A Multidisciplinary Approach to Hypermobility Spectrum Disorder, Raynaud's Phenomenon, and Biomechanical Soft Tissue Injuries in an Adolescent Boy: A Case Report
Funding: The authors received no specific funding for this work.
ABSTRACT
A 16-year-old male with hypermobility spectrum disorder (HSD) and Raynaud's phenomenon (RP) was referred to a clinical exercise physiologist (CEP) by their pediatric rheumatologist. The patient presented with arthralgia in the left knee and shoulder. Specifically, the left knee presented discomfort during activities of daily living (ADL), and the left shoulder had a reduced range of motion resulting from pain. Finally, complaints of painful fingers were also significant due to increased RP flare-ups during winter. A posture analysis was conducted, indicating relatively poor posture. Range of motion and manual muscle testing were suboptimal in the shoulders, but optimal in the knees and hips. The Kendal test, patella compression test, and Clarke's sign were conducted due to knee pain. Functional tests included a pelvic bridge, squat, Neer's test, and wall push-up. Finally, the modified pediatric clinical test of sensory interaction in balance (mPCTSIB) was completed to determine the interaction between balance systems. Analysis of all the tests conducted above confirmed the diagnosis of HSD and also indicated scapula dyskinesia, supraspinatus impingement, and patellofemoral pain syndrome. Consequently, the CEP treatment focused on strengthening the foot, knee, and hip kinetic chain, as a 12-week home program, along with hand exercises as needed to aid in the pain and stiffness experienced during RP flare-ups. The physiotherapist treatment was more hands on in the use of myofascial release, electrotherapy, taping, and posture correction of the neck and shoulder over four in-house visits. Finally, a 6-month follow-up was conducted by the CEP, in which the patient showed improvement with a pain-free range of motion and the ability to optimally conduct ADLs.
Summary
- Hypermobility spectrum disorder (HSD) is associated with other connective tissue disorders, such as Raynaud's phenomenon (RP) and biomechanical restrictions.
- Appropriate, individualized physical assessment can provide clear guidelines for deficits and individualized exercise prescriptions.
- As a home-based program, exercise therapy can assist with pain management and reduce biomechanical restrictions.
1 Introduction
Hypermobility spectrum disorder (HSD) and Raynaud's phenomenon (RP) both impact connective tissue, with HSD resulting in joint hypermobility, impacting ligaments, tendons, and muscles [1-5]. In the case of RP, the blood vessels' connective tissue are dysfunctional, resulting in poor circulation to the extremities of the hands and feet. All ethnic and age groups are affected by HSD, but a suspected higher prevalence exists in children and adolescents, females, Asians, and West Africans [2]. The suspected prevalence in Africa for children and adolescents is five to 18%, with prevalence reducing with age [4]. HSD is largely undiagnosed with a lack of epidemiological studies, especially in sub-Saharan Africa [2]. The prevalence of RP in the pediatric population is unknown but suspected to be rare and more predominant in females aged 12 to 15 [6].
Joint hypermobility (JHM) is a common clinical feature of HSD and is the ability of a joint to move beyond the optimal limits of the physiological axes [5]. Critically, there is a differentiation between localized and generalized JHM, with the latter likely associated with genetic markers. HSD is diagnosed when the 2017 International Classification of the Ehlers-Danlos Syndromes (ICEDS) criteria for hypermobile Ehlers-Danlos syndrome is not satisfied in a patient with symptomatic JHM. HSD's pathophysiology is relatively unknown and has a variable clinical presentation, with little guidance on associated biomarkers and a single pathophysiological mechanism. Instead, a host of genetic and environmental factors can contribute to HSD. Environmental factors particularly refer to repetitive microtrauma at an affected excessively lax joint that alters kinematics and proprioception, overloading joints on either side of the kinetic chain, resulting in associated arthralgia and diffused musculoskeletal pain [2].
RP is associated with an episodic response to cold weather and emotional stress, particularly in primary RP [6-8]. Secondary RP is associated with an already existing connective tissue disorder, requiring laboratory testing for antinuclear antibodies and physical assessments including nail capillaroscopy [7, 8]. Episodic spasms in both primary and secondary RP results in a triphasic color response of extremities such as fingers and toes and, in rare cases, the nose, ears, and tongue [7]. Vasospasms of the arteries and arterioles occur, causing a pallor (white) appearance, followed by dilation of the capillaries and venous stasis, causing cyanosis (blue). Finally, arteries and arterioles dilate, causing reactive hyperemia (red) [8]. A biphasic color appearance can also occur. Not only are there color signs but also symptoms of pain and tingling can be reported.
The current case report is of value in the global context to the pediatric cohort. Crucially, the case demonstrates a unique combination of HSD and RP, not previously reported on. Not only are the combination of diagnoses unique, but the presentation and signs and symptoms also carry novelty. Additionally, the diagnoses of biomechanical soft tissue injuries along with the HSD and RP increase the case's uniqueness and have not been reported globally. The case is also noteworthy due to the multidisciplinary nature of the treatment provided, with each healthcare profession implementing their scope of treatment ranging from pharmacological intervention to manual therapy and exercise prescription.
2 Case Presentation
2.1 Patient Information
An adolescent boy presented to a tertiary hospital in the Western Cape in 2018 with painful hands that occasionally swell, itch, and blister with a complaint of difficulty opening bottle tops. These symptoms improved during the summer, with fewer days of complaints. Additionally, marfanoid features such as elongated limbs and torso, tall for age, greater arm span to height, arachnodactyly, pes planus, and hypermobility were noted. Otherwise, the patient was generally healthy, except for atopic asthma, rhinitis, and mild eczema. At the time of this presentation, the patient was age 13, with a height of 170 cm (cm) and a weight of 51.2 kg (kg), a blood pressure (BP) of 136/64 mmHg, and a heart rate of 67 beats per minute (bpm).
In August 2021, the head pediatric rheumatologist referred the now 16-year-old boy to the new clinic biokineticist (clinical exercise physiologist [CEP]) for pain management and joint strengthening. Simultaneously, his private general physician referred the boy to a physiotherapist for left shoulder pain. Through the initial consultation, subjective historical evidence included no cardiovascular complications, no temporomandibular joint discomfort, no history of joint subluxation or dislocation, use of eye spectacles for digital screens, no smoking, and a total of 70 min of low to moderate physical activity per week. Familial history included direct relative diabetes mellitus type two (DMTII) and hypertension. Additionally, the patient stated his goal was overall pain management. Upon examination, HSD could be confirmed using the Brighton Criteria including a Beighton Score of four (major criteria), arthralgia in two joints in the past three months (minor criteria), soft tissue lesions in one joint (minor criteria), and Marfan-like habitus (minor criteria). Finally, the patient's hands also presented cold with white discoloration, as related to RP and as reported by the pediatric rheumatologist.
2.2 Initial Examination
2.2.1 Physiotherapy
Upon the patient's first visit to the physiotherapist, patient history was taken, and a physical assessment was conducted on the left shoulder and cervical spine. History questions revealed that the patient suffered from left shoulder pain and enjoyed being in front of his laptop for leisure and study. Furthermore, the patient reported no sports involvement. The first physical evaluation revealed reduced muscle bulk, with a generally poor posture related to a forward neck, elevated left shoulder, and left scapula winging.
Palpation, range of motion (ROM), manual muscle testing (MMT), and special tests were conducted on the left shoulder and cervical spine. Palpation revealed upper trapezius trigger points, a tender middle trapezius and teres minor, and tight pectoralis major and minor muscles. The ROM on the left in abduction and shoulder flexion was suboptimal. Cervical side flexion only achieved two-thirds of the optimal range, with pain in the left cervical region. Furthermore, cervical rotation had optimal ROM, but the pain was produced at the end range to the left side. Weak deep neck flexors, weak left rhomboids, and weak left levator scapulae presented with MMT. Generally, the scapulae bilaterally had poor positioning and setting.
2.2.2 Biokinetics
Upon the patient's initial visit, patient's personal data, consent, and a Physical Activity Readiness Questionnaire (PARQ) were conducted. The PARQ indicated dizziness was experienced twice in the past 12 months, the conditions in question, medication usage, and most importantly, medical clearance from the patient's physician was achieved (as referred). Medication used by the patient included Avamys and Desalex for asthma and rhinitis, as well as Nifedipine for controlling RP. The patient was also provided with the Pediatric Rheumatology Quality of Life Scale (PRQL), for which he scored 16 out of 30, with his physical health (10/15) being more negatively impacted than his psychological health (6/15). Finally, and most importantly, the patient was asked about their personal goal, which was identified as whole-body pain management.
Anthropometric data and a detailed posture analysis were conducted. A weight of 55.5 kgs and a height of 180 cm gave a BMI of 17.1 kg/m2, which is underweight for the age and sex, as it is within the 5th percentile. Wingspan was also measured to be 186.8 cm, giving a wingspan-to-height ratio of 1.04. As part of anthropometric data, leg length was also measured, and found to be equal bilaterally. The postural analysis was initiated from the feet up toward the head. Various observations and palpations were made, with the consequent findings tabulated in Table 1.
| Postural analysis with observation and palpation of various bony structures and muscle interties | |
|---|---|
| Anterior view | Bilateral navicular bulge bilaterally |
| Pes planus and Pes valgus | |
| Right inferior medial patella pain upon palpation. Palpation tenderness above the Pes anserinas | |
| Right increased vastus lateralis muscle tonus compared to the left | |
| Reduced vastus medilais oblique muscle mass bilaterally | |
| Pectus excavatum | |
| Raised left shoulder in height compared to the right | |
| Lateral view | Increased iliotibial band tightness bilaterally |
| Greater right anterior pelvic tilt at 11° and left at 10° | |
| Forward shoulder posture bilaterally | |
| Elongated neck | |
| Posterior view | Rearfoot valgus bilaterally (medial curve of the Achilles tendon) |
| Increased soleus muscle tonus bilaterally | |
| Tenderness on palpation of the right lateral head of the gastrocnemius and bilateral soleus | |
| Reduced bilateral hamstring tonus compared to the tonus of the quadricep muscles | |
| Type I and II scapula dyskinesia bilaterally | |
| Increased levator scapulae tonus bilaterally | |
| Tenderness on palpation across right rhomboid and middle trapezius | |
| Range of motion and manual muscle testing | ||||
|---|---|---|---|---|
| Test | Joint movement | Left | Right | Comments |
| Range of motion | Hip flexion | 100° | 97° | Pain bilaterally at end ROM |
| Knee flexion | 129° | 125° | ||
| Knee extension | 180° | 180° | Pain bilaterally at end ROM | |
| Shoulder abduction | 149° | 180° | ||
| Shoulder flexion | 160° | 180° | ||
| Manual muscle testing (Oxford scale) | Hip flexion | 4 | 4 | |
| Knee flexion | 5 | 5 | ||
| Knee extension | 5 | 5 | ||
| Shoulder abduction | 2 | 3 | The left shoulder had superior capsule pain from 25° onward combined with posterior capsule pain from 45° onward | |
| Shoulder flexion | 3 | 3 | Pain on the left from 45° onward | |
| Lower and upper extremity special tests | |||
|---|---|---|---|
| Test | Left | Right | Comment |
| Kendal | + | − | Testing on the right elicited pain in the left knee |
| Patella compression | + | − | Increased apprehension was observed from the patient during the conduction of both tests on the left side |
| Clarke's sign | + | − | |
| Empty can | + | + | Immediate pain felt on the left of VAS 7 and only at the end ROM on the right at VAS 3 |
| Belly press | − | − | |
| Hornblower's sign | + | + | Pain on the right was located at the teres minor insertion and on the left subjectively pain was reported as inside the capsule |
| 90° External rotation | + | + | |
| Modified pediatric clinical test of sensory interaction in balance | ||
|---|---|---|
| Condition | Stance duration (s) | Degree of sway |
| Stable surface with eyes open | 30 | 1 |
| Stable surface with eyes closed | 30 | 2 |
| Unstable surface with eyes open | 28 | 3 |
| Unstable surface with eyes closed | 5 | 4 |
Special tests and functional tests formed the bulk of the physical assessments to gain a greater understanding of the patient's ability to move and their body's interaction with the environment. Special tests consisted of a ROM, MMT, Beighton's Score, and various biomechanical special tests to understand biomechanical soft tissues. Functional tests consisted of the modified Pediatric Clinical Test of Sensory Integration in Balance (mPCTSIB), scapular humeral rhythm, pelvic bridges, wall push-ups, and squats. Raw data for ROM tests and MMT of joints that were bothersome to the patient can be found in Table 1.
History, posture analysis, ROM, and MMT formed the basis for decision-making on which special and functional tests needed to be conducted. Due to the consequent pain at the end of hip flexion and knee extension, the Kendal tests, patella compression test, and Clarke's sign (patellar grind test) were conducted, with outcomes present in Table 1. Furthermore, the integrity of patellar stability was assessed by moving the patella medially and laterally, which indicated increased patella instability as the patella moved laterally significantly. These tests suggest patellofemoral pain syndrome (PFPS), as associated with the risk factor of increased patellar laxity. Special tests done on the shoulder were to gain an understanding of the rotator cuff muscles' integrity to derive whether there is enough dynamic stability provided to the glenohumeral joint. The results of these tests can be seen in Table 1. Finally, the Beighton Score also revealed four out of nine hypermobility points to be present, namely bilaterally being able to pull the thumb toward the forearm and elbow extension greater than ten degrees bilaterally, which is in addition to a positive Walker-Murdoch and Steinberg sign bilaterally.
Functional tests conducted started with assessing balance, using the mPCTSIB with raw data present in Table 1. During the mPCTSIB, the left foot was the main foot balanced to gain an understanding of the proprioceptive ability of the left kinetic chain. Through interpretation of the results, it can be concluded that the patient is dependent mostly on their proprioceptive system, followed by their visual system, and least dependent on their vestibular system. Additionally, the patient may also struggle with sensory integration due to the increase in sway noted in the last three conditions.
Other biomechanical functional tests included observation of a pelvic bridge, squat, scapular humeral rhythm, and wall push-up. Ten repetitions of the pelvic bridge were done with a good technique, but the patient had shaky legs and reported difficulty completing the movement. When asked to extend the leg at the end of the pelvic bridge, a left hip drop was noted when the right leg was supported. During ten squats, it was observed that the patient is hip dominant, hence a greater bend at the torso than the knees, indicating more hamstring involvement than the quadriceps. Additionally, the feet were excessively externally rotated to perform the movement, with the medial arch dropping throughout the ten repetitions. When asked to perform the squat with the knees over the toes, the patient expressed discomfort in the left knee. The pelvic bridge and squat provided information that the quadriceps may be functionally weaker than the hamstrings and that the right gluteus medius does not provide enough pelvic stability. Reduced pelvic stability may also occur with a dropped medial arch during the squat.
The shoulder functional tests gave greater insight into the biomechanical constraint of the shoulder, namely poor dynamic shoulder stability and scapular dyskinesia. Poor scapular humeral rhythm indicates that the scapulae rotate upwards earlier than biomechanically expected. The upward rotation occurs around 30° of shoulder abduction when it should only aid shoulder movement beyond 45° of shoulder abduction. Furthermore, scapular winging occurs beyond 45° of shoulder abduction, indicating poor glenohumeral stabilization from the serratus anterior, with pain also occurring on the left from 45° onward. Scapular winging was also prominent during the wall push-up, with pain occurring during the push-off movement, particularly at the top around the anterior portion of the shoulder. Both the shoulder functional tests confirm type I and type II scapular dyskinesia and weak dynamic shoulder stability, particularly from the rotator cuffs and the serratus anterior.
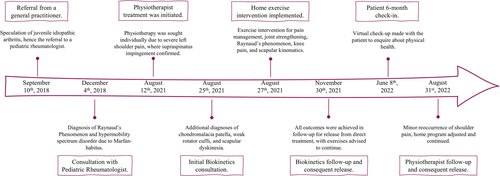
2.3 Timeline
A complete timeline of known patient participation is illustrated in Figure 1.
2.4 Therapeutic Intervention
2.4.1 Physiotherapy
Three physiotherapy sessions and home exercises were provided as treatment in 2021. The first session occurred on August 12, 2021, and consisted of myofascial release and electrotherapy of the upper trapezius. Next, stretches of the cervical muscles, scapula setting, and isometric strengthening of the rhomboids were implemented. Consequently, the patient was provided with a home program focusing on scapula setting and posture correction. On August 19, 2021, the second session was conducted with the finding of improved left shoulder abduction and discomfort. Manual therapy of the upper and middle trapezius was implemented, followed by Kinesio-taping of the scapula in relation to the shoulder. After taping, scapula stability against the wall and isotonic strengthening of the rhomboids were conducted. The session was completed by stretching cervical muscles, the pectoralis group, and deep neck flexor activation.
The third and final session was conducted on September 2, 2021, with observations of no pain experienced and increased participation in physical activity. Improved posture, scapula positioning, and rhomboid strength were noted, with a functional range of motion in the left shoulder. Finally, exercises were reviewed and progressed to scapula stability with upper extremity function and resistance of 1 kg added.
2.4.2 Biokinetics
Due to the treatment provided by the physiotherapist at that stage of treatment, the biokineticist only focused on rehabilitation through exercise for pain management, improving lower limb joint stability, and increasing general physical activity and functionality. Evidence-based exercises were provided to aid in pain management for the anterior knee pain, which included a home program around the lower limb and core isometric and isotonic strengthening exercises with appropriate mobility exercises. Additionally, proprioceptive exercises such as balancing and intrinsic foot muscle strengthening were also included. The exercise program can be found in Table 2, giving the exercise name and volume. Using FITT (frequency, intensity, time, and type) principles, exercise was prescribed at a frequency of four times a week, an intensity of VAS no more than 3 of 10, with duration no longer than an hour, and strengthening, muscle control, and mobility as the types of exercise.
| Exercise | Volume |
|---|---|
| Warm-up | |
| Cardiorespiratory across 10 m | 2 sets of brisk walking, then 40% maximum, and lastly 60% maximum |
| Psoas lunge stretch | 1 set of 10 each side |
| Main session | |
| Supine ball squeezes | 2 sets of 10 |
| Supine lumbo-pelvic-hip control | 3 sets of 10 |
| Heel taps | 2 sets of 20 (10 each side) |
| Clam series against the wall | 2 sets of each and 6 per set |
| Sit-to-stand with TheraBand around knees | 2 sets of 10 |
| Terminal knee extension | 3 sets of 12 |
| Heel sliders down wall | 2 sets of 20 (10 on each side) |
| Cool-down | |
| Foot doming variations | 2 sets of 8 |
| Soleus stretch | 2 sets of 8, 10 s each |
| Supine glute stretch | 2 sets of 8 |
| RP exercise prescription | |
| Finger squeezes | Complete as necessary to control symptoms of pain and stiffness |
| Fist flexion, extension, sbduction, and adduction | |
| Hand hook shapes | |
Furthermore, exercises were also prescribed to target pain and stiffness resulting from RP. Hand and finger exercises in Table 2 were prescribed to be done in a lukewarm water basin, only to be done when the patient was symptomatic. The goal of the exercises was to control the pain, stiffness, and mobility of the hands and fingers during Raynaud's flare-up.
2.5 Follow-Up and Outcome
2.5.1 Physiotherapy
The patient requested a session due to a reoccurrence of left shoulder pain on August 31, 2022. However, symptoms were mild and not as severe and limiting as the year prior. A predisposing factor to the reoccurrence of the left shoulder pain related to increased studying time during the June/July examinations and increased environmental stress factors. Objectively, trigger points in the upper trapezius and weak deep neck flexors were noted. Due to this, treatment was initiated with myofascial release and stretching of the upper trapezius. Scapula stability and posture adjustments were revisited and reinforced with Kinesio-taping of the upper trapezius. Home exercises were provided to maintain previously identified musculoskeletal imbalances.
2.5.2 Biokinetics
A three-month follow-up was made with the patient to reassess. The patient reported a high academic load, which caused some stress and impacted their ability to be physically active. Hence, adherence to exercise was not 100% of the prescription but was subjectively estimated by the patient to be around 80%. The patient also reported a positive response to exercise, saying it helped with hand discomfort during that last bit of winter and improved overall body pain. Additionally, the physiotherapy treatment also concluded at the end of October, as the patient reported less tenderness and pain with movements of the shoulder. Symptoms associated with RP were also reported to be less as summertime arrived. The only complaint regarding hand discomfort was the index finger causing pain during excessive writing.
A similar consultation procedure was followed, namely gathering anthropometric data, posture analysis, ROM, MMT, special tests, and functional tests (Table 3). Assessments that previously provided normal results were not conducted again, and an additional test was conducted for functional cardiorespiratory capacity. With regard to anthropometric data, a weight of 56.8 kg and a height of 180.2 cm were measured, giving a BMI of 17.5 kg/m2, indicating an improvement into the 6th percentile for age and sex, hence a healthy weight. Arm span was measured to be the same at 186.8 cm, hence an arm span to height ratio that remained unchanged. Resting BP indicated some white coat syndrome, measured at 140/80 mmHg with a heart rate of 62 bpm.
| Postural analysis with observation and palpation of various bony structures and muscle interties | |
|---|---|
| Anterior view | No tenderness on the right inferior medial patella or Pes anserinas |
| Improved vastus medilais oblique muscle mass bilaterally | |
| Equal shoulder height | |
| Lateral view | No forward shoulder posture bilaterally |
| Posterior view | No rearfoot valgus on the right (medial curve of the Achilles tendon) |
| Normal soleus muscle tonus bilaterally | |
| Improved hamstring tonus on the left compared to the right | |
| Type I and II scapula dyskinesia on the left and type I on the right | |
| Normal levator scapulae tonus bilaterally | |
| No tenderness on palpation across the right rhomboid and middle trapezius | |
| Range of motion and manual muscle testing | ||||
|---|---|---|---|---|
| Test | Joint movement | Left | Right | Comments |
| Range of motion | Hip flexion | 87° | 90° | No pain at end ROM |
| Knee extension | 180° | 180° | No pain at end ROM | |
| Knee flexion | 121° | 112° | ||
| Shoulder abduction | 180° | 180° | Left shoulder ROM improvement, with no experience of pain | |
| Shoulder flexion | 180° | 180° | ||
| Manual muscle testing (Oxford scale) | Hip flexion | 4 | 4 | No pain at end ROM |
| Hip abduction | 4 | 5 | ||
| Knee flexion | 5 | 5 | ||
| Knee extension | 5 | 5 | No pain at end ROM | |
| Shoulder abduction | 4 | 5 | Left capsule and supraspinatus pain at end ROM | |
| Shoulder flexion | 4 | 5 | No pain experienced | |
| Lower and upper extremity special tests | |||
|---|---|---|---|
| Test | Left | Right | Comment |
| Kendal | − | − | No pain on either movement or either side |
| Patella compression | − | − | No apprehension observed from the patient |
| Clarke's sign | − | − | |
| Empty can | + | + | Pain felt on the left at 45° of VAS 3, but no pain on the right |
| Belly press | − | − | No pain with improved strength noted |
| Hornblower's sign | − | − | No pain reported, but less than optimal strength noted |
| 90° External rotation | + | − | Pain experienced at end ROM of VAS 3 |
| Modified pediatric clinical test of sensory interaction in balance | ||
|---|---|---|
| Condition | Stance duration (s) | Degree of sway |
| Stable surface with eyes open | 30 | 0 |
| Stable surface with eyes closed | 30 | 1 |
| Unstable surface with eyes open | 30 | 1 |
| Unstable surface with eyes closed | 30 | 3 |
Functional tests in the follow-up included the mPCTSIB, bridge movement with leg extension, a squat for the lower limb, a wall push-up, and scapular humeral rhythm. The mPCTSIB improved on all fronts. Such improvement indicated better integration between the three balance systems to maintain postural control and balance and improved reliance on the vestibular system. The bridge movement showed significant improvement, with muscle activation felt in the hamstring and improved endurance ability of the muscles, as the legs did not “get shaky,” as described by the patient. Additionally, no hip drop was seen on the right, but a slight hip drop was still present on the left during leg extension with the bridging movement. Such observations agree with the MMT conducted, but an improvement in pelvic stability was seen, nonetheless. The squat showed complete improvement, with no technical issues or pain being displayed or expressed by the patient. Even though pes planus is structurally present, no drop in the medial arch indicates improvement in dynamic arch stability provided by the intrinsic foot muscles.
Shoulder functional tests also indicated improvement with the wall push-up provoking no pain and improved scapular control, as only the left scapula displayed delayed movement but no winging bilaterally. Such results indicate an improved ability of the serratus anterior to engage and provide dynamic stability to the scapulothoracic joint. Similar results were seen with the scapula-humeral rhythm, as the only delayed movement was noted in the left scapula, with the right scapula displaying the correct scapula-humeral rhythm.
3 Discussion
The importance of reporting on this case relates to the intricate presentation of HSD, RP, and musculoskeletal injuries, in conjunction with the multidisciplinary approach to treatment. The multidisciplinary treatment focuses on the adjunct treatment for HSD, RP, and musculoskeletal injuries from a physiotherapist and biokineticist. Additionally, the simultaneous presentation of HSD and RP has never previously been reported.
To implement exercise therapy for HSD, an extensive understanding of the environmental factors is required as related to repetitive microtrauma of a joint due to joint laxity. In particular, children tend to have a higher complaint of musculoskeletal pain, which tends to be idiopathic, chronic, and misaligned with clinical historical evidence [9]. Musculoskeletal pain is regularly accompanied by muscle weakness and impaired joint control mechanisms, resulting in balance impairments and reduced joint position sense (kinesthesia). Poor proprioception leads to changes in joint kinematics and kinetics [10]. Due to the combinative effect of reduced proprioception, kinesthesia, and muscle strength, children with HSD may have poor coordination, suboptimal posture, and gait abnormalities [4].
Research indicates that reduced proprioception in children with HSD increases the risk of injury, especially in the knee [2, 4]. Reduced proprioception may be associated with improper feedback from mechanoreceptors located in ligaments and improper feedback from reflexes such as the muscle spindles and Golgi tendon organ. Due to reduced proprioception, children with HSD also have difficulty with kinesthesia, which may contribute to an increased risk of knee joint injuries. Not only is proprioception impacted, but children with HSD also have reduced muscle mass and strength, possibly associated with an increase in tendon laxity, reducing its ability to transmit the power generated by the muscle. Furthermore, individuals with HSD may also have trochlear dysplasia which contributes to patellofemoral instability, further increasing the risk of injuries such as PFPS [11].
Altered kinematics in the shoulder also increase the risk of a shoulder injury due to altered function in neuromuscular control, reduced dynamic stability from rotator cuffs, and improper scapula coordination [12]. Normally, the scapula rotates upward, tilts posteriorly, and rotates externally to ensure the stability of the humeral head in the glenoid fossa. When such kinematics are altered, it results in scapula dyskinesia. Consequently, there is an increased risk of shoulder impingement for structures under the acromial arch, including the supraspinatus, long-head bicep tendon, and acromial bursa. Moreover, like the knee, proprioception is also poor in the shoulder, impacting kinesthesia and altering shoulder kinetics [13].
Poor proprioception, kinesthesia, joint kinematics, and kinetics increase the risk of joint injury and pain. Children with HSD also have reduced physical activity levels and increased deconditioning and exercise intolerance, all because of fear of provoking pain and inducing injury [2]. All of the above-mentioned factors, poor knee and shoulder stability related to proprioception and muscle strength, as well as reduced physical activity, were presented within this current case. All these factors can appropriately be targeted with exercise therapy related to improving neuromuscular control to improve clinical outcomes of joint pain.
Exercise therapy has also been shown to be adequate for RP. Little research is available regarding exercise and RP alone. Still, RP is a symptom of systemic sclerosis and has abundant research regarding the benefit of exercise for microvascular reactivity. Specifically, combined aerobic and resistance exercises improve overall vascular endothelial function [14]. Furthermore, hand exercises have improved hand function and pain in individuals with systemic sclerosis symptoms of RP [15]. However, research is limited regarding the improvement of hand microvascularity, as it is hypothesized that exercise appropriately benefits large vascular systems but not conduit systems [16].
4 Conclusion
Exercise therapy has been shown to be an appropriate treatment for HSD and was also implemented for RP, regardless of the lack of scientific evidence. The multidisciplinary team also appropriately treated the patient within their scope of practice to successfully reach the clinical outcomes of reduced pain and improved physical activity. The positive response to adjunct therapy within this case creates a foundation for future approaches to treating HSD and associated musculoskeletal injuries, as well as improving pain associated with RP, especially with winter flare-ups. Yet, to appropriately understand the impact of exercise on RP, further research with larger sample sizes are required to determine the strength of the benefit. Finally, the follow-up of the psychological impact exercise had on HSD and RP could have been better and seen as a limitation in the article due to not readministering the PRQL.
Author Contributions
Su-ané Zwiegelaar: conceptualization, data curation, formal analysis, investigation, writing – original draft, writing – review and editing. Deepthi R. Abraham: conceptualization, supervision, writing – review and editing. Olivia Roman: data curation. Karen E. Welman: resources, supervision, writing – review and editing.
Consent
Written consent and assent were obtained for the use of data upon the first consultation. Furthermore, written consent was retaken to ensure the inclusion of the data collected by the physiotherapist in her separate consultation. The article was submitted with its consent and assent. To the Health Research Committee of Stellenbosch University to ensure all ethical guidelines were met and maintained throughout the process.
Open Research
Data Availability Statement
The data supporting this study's findings are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.