Survival and outcome of retinoblastoma treated by neo-adjuvant chemotherapy in India
Abstract
Background
Retinoblastoma is the most common intraocular malignancy during infancy and childhood. The survival rate for children with retinoblastoma has improved significantly in developed countries; however, the outcome of the disease in developing countries remains dismal. Neoadjuvant chemotherapy is useful in this clinical scenario and can improve the survival of these children in the developing and underdeveloped countries.
Aim
To study the outcome and related factors in retinoblastoma patients treated at a tertiary care hospital in northern India.
Methods and Results
A tertiary care center-based retrospective study was done from the year 2009 to 2015. All patients underwent an examination under anesthesia and classified using International Classification of Retinoblastoma. All subjects received systemic chemotherapy and, additionally, local surgical therapy according to the stage of the disease. Extraocular presentation and/or residual/recurrent tumour was treated by radiotherapy. All the subjects who followed the treatment protocol were included in the study. Two hundred and forty-seven eyes of 200 subjects were included after screening the records of 233 subjects, who presented with retinoblastoma from January 2009 until December 2015. Mortality rate was highest in Group E (n = 50, 42.0%) followed by Group D (n = 24, 33.8%), whereas there was no mortality in unilateral Group B and Group C. Total 126 (63.0%) patients were alive at the end of the study. Factors significantly associated with mortality were age at the time of diagnosis, latency in the diagnosis, and the stage of the disease at presentation.
Conclusions
Neo-adjuvant chemotherapy shows promising results in terms of low recurrence rates. Latency in diagnosis, higher age at presentation, and advanced disease at presentation were associated with higher mortality. Subjects with early presentation had a favourable outcome, and cure was possible after completion of the therapy.
1 INTRODUCTION
Retinoblastoma is the most common intraocular malignancy during infancy and childhood,1-4 Untreated retinoblastoma has high rate of mortality due to systemic metastasis with disease progression. Mortality in retinoblastoma is related to the primary tumour metastasis and also due to vulnerability to have secondary malignancies due to the underlying gene defect and ionizing radiation used as a treatment modality.
In developed countries, prognosis of retinoblastoma has considerably improved over the past several decades.5 However, in developing and underdeveloped regions of the world, the survival rates are still not satisfactory due to various reasons that include socioeconomic conditions of patients and quality of health care services.6-10
The neoadjuvant chemotherapy, which consists of chemotherapy for reduction of tumor load followed by enucleation, provides good cure rates as it takes care of any systemic metastasis.11-16
- After achieving downstaging, a smaller tumor implies a less aggressive surgical management. In a tissue as vital as the eye, this has significant consequences. Often, it is possible to conserve the sight or the globe which would be unsalvageable if surgical therapy was performed at the outset.15, 17
- It is expected to reduce the micrometastasis during surgery.
-
Hospital stay during neo-adjuvant chemotherapy has other unintended advantages
- Malnourished children are often poor candidates for surgery under general anesthesia, and dietary advice and supervision give an opportunity to improve the general health of the patients.
- It also serves to sensitize the parents to give consent for enucleation after they have witnessed other children with the similar disease and having improvement with the treatment.18
2 METHODS AND MATERIAL
Records of patients who presented with retinoblastoma at King George's Medical University, Lucknow, India, since the year 2009 (when neo-adjuvant chemotherapy was introduced) till the year 2015 were screened, and candidates who completed the treatment protocol were included in the study. The institutional ethical committee was notified of the same, and approval for the same was received before starting the study. Study followed the tenets of the Declaration of Helsinki.
Records of the subjects were processed to include demographic information, history, clinical features, treatment delivered, adherence to treatment protocol, eye salvage, visual function salvage, survival/mortality outcomes, and duration of follow-up. This information was used to classify the subjects according to International Classification of Retinoblastoma.19, 20
The management was done using multimodality approach by collaboration between the Departments of Ophthalmology, pediatrics (oncology unit), radiotherapy, and prosthodontics (for cosmetic rehabilitation). Diagnosis and classification were based on clinical evaluation under general anesthesia, ultrasonography of the orbit, and computed tomography of the orbit and skull. Cerebrospinal fluid cytology was done in all subjects, and bone marrow examination was done only in cases with the extraocular spread.
Standard six cycles of Vincristine, Etoposide, and Carboplatin21 systemic chemotherapy were given to all the patients soon after clinico-radiological confirmation of the disease. LASER therapy or cryotherapy was given to the patients classified under group A and group B with disease amenable to local therapy. For patients under group C and group D, enucleation was done after four chemotherapy cycles, and subsequently, the remaining two chemotherapy cycles were delivered.
In extraocular retinoblastoma at presentation, surgical decision was made after clinical and radiological evaluation performed after four chemotherapy cycles. Those patients who had no evidence of orbital metastasis (down-staging) were treated by enucleation and others by exenteration.
The mentioned protocol was altered, and a relatively conservative approach was practiced for subjects with bilateral disease so as to preserve the better eye with the possibility of vision.
The cure was defined as clinical and radiological freedom from a tumor after 1 year of cessation of therapy.
Data were analyzed using Medcalc (Version 14.8.1). Descriptive statistics were used as needed. Categorical variables were compared using the χ2/Fisher's exact tests. Kaplan-Meier survival analysis was carried out to study the survival pattern among different groups. A P-value <0.05 was considered statistically significant.
3 RESULTS
3.1 Epidemiology and clinical features
A total of 233 patients were diagnosed to have retinoblastoma during the 6-year period from January 2009 until December 2015. Thirty-three patients (13.7%) who abandoned the therapy and did not return for follow-up were excluded. Thus, 200 patients who completed the treatment and were under regular follow-up were included in the study.
The epidemiological data and clinical features at presentation have been summarised in Tables 1 and 2. Overall, unilateral cases presented with relatively advanced stage of retinoblastoma when compared with bilateral cases, and this difference was statistically significant (Chi-squared test P = 0.008).
| Including All Patients (N = 200) | Male (n = 118) | Female (n = 82) | P-Value | Unilateral (n = 152, 76%) | Bilateral (n = 48, 24%) | P-Value | Intraocular (n = 118, 59%) | Extraocular (n = 82, 41%) | P-Value | |
|---|---|---|---|---|---|---|---|---|---|---|
| Median age (months) at first sign (average, range) | 27.0 (35.2, 0-178) | 27.5 (36.7, 0-178) | 24.0 (33.1, 0-168) | 0.39 | 30.5 (38.5, 0-178) | 18 (24.8, 0-128) | 0.01 | 24.5(35.3, 0-178) | 28.5 (35.0, 0-170) | 0.68 |
| Median age (months) at presentation (average, range) | 33.0 (42.2, 0-182) | 35.0 (43.3, 1-182) | 31 (40.7, 0-172) | 0.46 | 37.0 (46.3, 0-182) | 24 (29.1, 0-131) | 0.0008 | 29.0 (41.1, 0-182) | 37.0 (43.6, 3-171) | 0.17 |
| Median lag period (months) (average, range) | 3.0 (7.0, 0-88) | 3.0 (6.6, 0-65) | 3.0 (7.6, 0-88) | 0.78 | 3 (7.8, 0-88) | 2(4.4, 0-24) | 0.04 | 2.0 (5.8, 0-65) | 5(8.6, 0-88) | 0.0003 |
| Male (%) | 118 (59) | – | – | – | 91 (77.1) | 27 (22.9) | 0.78 | 66(55.9) | 52 (44.1) | 0.36 |
| Female (%) | 82 (41) | – | – | – | 61 (74.4) | 21 (25.6) | 52 (63.4 | 30 (36.6) | ||
| Unilateral (%) | 152 (76) | – | – | – | – | – | – | 86 (72.9) | 66 (80.5) | 0.28 |
| Bilateral (%) | 48 (24) | – | – | – | – | 32 (27.1) | 16 (19.5) |
| Presenting Symptomsa | Number of Patients | Percentage | Average Age at First Sign (Median Age) | P-Value (Kruskal-Wallis Test) | Average Age at Diagnosis (Median Age) | P-Value (Kruskal-Wallis Test) | Average Lag Time for Diagnosis (Median Age) | P-Value (Kruskal-Wallis Test) |
|---|---|---|---|---|---|---|---|---|
| Leukocoria | 148 | 74% | 34.39 (26.0) | <0.001 | 41.70 (31.5) | 0.007 | 7.33 (3.0) | 0.49 |
| Squint | 19 | 9.50% | 13.47 (9.0) | 23.05 (23.0) | 4.33 (6.0) | |||
| Red eye | 24 | 12.00% | 50.75 (43.5) | 55.08 (50.0) | 4.33 (2.5) | |||
| Proptosis | 9 | 4.50% | 53.44 (24.0) | 57.77 (31.0) | 9.57(4.0) |
- a Primary and most prominent symptom.
- The bold font is used in this table to signify significant p value.
There was a significant increase in the number of subjects with extraocular disease from nine cases with protrusion as the first symptom seen to 82 cases with extraocular extension radiologically/clinically at the time of patient registration. The median latency in diagnosis from the first symptom was 5 months in the extraocular presentation and 2 months in the intra-ocular retinoblastoma subjects; this difference was statistically significant (Mann-Whitney test P = 0.0003) (Table 1). Thus, the delay in the presentation may be one of the reasons which caused conversion of intra-ocular disease to extraocular.
Ophthalmologists diagnosed most of the patients (n = 170, 94.1%). The family history of cancer was present in eight (4.0%) patients, and there was no statistical difference in the age at which the diagnosis was made between these and those with a negative family history (Mann-Whitney test P = 0.78).
There were total 248 eyes of 200 subjects, and half of the eyes were in Group E classification or worse (124, 50.0%), 89 (35.88%) in Group D, 9 (3.6%) in Group C, 15 (6.04%) in Group B, and 11 (4.43%) in Group A.
3.2 Treatment
Apart from standard six cycles of neo-adjuvant chemotherapy (Vincristine, Etoposide, and Carboplatin) given to all the subjects, 208 (83.46%) eyes out of total 248 eyes (of 200 subjects) were treated by enucleation, 34 (13.7%) eyes received focal treatment in the form of LASER/Cryotherapy, and 6 (2.4%) cases required exenteration. Radiotherapy was administered to 21 children with residual orbital disease. All the eyes in group A and B were saved from enucleation, whereas only one eye (11.1%) in group C was salvageable out of nine eyes. All eyes with Group D and E or worse were treated by removal of the eyeball. There were 98 (39.51%) eyes (82 patients) out of 248 eyes with extraocular spread at the time of diagnosis, but only six (6.1%) out of these eyes needed exentration after neo-adjuvant chemotherapy. This was a major advantage of neo-adjuvant chemotherapy, due to which a disfiguring surgery was avoided.
3.3 Survival and mortality-related factors
The average follow-up of these 200 subjects was 45.79 months (SD 21.7, range 7-111 months). During the study period, 74 subjects (37.0%) out of total 200 subjects died due to retinoblastoma related complications.
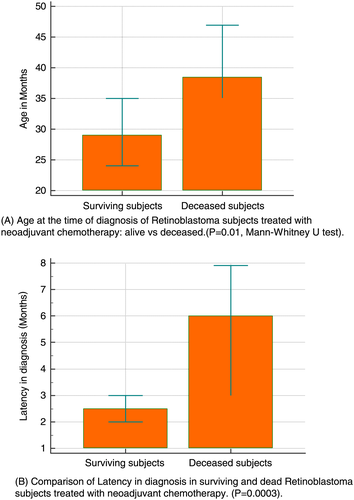
There was a statistically significant difference in the median age at diagnosis and median latency in the diagnosis among the subjects who died and those who survived (Mann-Whitney test P = 0.01 and P = 0.0003, respectively, Figure 1A,B). There was a relative risk of 1.49 of death among subjects with extraocular disease at the time of presentation, and this was statistically significant (P = 0.02). However, the age at which the first sign appeared was not significantly different among the surviving and deceased subjects (Mann-Whitney test P = 0.28) (Table 3). Thus, the factors affecting the survival of the subjects were mainly age at diagnosis, latency in diagnosis, and extraocular disease at the time of diagnosis. The association between these variables and the significance levels is shown in Tables 3 and 4.
| Including All Patients (N = 200) | Alive (n = 126, 63.0%) | Dead n = 74, 37%) | P-Value (Mann–Whitney Test) | |
|---|---|---|---|---|
| Median age at first sign in months (average, range) | 27.0 (35.2, 0–178) | 24.0 (34.7, 0-178) | 35 (36.0, 0-151) | 0.28 |
| Median age at diagnosis in months (average, range) | 33.0 (42.2, 0-182) | 29 (40.32, 0-182) | 38.5 (45.5, 1-168) | 0.01 |
| Median latency in diagnosis in months (average, range) | 3.0 (7.0, 0-88) | 2.5 (5.6, 0-88) | 6 (9.5, 0-54) | 0.0003 |
- The bold font is used in this table to signify significant p value.
| Including All Patients (N = 200) | Alive (n = 126, 63.0%) | Dead (n = 74, 37%) | Relative Risk | P-Value | |
|---|---|---|---|---|---|
| Intra-ocular disease | 118 (59) | 78 | 34 | 1.49 | 0.02 |
| Extra-ocular disease | 82 (41) | 48 | 40 | ||
| Unilateral disease | 152 (76) | 93 | 59 | 0.8 | 0.36 |
| Bilateral disease | 48 (24) | 33 | 15 | ||
| Male gender | 118 (59) | 74 | 44 | 1.01 | 0.91 |
| Female gender | 82 (41) | 52 | 30 |
- The bold font is used in this table to signify significant p value.
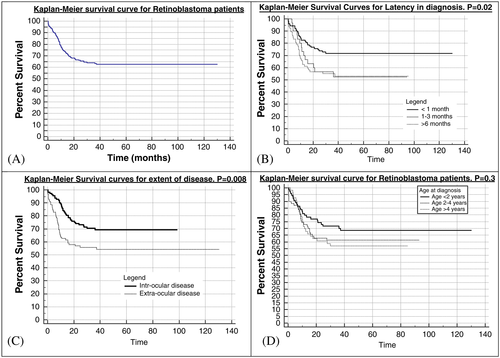
Overall survival probability as per Kaplan-Meier survival analysis at 1, 2, 3, and 5 years was 74%, 65.5%, 63.3%, and 62.2%, respectively (Figure 2A). The Kaplan-Meier survival analysis showed statistically significant and favorable survival probability for patients with less than 1 month of latency in diagnosis (P = 0.02) (Figure 2B), than those with intraocular disease at the time of presentation (P = 0.008) (Figure 2C), or those who presented before the age of 2 years (P = 0.3) (Figure 2D).
Mortality among males was 44 (37.3%) and those among females was 30 (36.6%), and this difference was insignificant (Chi-squared test, P = 0.96).
Out of total 48 patients with bilateral disease, 15 (31.9%) died, while out of 152 patients with unilateral disease, 59 subjects (38.6%) died (relative risk 0.80, P = 0.36). Four out of eight patients (50%) with family history of cancer died, while there were 70 deaths among 192 subjects (36.45%) with no family history of malignancy (relative risk of 0.72, P = 0.388).
There were no deaths in the unilateral group B, and C, while in the group D 24 (33.8%) patients died out of 71 and in the group E 50 subjects (42.0%) died out of 119 subjects (P = 0.05, Chi-squared test). At the time of reporting, out of 200 patients, 126 (63.0%) patients were alive after 2 years of completing the treatment, and 74 (37%) patients died during treatment.
4 DISCUSSION
Our study spanning over a time of 6 years and ending in December 2015 included the records of 200 subjects and 248 eyes of patients who completed the study protocol in Northern India. There was a preponderance of male subjects, which is common in all reported data in the literature.7, 22-27
The median age at diagnosis was 33 months, and majority become clinically apparent before the age of 4 years. This was higher when compared with other studies from Asia, which report the average/median age at diagnosis from 22 months to 29 months. 22, 23, 28-30 However, this is better when compared with reports from the African continent where the median age at diagnosis was 36 months (Ghana) and 37.5 months (Kenya).24, 25The onset of symptoms was at the median age of 27 months, and the bilateral cases had an earlier onset of symptoms when compared with unilateral cases which are in agreement with other studies.20-22, 31We had 24.0% bilateral and 76.0% unilateral retinoblastoma cases, which is in agreement with another study from north India.21
One of the major factors affecting the disease status at presentation was the lag period (median 3 months) from the first symptom till the presentation. This lag period was not affected by the gender of the child; however, the subjects with unilateral disease and extraocular disease at the time of presentation had a greater lag period. This can be interpreted as delay in seeking medical care due to various reasons (negligence, poor awareness, non-availability of health care facilities, personal beliefs etc.). The lag period in our study was comparable to other studies from India and China.21, 22, 28
The proportion of cases with the extraocular disease in our study was 41%, which was significantly higher than the developed world (less than 5%).32 This is comparable to the reports from developing (Taiwan, Malaysia) and underdeveloped regions (Ghana) of the world which ranges from 26% to 50%.20, 26, 30 Major reasons for late presentation with advanced disease include lack of awareness, inadequate healthcare facilities, unreliable referral system, delay in seeking health care by the guardians, and poor compliance to treatment because of fear of morbidity and treatment failure.8
In our study leukocoria was the most common symptom at presentation which is universally seen in all the studies.33 However, the second most common symptom was redness of the eye and pain which indicates secondary glaucoma due to extensive intraocular spread, which is in contrast to developed nations where the second most common symptom is strabismus.
The majority (~75%) of children had unilateral disease in our study. Bilateral cases were reported earlier than the unilateral cases, which is commonly seen phenomenon worldwide (the USA,34 Australia, and UK,9 China35). However, the median age at presentation for both unilateral and bilateral cases was higher than developed countries.
Majority of early intraocular disease (International Classification of Retinoblastoma Group A and B) were the eyes with incidental findings in the contralateral eye of presenting eye. Thus, no case in the group A disease, and only 1/5 eyes in the group B had unilateral disease. Our observation of identifying less advanced disease more often in bilateral RB is consistent with that reported by Zhao et al34 in Chinese children.
Untreated retinoblastoma is always fatal. With early detection and improved treatment modalities, the prognosis of the patients has improved significantly. It has a survival rate of 95% to 98% in developed countries and 50% worldwide.36 In our study, the survival was 63%, which is better than the reports from African countries and at par with Asian nations.7, 29 One of the major reasons of discrepancy in survival rates between the developed nations and our study is that in our population extraocular retinoblastoma at presentation was seen in 41% of cases, while in a study from the UK,33 the extraocular disease was seen in only 1.6% of their retinoblastoma population.
The survival probability in our population at 1, 2, and 5 years was 74%, 65.5%, and 62.6%, which is comparable to another study in India by Chawla et al.21
The association between the age at diagnosis and mortality has been established by various studies in India28, 29 and other countries.22, 23 The subjects who survived had significantly lower age at the time of diagnosis as compared with those who died. Latency in diagnosis is another factor affecting the survival of these patients significantly. This is because increased latency causes disease progression and metastasis at the time of presentation. This is in agreement with other studies from India and China as well which have reported significant delay in presentation.20, 21
There was no relation to the gender of patients and mortality rates in our study, although an earlier study reported the better outcome in male children.26 Mortality rate was slightly lower (31.2%) in bilateral cases as compared with unilateral cases (38.8%), but this was not significant. This may be because of earlier presentation of bilateral cases as compared with unilateral cases.
The high rate of treatment by enucleation (83.8%) of the eye is mainly due to advanced disease at the time of presentation and is desirable as these eyes have no visual potential and high chances of metastasis. Similar reports are from other studies with a high proportion of group D and E at the time of presentation.21, 34 It is interesting to see that although the extra-ocular retinoblastoma was seen in 82 (40%), out of total subjects at the time of presentation but only six (3%) subjects needed exenteration. This is because of down staging achieved by the neo-adjuvant chemotherapy. Thus, in majority of extra-ocular retinoblastoma, we were able to avoid disfiguring surgery with the help of neo-adjuvant chemotherapy.
All the retinoblastoma affected eyes in group A and B were preserved (11/11 and 15/15) and 88.9% of group C (8/9) were preserved with some visual potential. All the eyes in group D and group E were removed as per the treatment plan. This outcome is different from other reports where nearly all eyes were preserved in the group A, B, and C, and additionally nearly half the eyes were preserved in group D.15, 21
We found out that the mortality rate was highest in Group E (50, 42.0%) followed by Group D (24, 33.8%) and there was no mortality in less extensive disease. The mortality distribution as per the retinoblastoma group was statistically significant with P-value of 0.05.
Multivariate analysis showed that the increased latency period in the diagnosis and stage of the disease at the time of diagnosis were the factors significantly associated with mortality in our cohort. This is in partial agreement with the studies in India, Taiwan, and Uganda which quote stage of the disease as the main factor for mortality as per multivariate analysis.20, 21, 27
A previous study had concluded that chemotherapy given before enucleation of group E eyes masked pathologic evidence of extraocular extension. This increased the risk of metastatic death from reduced surveillance and inappropriate management of high-risk disease, especially if enucleation was performed longer than 3 months after diagnosis.37 However, a letter to the editor referring to this article questions the conclusions of this study by Zhao J et al and quotes that the title and conclusion “might be potentially misleading for treating physicians, especially in less developed countries, who might interpret from it that initial enucleation should be attempted in all patients with advanced retinoblastoma, including those with different degrees of orbital dissemination.”38 The commentary also mentions that the neoadjuvant chemotherapy helps in avoiding exenteration, triggers chemoreduction of the contralateral eye disease (in bilateral cases), and sensitizes the guardians to provide consent for enucleation.
In summary, presentation of advanced retinoblastoma is frequently observed in India and may be attributed to increased latency in diagnosis. This results in high proportion of eyes being managed by enucleation. Advanced disease also causes extra-ocular spread at the time of presentation and increased possibility of local and distant metastasis. This correlates with low survival rates in these children, which necessitates the use of neo-adjuvant chemotherapy to downgrade the tumour, thereafter allowing safe eradication of tumour by enucleation and avoiding exenteration. On the other hand, children presenting with early disease have eye salvage and survival rates comparable to other parts of the world. Apparently increased general awareness, early diagnosis, better access, and compliance to therapy can improve the outcome of these children both in terms of eye salvage and survival.
ACKNOWLEDGMENTS
We acknowledge the contribution of Mr Pawan Kumar Mishra for typing the manuscript and doing data consolidation and validation.
SOURCE (S) OF SUPPORT
None.
PRESENTATION AT A MEETING
None.
CONFLICTS OF INTERESTS
None declared.
AUTHORS' CONTRIBUTION
All authors had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Conceptualization, S.K.G.; Methodology, S.K.G., M.M., A.K.; Investigation, S.K.G., M.M., Ar.K., N.V.; Formal Analysis, S.K.G., M.M., Aj.K.; Resources, S.K.G., Ar.K., N.V.; Writing—Original Draft, M.M., Aj.K.; Writing—Review & Editing, S.K.G., Aj.K., S.A., N.V.; Visualization, S.K.G., M.M.; Supervision, S.K.G., A.K.