Management of catheter ablation in arrhythmia patients during the coronavirus disease 2019 epidemic
All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Abstract
Aims
Health care providers have reduced outpatient services and delayed elective cardiac surgeries during the coronavirus disease 2019 (COVID-19) epidemic, while a large number of patients face more cardiovascular risks compared with those of the pandemic. The present study attempted to explore the management of catheter ablation in arrhythmia patients during the pandemic.
Methods and results
From 1 January 2020 to 24 March 2020, a total of 269 arrhythmia patients hospitalized for catheter ablation under strict risk assessments and careful infection prevention were retrospectively analysed and considered for our analysis at our centre. Preventive measured included a 14 day quarantine, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) nucleic acid detection, adoption of personal protection equipment, application of hand disinfectant, management of hospital visitors, and maintenance of environmental hygiene. Three patients who had fever following ablation and were finally excluded from SARS-CoV-2 infection, and no hospital infection occurred during the 3.1 ± 1.5 day hospitalization period. Additionally, 258/269 (95.9%) patients were free from arrhythmia after a median 133 day follow-up (Q1, 81; Q3, 143; ending 1 June 2020), and no SARS-CoV-2 infections occurred at follow-up.
Conclusions
By adopting strict risk assessments and careful infection prevention measures, catheter ablation in patients with arrhythmia can be safely and effectively performed during the COVID-19 epidemic in well-controlled areas.
Introduction
As of 1 June 2020, over 6 million people have been affected by coronavirus disease 2019 (COVID-19), and >280 000 people have died worldwide.1 In China, a total of 83 022 cases have been reported till 1 June 2020.2 In first-tier cities with large populations like Shanghai, the epidemic was less severe compared with that of Wuhan. In total, 673 cases were reported in Shanghai till 1 June,3 and the number of cases initially rose rapidly after 10 January, peaking on 5 February and declining slowly afterward.4
In addition to infection risk, cardiovascular risk may also increase owing to preventive measures that must be undertaken during the COVID-19 epidemic.5 Many health care centres reduced outpatient services and delayed elective cardiac surgeries, which may significantly confer impacts beyond the pandemic.6 Moreover, being exposed to COVID-19 may cause acute outbursts of arrhythmias, resulting in cardiac death and morbidity, especially in those in which conservative treatment is not effective as well as those with recurring arrhythmias. Such points emphasize the necessity of catheter ablation over medical therapy or cardioversion in the treatment of arrhythmia.
Accordingly, this study attempts to explore the management of catheter ablation during the COVID-19 epidemic in order to verify its necessity and feasibility in well-controlled epidemic areas.
Methods
This study provides a retrospective single-centre analysis. Because Shanghai's level of major public health emergency was shifted from primary to secondary in 24 March 2020, this study included all patients who have received catheter ablation for symptomatic arrhythmia with poor response to antiarrhythmic drugs at our centre between 1 January 2020 and 24 March 2020.
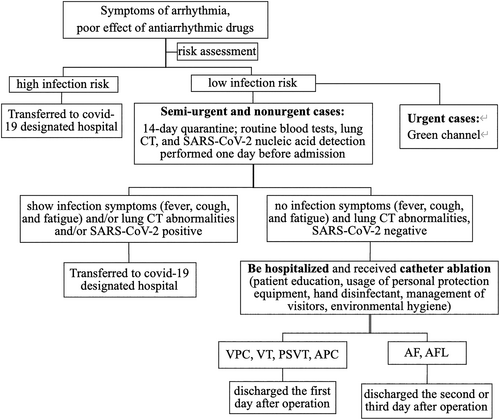
Accordingly, a modified workflow for arrhythmia disease catheter ablation was established at our centre (Figure 1), which was agreed upon among the local cardiologists and was comprehensively evaluated within the risk–return ratio for both patients and health care workers.
Prevention measures prior to admission
All patients admitted to hospital were required to undergo risk assessment. Here, health care workers observed COVID-19-related symptoms (fever, cough, fatigue, and gastrointestinal symptoms) and inquire about their epidemiological contact history with epidemic areas, infected patients, and suspected infected patients.
Once infection symptoms or contact history was confirmed, patients were marked as high-infection-risk patients and transferred to a COVID-19 designated hospital for quarantine and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) nucleic acid detection test. Low-infection-risk patients were divided into urgent or emergent cases, semi-urgent cases, and nonurgent or elective cases as recommendation.7 For urgent or emergent cases, there were a ‘green channel’ followed for therapy. Once excluded from high-infection-risk cases, they immediately received routine blood tests, lung computed tomography (CT), and SARS-CoV-2 nucleic acid detection. Suspected infection and infection cases were immediately transferred to a COVID-19 designated hospital for treatment. For other urgent cases, catheter ablation was performed in a special catheterization laboratory dedicated to emergency interventional surgeries following the infection prevention measure below. Otherwise, patients received a 14 day quarantine in Shanghai prior to admission in order to observe for COVID-19-related symptoms. The 14 day quarantine period was confirmed by the ‘communication big data and itinerary card’ as well as the Shanghai local residents committee. A mobile phone application provided by a joint venture between China Telecom, China Mobile, China Unicom, and China Academy of Information and Communications Technology, the ‘communication big data and itinerary card’ checked the personal domestic and international itinerary of patients in the last 14 days by analysing their mobile phone signal data, which may be obtained from the location of the base station where the mobile phone is located, having extremely strict security and privacy protection measures while boasting high authenticity and accuracy. Moreover, quarantine was performed under the assistance of the Shanghai local residents committee, in which the local residents committee staff visited patients' residences in Shanghai every day and issued a certificate on the last day of the quarantine period. Following the 14 day quarantine period, routine blood tests, lung CT, and SARS-CoV-2 nucleic acid detection were performed 1 day prior to admission. If infection or suspected infection symptoms, lung CT abnormalities or a positive SARS-CoV-2 nucleic acid test were displayed during such period, the patients were transferred to a designated hospital for further diagnosis and treatment. Those who were infection-free were admitted to our centre.
Perioperative prevention measures
Patient education pertaining to the epidemic included the latest information regarding the epidemic's progress, the government's newest policies on the epidemic, and popularization science of epidemic prevention performed during hospitalization. All patients were required to wear masks and use hand disinfectant. Excluding one fixed family member, no other visitors were allowed to visit or accompany the patient. Additionally, health care workers were not allowed to leave Shanghai. Additional personal protection equipment including disposable caps, goggles, gowns, and gloves were required for their daily medical activities. Their body temperatures were measured every day before work, and SARS-CoV-2 nucleic acid detection tests were performed every 2 weeks for health care workers. Environmental hygiene was also done every day. The use of central air conditioning was reduced, while ventilation with the outside environment increased.
When performing ablation, different levels of personal protection equipment from the Regulation for Prevention and Control of Healthcare Associated Infection of Airborne Transmission Disease in Healthcare Facilities8 were obtained. Level 2 protection (goggles or facemask, N95 respirator, disposable cap, disposable protective overall, medical gloves, disposable shoe covers, and rapid hand disinfection solution) was sufficient for ordinary patients as well as daily medical activities.
Following catheter ablation, and after no complications were reported, patients were discharged as soon as possible in order to prevent nosocomial infection. Patients with premature ventricular contractions and paroxysmal supraventricular tachycardia were usually discharged on the first day after operation, while atrial fibrillation (AF) patients were usually discharged on the second or third day after operation.
Special attention was given to asymptomatic COVID-19 patients on admission. During hospitalization, once COVID-19-related symptoms were observed, patients were isolated in a single room with air sanitization facilities and were immediately subjected to SARS-CoV-2 nucleic acid detection so as to exclude infection. If SARS-CoV-2 tested negative, patients were removed from the single quarantine room, after which routine therapy was continued. However, if SARS-CoV-2 tested positive, patients were transferred to COVID-19 designated hospitals as soon as possible.
Follow-up
COVID-19-related symptoms were observed during the entire period of hospitalization, including fever, cough, fatigue, and gastrointestinal symptoms. Hospital infection was defined by the displayed symptoms with COVID-19 nucleic acid detection showed positive in hospital.
Clinical follow-up was performed between 1 February 2020 and 1 June 2020. Under the protection of PPE such as masks, patients were required to attend outpatient clinics in person and had 24 h Holter electrocardiograms done on every single month following ablation for the first 3 months. SARS-CoV-2 nucleic acid detection was also done during the outpatient visit. Additionally, for AF patients, European Heart Rhythm Association (EHRA) score was assessed prior to ablation and during the last follow-up. Recurrence of AF or atrial flutter (AFL) was defined as any documented AF/atrial tachycardia (AT) episode > 30 s following a 1 month blanking period. Recurrence of other arrhythmias was defined as any documented arrhythmia that was the same prior to ablation. Monthly telephone interviews were also done after the first 3 months.
Definition of complications
Major complications were defined as transient ischaemic attack (TIA), stroke, severe bleeding events, pneumothorax or haemothorax, high-degree (>70%) pulmonary vein (PV) stenosis, atrioesophageal fistula, phrenic nerve palsy pericardial tamponade, and arterio-venous fistula requiring surgery. Haematoma at access sites and PV stenosis < 70% were considered minor complications.
Statistical analysis
Statistical analysis was performed using SPSS version 25.0. Continuous data were presented as mean ± SD or median with inter-quartile range. Categorical variables were reported as frequencies (percentages). The difference between the value of EHRA score was evaluated by a generalized linear mixed model.
Sample data availability statements
The data underlying this article will be shared on reasonable request to the corresponding author.
Statement of assurance
Informed consent was obtained from each patient. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in the prior approval taken from the institution's human research committee.
Results
Patient characteristics
From 1 January 2020 to 24 March 2020, a total of 269 patients were prepared for catheter ablation at our centre. During the risk assessment prior to admission, three patients were recognized as having suspected COVID-19 owing to fever and were suggested for transfer to a COVID-19 designated hospital. Another patient had fever during the 14 day quarantine before admission, and all four patients were confirmed to be infection-free and came back to our centre after a new 14 day quarantine once their body temperature was normal. Finally, 269 patient [152/269 male (56.5%)] cases with symptomatic arrhythmia and poor response to conservative treatment received catheter ablation at our centre, of which 185 (68.8%) had AF or AFL, four (1.5%) had atrial premature contraction or atrial tachycardia, 49 (18.2%) had paroxysmal supraventricular tachycardia, and 31 (11.5%) had ventricular premature contraction (VPC) or ventricular tachycardia (VT). All the patients were marked as semi-urgent or nonurgent cases. Patients ranged from 15 to 82 years old with a median age of 65 years (Q1, 55; Q3, 71). As the Chinese government prohibits the movement of people in severely affected provinces such as Hubei or Guangdong, no patients came from provinces heavily affected by SARS-CoV-2. Accordingly, 175 (65%) patients were from Shanghai, and 94 (35%) patients came from other provinces in China, including 24 from Jiangsu, 23 from Zhejiang, 19 from Shandong, 9 from Anhui, 8 from Fujian, 4 from Jiangxi, 3 from Yunnan, 2 from Henan, and 2 from Heilongjiang. Furthermore, 26 (9.7%) patients had heart failure before ablation, and 25 were AF patients. The baseline clinical characteristics of the enrolled patients are shown in Table 1.
| Characteristics | All patients (n = 269) | AF/AFL (n = 185, 68.8%) | AT/APC (n = 4, 1.5%) | PSVT (n = 49, 18.2%) | VT/VPC (n = 31, 11.5%) |
|---|---|---|---|---|---|
| Age (years) | 65 (55, 71) | 68 (60, 73) | 45.5 (34.3, 57.5) | 53 (31, 66) | 55 (36, 63) |
| Male, n (%) | 152 (56.5%) | 109 (58.9%) | 2 (50%) | 25 (51%) | 31 (51.6%) |
| hospitalization time (days) | 3 ± 1.5 | 3.8 ± 1.0 | 2.3 ± 1.0 | 1.1 ± 0.3 | 1.1 ± 0.3 |
| Local Shanghai patients, n (%) | 175 (65%) | 116 (62.7%) | 2 (50.0%) | 38 (77.6%) | 19 (61.3%) |
| Coronary heart disease | 32 (11.9%) | 30 (16.2%) | 0 | 0 | 2 (6.6%) |
| Hypertension | 38 (14.1%) | 28 (15.1%) | 1 (25%) | 5 (10.2%) | 4 (12.9%) |
| Diabetes mellitus | 24 (8.9%) | 23 (12.4%) | 0 | 0 | 1 (3.2%) |
| Heart failure | 26 (9.7%) | 25 (13.5%) | 0 | 0 | 1 (3.2%) |
| LVEDD (mm) | 47.2 ± 5.1 | 47.6 ± 5.3 | 43.5 ± 3.9 | 46.1 ± 4.3 | 47.3 ± 4.6 |
| LVEF (%) | 61.8 ± 7.8 | 61.4 ± 9.1 | 67.0 ± 1.8 | 62.7 ± 3.0 | 62.1 ± 4.9 |
| EHRA score | / | 3 (3, 4) | / | / | / |
- Values are means ± standard deviations; medians with 25th, 75th percentiles; and frequencies (percentages).
- AF, atrial fibrillation; AFL, atrial flutter; APC, atrial premature contraction; AT, atrial tachycardia; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; PSVT, paroxysmal supraventricular tachycardia; VPC, ventricular premature contraction; VT, ventricular tachycardia.
Follow-up after ablation
The hospitalization time was 3.1 ± 1.5 days, and no hospital infection occurred. Three AF patients had fever on the first day after ablation. Their maximum body temperatures were 37.8°C, 38.0°C, and 38.1°C, with no other symptoms of COVID-19. All three patients were isolated and received SARS-CoV-2 nucleic acid tests immediately following onset of fever, which was negative in all of them. After anti-inflammatory rehydration and nutritional support, two patients' body temperatures returned to normal on the second day after ablation, and another became normal on the second day after ablation. Procedure outcomes are shown in Figure 2.
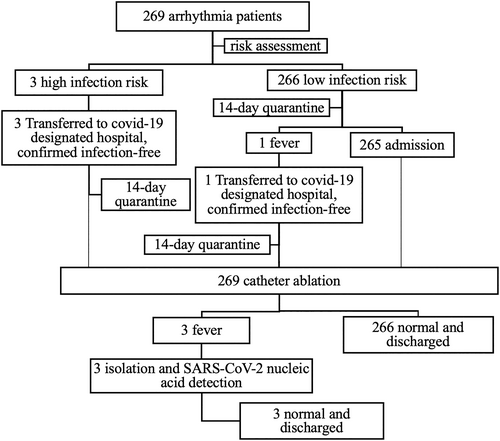
After a median follow-up duration of 133 days (Q1, 81; Q3, 143; ending 1 June 2020) following catheter ablation, 258/269 (95.9%) patients were free from arrhythmias (±AAD). All results of the SARS-CoV-2 test were negative at the outpatient visits, and no SARS-CoV-2 infection occurred during follow-up. EHRA scores improved during follow-up from a median of 3 to 1 (Δ2, P < 0.001) in AF patients. Among 11 patients with recurrent arrhythmia, 10 were AF patients (three paroxysmal AF and seven persistent AF or long-standing persistent AF), while one patient had VPC originating from the left posterior papillary muscle.
Complications
No severe complications occurred during hospitalization. Additionally, two AF patients had their hospitalization extended owing to femoral vein puncture point haematoma, which was absorbed following access site pressing and bandaging.
Discussion
In the present study, the management of catheter ablation was investigated in arrhythmia patients during the COVID-19 epidemic in Shanghai. Here, 269 arrhythmia patients received catheter ablation, which demonstrated that (i) although prevention measures were taken, the success rate of catheter ablation did not reduce. Moreover, prevention measures ensured that catheter ablation may be safely performed with an infection rate of 0% at the study's centre; (ii) a beneficial clinical outcome of catheter ablation can be achieved regardless of the type arrhythmia, with 95.9% patients becoming free of arrhythmias (±AAD); (iii) the EHRA score significantly improved following ablation in AF patients; and (vi) the rate of major complications was 0%.
Coronavirus disease 2019 epidemic and cardiac arrhythmias
Among the 83 022 cases reported in China as of 1 June 2020, 1716 health care workers became infected, of which 14.6% were severe.9 Moreover, a previous study10 of 138 in-hospital COVID-19 patients showed a 41.3% in-hospital infection rate of patient-to-patient transmission. A narrative review showed a rate of 40% to 45% of asymptomatic persons in all SARS-CoV-2 infections,11 warning that patients can be asymptomatic on admission but present with cardiovascular symptoms. The data above demonstrated that both patients and health care workers faced great danger due to nosocomial infection.
Meanwhile, exposure to COVID-19 caused a high incidence of arrhythmia. Wang et al.10 reported that 16.7% of 138 hospitalized COVID-19 patients developed arrhythmia, which was ranked second in COVID-19 complications. Moreover, arrhythmia was observed in 44% of COVID-19 patients who were admitted to an ICU in another study,12 which could increase the risk of death in infected patients.
In preparation for the COVID-19 pandemic, many health care providers had to scale down outpatient services, defer elective cardiac procedures and surgeries, and decline or delay acute cardiac emergencies.6 With a total of 673 cases reported,3 the Shanghai epidemic was not as severe as that of Wuhan. A recent study regarding the clinical progression of patients with COVID-19 in Shanghai showed that 90% of 249 cases were mild as evidenced by relatively low rates of ICU admission and high cure rate.13 Thus, compared with the severity of COVID-19, the impact of such medical strategies may extend beyond the epidemic and contribute to cardiac mortality.
Prevention strategies in the perioperative period
Chinese Society of Cardiology (CSC) expert consensus on the management of severe emergent cardiovascular diseases during the COVID-19 epidemic9 considered both the prevention and control of COVID-19 transmission to be of highest priority, having preference for conservative medical therapy and strict measures in limiting spread of infection within the hospital and among health care workers. However, Chinese expert consensus did not cover ordinary non-emergency cardiovascular diseases including common arrhythmia diseases such as AF, which has high disease incidence and may reduce the quality of daily life with potential risks.14
By obeying the principle of the CSC expert consensus,9 this study attempted to adopt a new workflow for catheter ablation in arrhythmia.
In the present study, CT was used as the first line in imaging screening. In China, patients were encouraged to present to hospital early for diagnosis as a form of public health measure. During the early stages of COVID-19, CT was preferred over chest radiography, as CT is more likely to be diagnostic than early chest radiographs.15 False-negative radiographs may be present, as chest radiographs can be normal in certain patients with clinically diagnosed or diagnosed COVID-19 pneumonia by CT.16 In many other countries such as the USA and UK, however, patients with early disease are encouraged to stay at home and to present to hospital only if symptoms progress.15 At this later stage, chances are higher in detecting COVID-19 changes on chest radiography.15 Moreover, in low resource settings, chest radiography may be more readily available than CT.17
Considering the incubation period of COVID-19, a 14 day isolation period was established as recommended by the Chinese Clinical guideline for COVID-19 diagnosis and treatment (7th edition).18 However, those with asymptomatic infection may still carry the virus. Wan et al.19 discovered two asymptomatic infections among 78 laboratory-confirmed patients, one of whom remained RT-PCR positive on the 15th day. Thus, SARS-CoV-2 nucleic acid detection testing was required in order to minimize the possibility of infection.
During hospitalization, the use of personal protection equipment served as the most important prevention measure. Wearing masks was strongly emphasized so as to control respiratory infections within the hospital for both patients and health care workers, which was found to reduce the infection rate by 87%.20 When wearing a mask, the metal wire should be placed on the bridge of the nose and moulded until it completely seals the contour of the bridge of the nose. Patients should avoid touching the outer surface of the mask when removing the mask after use, employing hand hygiene afterward, which is essential during hospitalization. A meta-analysis of 30 studies21 suggested that the use of nonantibacterial soap alongside hand hygiene educational interventions was efficacious in preventing gastrointestinal and respiratory illnesses.
Clinical outcome of catheter ablation during coronavirus disease 2019
The success rate of catheter ablation in the present study was 95.9%, with AF being 94.6%, VT and VPC being 98.0%, and others being 100%, which are similar to those of previous studies.22-24 Catheter ablation is known to reduce symptoms and improve quality of life.25 In the present study, symptoms evaluated by the EHRA score were reduced from three to one in AF patients, indicating that catheter ablation during the COVID-19 epidemic was effective. In addition, the low complication and infection rate illustrated the safety of catheter ablation.
The infection rate of COVID-19 was 0% at our centre, although fever remained during hospitalization following catheter ablation in certain cases. Fever has a better sensitivity to specificity for COVID-19. A previous study26 reported that 30 of 370 patients (8%) developed fever within 24 h following AF ablation. Such causes of fever include atelectasis, pneumonitis, pericarditis, haematoma at the access site, venous thromboembolism, thrombophlebitis, and, rarely, oesophageal injury. However, the possibility of COVID-19 infection seems less likely in these patients as strict screening was carried out prior to admission. Furthermore, three patients having fever after ablation were confirmed to be SARS-CoV-2 negative; hence, fever may be a stress response of ablation.
Limitations
Various limitations exist in the present study. First, the data were taken from a single institution, and the retrospective study design did not have the effect of prospective design owing to possible bias. Although the results might be typical and applicable in some areas like Shanghai, studies analysing larger patient populations require further analysis. Second, the epidemic is constantly evolving and changing. Once the infection population greatly increases, the impact of COVID-19 would be more serious than arrhythmia, making the present workflow inapplicable. Finally, data from longer follow-up periods and larger populations are necessary to further support this study.
Conclusions
The high severity of the COVID-19 pandemic has caused increased risk of infection for both patients and health care workers. By adopting strict risk assessment and careful infection prevention, however, catheter ablation in patients with arrhythmia can be safely and effectively performed in well-controlled areas during the COVID-19 epidemic. The proposed management may also be useful for cardiac electrophysiology doctors in response to the COVID-19 outbreak.
Conflict of Interest
None declared.
Funding
This work was supported by the National Natural Science Foundation of China (Grant Numbers 81400246 and 81770324) and Program of Shanghai Academic Research Leader.