximum frequency (“IPC in clinical practice”) was 73% higher than the minimum frequency (“Patient safety and occupational health”). This suggests that IPC in clinical practice is widely understood, and a focus. However, patient safety and occupational health are of less concern, and may even be ignored. The lower the frequency, the less that competence is discussed, indicating areas for development. We found significant differences among the five core competencies of IPCPs, highlighting varying levels of attention on these competences.
3.4 Cluster analysis
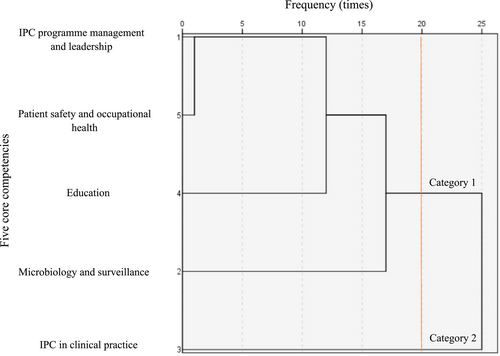
The results of the cluster analysis are shown in Figure 4 and Supporting Information S1: Table S3. With a distance threshold of 20, the cluster analysis identified two core competency categories: Category 1: IPC program management and leadership, Patient safety and occupational health, Education, and Microbiology and surveillance; and Category 2: IPC in clinical practice. The clustering coefficient was 5669.
A detailed explanation of the competences is shown in Table 3.
| Category | IPCPs' core competencies | Detailed explanation | |
|---|---|---|---|
| Category 1 | IPC program management and leadership | Use management strategies and leadership to plan and operationalize an IPC program, develop evidence-based IPC guidelines, standard operating protocols, training resources and monitoring tools, and undertake monitoring and feedback of adherence to guidelines and recommendations. Support the achievement of adequate infrastructure for water, sanitation and hygiene and IPC and procurement of supplies. Assess the infection risks related to building design, construction and renovation, and provide guidance based on IPC principles. Use communication skills to interact with teams, senior management, patients and families, and other audiences [55]. | |
| Microbiology and surveillance | A coherent set of actions to promote the responsible use of antimicrobials. The primary goal of antimicrobial stewardship is to optimize clinical outcomes while minimizing unintended consequences of antimicrobial use, including toxicity, the selection of pathogenic organisms (such as Clostridium difficile), and the emergence of resistance [56]. Facility-based healthcare-acquired infection (HAI) surveillance should be performed to guide IPC interventions and detect outbreaks, including antimicrobial resistance surveillance, with timely feedback of results to healthcare workers and stakeholders and through national networks [4]. | ||
| Education | IPC education should be in place for all healthcare workers by using team- and task-based strategies that are participatory and include bedside and simulation training to reduce the risk of HAI and antimicrobial resistance [4]. | ||
| Patient safety and occupational health | Demonstrate an understanding of the key principles of quality and patient safety and of the epidemiology, burden of risk factors and causes of adverse events, near-misses, accidents, and dangerous incidents in healthcare. Contribute to designing, developing, implementing, and evaluating quality improvement and patient safety programs. Understand the infection risks related to employment and support the implementation of appropriate preventive measures to provide a safe environment and healthy workforce [11]. | ||
| Category 2 | IPC in clinical practice | Standard precautions | A set of activities designed to prevent the transmission of organisms between patients/staff for the prevention of HAI. They must be applied to all patients who require healthcare, by all healthcare workers in all healthcare settings. They include hand hygiene; use of PPE; handling and disposal of waste and sharps; handling and management of clean and used linen; environmental cleaning; and decontamination of equipment [57]. |
| Transmission-based precautions | Additional measures focused on the specific mode of transmission of the microorganism and always used in addition to standard precautions. They are grouped into categories according to the route of transmission of the infectious agent. Transmission-based precautions should be applied when caring for patients with known infections, patients who are colonized with an infectious organism and asymptomatic patients who are suspected of/under investigation for colonization or infection with an infectious microorganism [58]. | ||
| Decontamination and reprocessing of medical devices and equipment | All steps that are necessary to make a contaminated reusable medical device ready for its intended use. These steps may include cleaning, functional testing, packaging, labeling, disinfection, and sterilization [59]. | ||
| Catheter-associated blood-stream infection prevention | Understand the epidemiology, risk factors, burden, clinical presentation, and complications of catheter-associated bloodstream infections, catheter-associated urinary tract infections, surgical site infections, and healthcare-associated pneumonia, use evidence-based guidelines for prevention, and monitor the implementation of IPC measures [60]. | ||
| Catheter-associated urinary tract infection prevention | |||
| Surgical site infection prevention | |||
| Prevention of healthcare-associated pneumonia | |||
| Healthcare-associated outbreak prevention and management | Prevent, detect, manage, and control healthcare-associated outbreaks. Conduct IPC training activities and develop effective communications during outbreaks in healthcare facilities [61]. | ||
| COVID-19 blood tests | COVID-19 blood tests and related treatments are more effective when the budget, IPCP education level, and national development level are high [62]. | ||
- Abbreviations: COVID-19, coronavirus disease 2019; HAI, healthcare-associated infection; IPC, infection prevention and control; PPE, personal protective equipment.
4 DISCUSSION
Among the core competencies of IPCPs, it is particularly important to focus on IPC program management and leadership, microbiology and surveillance, education, and patient safety and occupational health. To enable IPCPs to cope with emerging infectious diseases with unknown causes or to prevent and control infections in hospitals, they should preferentially conduct microbiological surveillance backed up by multiple means, and ensure that they keep learning and attending training.
IPC in clinical practice is a comprehensive and highly regarded skill with many facets, including recognizing the risk of healthcare-acquired infections (HAIs), combining multiple approaches to IPC in clinical practice, and appraisal of outcomes. A prospective study found that a comprehensive hospital infection control strategy could successfully prevent infection among IPCPs, suggesting the importance of IPC program management and leadership [43]. Risk stratification models used in clinical practice can identify high-risk patients and assist nursing teams to manage resources including interventions, hospital beds, and staffing [63]. The clinical practice element of IPC, including but not limited to PPE usage guidelines and antimicrobial stewardship, patient monitoring, environmental surveillance, environmental cleaning and disinfection, and hand hygiene, plays an important role [43, 64].
We also found that the five core competencies are tightly linked. A cross-sectional study in four community hospitals in California found that the number of multidrug-resistant organisms could be decreased by providing additional education to IPCPs about appropriate PPE usage and the importance of hand hygiene, highlighting the capacity of education to improve microbiological surveillance [25]. A large-scale London hospital group developed the “PPE Helper Program”, which provided IPCPs with PPE support and education [54]. Enrolled workers had higher skills than their non-enrolled peers in using PPE appropriately (82.5% vs. 56.5%) [54]. A multicountry survey of 262 IPCPs of 10 nationalities showed that those who had received antimicrobial resistance training had significantly higher scores than those who had not [37].
- (a)
Establish training courses: when training new IPCPs, assist them to acquire work experience to strengthen their training, especially on correct and responsible use of antibiotics [56]; communicating with patients and their families [55]; epidemiology, clinical manifestations, and complications of HAIs [60]; basic precautions such as hand hygiene, use of PPE, and disposal of waste and sharp tools [59] and to help them develop a good mindset and value the patient and health;
- (b)
Develop assessment indicators: personal competency assessment indicators should be established based on the four competencies that need to be prioritized for development and targeted improvement of personal competencies;
- (c)
Regular assessment: managers of IPCPs should plan and implement IPC programs, regularly inspect and summarize the training courses, and help IPCPs identify gaps in their knowledge.
This study has some limitations. First, this article focuses on the priorities for developing core competencies during the COVID-19 pandemic. The literature from before the pandemic was not included in the analysis, and thus the conclusion has time limitations. Further research is needed to combine our findings with the literature from before the pandemic. Second, the study did not consider factors such as the varying levels of medical resources in different areas, different educational backgrounds, or the job tenure of IPCPs. For example, different countries and regions have different levels of medical resources, and the equipment and health conditions provided during the pandemic were very different. The education level of IPCPs in different medical institutions is also inconsistent, resulting in different response speeds to disease prevention and COVID-19. IPCPs with greater experience may be better able to make quick judgments about the severity of an outbreak [65]. In future studies, these factors should be examined in different cases to expand the results. Nevertheless, the identified core competencies could provide a development path for junior IPCPs to rapidly improve their competencies. They could also enable advanced IPCPs to improve their capabilities.
5 CONCLUSION
Our study summarized the five core competencies of IPCPs during the pandemic and divided them into two categories. We identified four competences in particular for prioritization. These were IPC program management and leadership, microbiology and surveillance, education, and patient safety and occupational health. We suggest that the future training of IPCP personnel should take these four competences as a clear entry point for improving abilities. It is particularly important to focus on the leadership role of senior managers, strengthening communication with patients and their families, correctly using antibacterial drugs, and focusing on patients and their health, especially to reduce the rate of HAIs.
AUTHOR CONTRIBUTIONS
Nuo Chen: Conceptualization and writing—original draft. Shunning Li: Writing—original draft and methodology. Zhengling Kuang: Writing—original draft and software. Ting Gong: Writing—original draft and data curation. Weilong Zhou: Formal analysis and supervision. Ying Wang: Writing—review and editing and supervision.
ACKNOWLEDGMENTS
The authors are very grateful for the funding support we have received. This study was supported by the National Natural Science Foundation of China (Grant no. 52178080), the Major Research Project of the Hospital Management Research Institute of the National Health Commission (GY2023011) and the National Institute of Hospital Administration Management of China (GY2023049).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
Ethics approval was waived for this study because no patient data were reported.
INFORMED CONSENT
The need for informed consent was waived for this study because no new patient data were reported.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.