Cutaneous perianal herpes simplex virus infection mimicking condylomata acuminata in a renal transplant recipient: A case report and literature review
Abstract
Key Clinical Message
Herpes simplex virus (HSV) infection can present atypically in immunosuppressed patients, such as renal transplant recipients, often mimicking conditions like condyloma acuminata. This case report of a 39-year-old male renal transplant recipient underscores the importance of maintaining a high level of clinical suspicion and employing thorough diagnostic techniques, including skin biopsy and polymerase chain reaction, to accurately diagnose chronic lesions and those not responding to initial therapies in these patients. Timely initiation of antiviral therapy, such as intravenous acyclovir, is crucial for improving patient outcomes. Clinicians should be aware of the diverse presentations of HSV in immunocompromised individuals to ensure prompt and effective treatment.
Herpes simplex virus (HSV) has a worldwide distribution and a wide range of clinical presentations. In immunosuppressed patients, the infection can have atypical presentations. We report a 39-year-old renal transplant recipient male with a cutaneous HSV infection mimicking condyloma acuminata. The diagnosis was confirmed by skin biopsy and polymerase chain reaction. The patient was treated with intravenous acyclovir. This case illustrates the significant clinical challenges in establishing a correct diagnosis of this common infection in these patients. A high level of clinical suspicion will result in a prompt diagnosis and timely initiation of antiviral therapy, which is crucial to better patient outcomes.
1 INTRODUCTION
Herpes simplex virus (HSV), is a member of an enveloped, double-stranded DNA virus family named Herpesviridae, this virus causes latent infection of neural ganglia.1 It has a worldwide distribution and a wide range of clinical presentations depending on the host's immune status and the infection site. In immunocompetent individuals, the most common presentation includes painful vesicles and erosions on an erythematous base, which can evolve into pustules and/or ulcerations.2, 3 In immunocompromised individuals such as solid organ or bone marrow transplant recipients, patients with hematologic malignancies, and human immunodeficiency virus (HIV) infection, HSV infection can have atypical manifestations, including chronic non-healing ulcers, verrucous plaques, and large protruding tumors. In the case of immunosuppressed patients, the lesions may disseminate and occur at multiple sites, including atypical locations such as the buttocks, abdomen, and lower back. Depending on the level of immunosuppression, HSV infection can have a variable duration, severity, and outcome. It can affect multiple or atypical sites, such as the abdominal, and thoracic regions, or even become disseminated.4, 5 In this article, we report a case of cutaneous perianal infection that presented as warty skin-colored papules and plaques underline the challenges in the morphologic and clinical diagnosis of this entity, and review the literature on verrucous HSV lesions in non-HIV patients.
2 CASE PRESENTATION
A 39-year-old male with a past medical history of renal transplantation 5 years ago due to uncontrolled hypertension, presented to our outpatient clinic with a two-month history of asymptomatic perianal lesions. Physical examination revealed perianal verrucous skin-colored papules and plaques (Figure 1). There were no other genital lesions, and the physical examination of other cutaneous areas was unremarkable. The patient did not report any previous occurrence of similar lesions. He has been receiving prednisolone 5 mg daily, azathioprine 50 mg two times a day (BID), and mycophenolate mofetil 1000 mg BID for his renal transplant since 5 years ago.

3 METHOD
The patient was initially diagnosed with condyloma acuminata in another clinic and was scheduled for cryotherapy. However, because of his immunosuppression to rule out other clinical differential diagnoses including squamous cell carcinoma (SCC), Cytomegalovirus (CMV) infection, and HSV infection, we performed a punch biopsy.
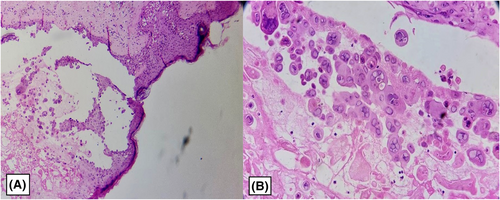
The histologic examination revealed separated and occasionally multinucleated keratinocytes, acanthosis, and spongiosis with nuclear inclusion in the epidermis. In the dermis, there was severe mixed inflammation in superficial, and mild perivascular and peri adnexal infiltration with extensive RBC extravasation in the deep dermis consistent with HSV infection (Figure 2). The polymerase chain reaction (PCR) assay, yielded a positive result for HSV-2.
The laboratory tests were evaluated before starting the treatment and were as follows; fasting blood sugar (FBS) = 94 mg/dL, Urea = 56 mg/dL, serum creatinine (SCr) = 2.15 mg/dL, Serum Glutamic-Oxaloacetic Transaminase (SGOT) = 23 IU/dL, Serum Glutamic Pyruvic Transaminase (SGPT) = 19 IU/dL, alkaline phosphatase (ALP) = 121 U/dL, erythrocyte sedimentation rate (ESR) = 37 mm/h and C-reactive protein (CRP) = 0.6 mg/dL. The complete blood count (CBC) and the serum electrolyte tests were normal. The patient's HSV-2 IgM level was measured at 0.5 Index Value (IV), which was categorized as negative (negative <0.9 IV). The HSV-2 IgG level was found to be 2.1 IV, falling into the positive range (positive >1.10 IV). These findings indicated a chronic herpes infection. The patient was promptly admitted for further management, during his admission he received intravenous Acyclovir 10 mg/kg every 12 h for 10 days, and after the restoration of his renal function to baseline levels, he was transitioned to oral valacyclovir 1 g BID for 2 weeks until all lesions resolved. As the patient was in good general health and non-septic, with a lowest Estimated Glomerular Filtration Rate (eGFR) of 55, none of his medications required discontinuation or adjustment during this period.
4 DISCUSSION
In immunocompromised patients, such as HIV-positive individuals, those undergoing immunosuppressive or chemotherapy, and organ transplant recipients, primary and secondary HSV types 1 and 2 infections tend to be more aggressive and persistent.6 They can also have atypical presentations like necrotic painful ulcers, chronic large ulcers, or verrucous plaques, with a predilection for atypical sites.7, 8 These individuals are also predisposed to severe complications of HSV infection such as dissemination and vital organ involvement including corneal and retinal infections, hepatitis, pneumonitis, and encephalitis resulting in increased mortality.9, 10
Diagnosing HSV infection is mainly achieved by viral cultures from mucosal surfaces or vesicles, a Tzanck smear, Molecular-based techniques such as PCR, and histological examination.3, 9 In regards to sampling mucocutaneous lesions, the timing is important; samples of genital lesions >5 days old yielded less than 35%. Direct Fluorescent Antibody (DFA) testing of mucocutaneous lesions, bronchoalveolar lavage (BAL), and other clinical samples can provide rapid results. Compared with tissue culture, the sensitivity is between 60% and 75% and specificity is 85%–99%. PCR for HSV DNA is 4-fold more sensitive than tissue culture for diagnosing mucocutaneous HSV and has largely replaced culture and DFA for HSV diagnosis in most body sites. Nevertheless, when drug-resistant HSV disease is suspected culture should be done. Serologic testing is infrequently useful for diagnosing acute infection as most patients will be HSV seropositive, and increased IgM levels in HSV may occur with reactivation and not a new acquisition.11 Our patient had undergone renal transplantation and was on immunosuppressive therapy for 5 years. He presented with perianal verrucous skin-colored papules and plaques and the diagnosis was confirmed by skin biopsy and histological examination. Because HSV infections cause significant morbidity in immunocompromised patients, early diagnosis and treatment are necessary. Significant developments have occurred in the availability of antiviral agents over the past two decades. In immunocompromised patients, limited mucocutaneous disease can be treated with nucleoside analogs; oral acyclovir, valacyclovir, or famciclovir. On the other hand, cases with disseminated or extensive disease, and visceral or central nervous system (CNS) involvement can be treated with intravenous acyclovir. Therapy should be continued until complete healing of the lesions and for a minimum of 5–7 days.11 In the case of severe immunosuppression, many authors recommend treatment with intravenous acyclovir, yet acyclovir-resistant HSV is a growing challenge in the management of immunosuppressed patients and Foscarnet is the sole FDA-approved antiviral medication in these cases.12 Our patient was treated with intravenous Acyclovir 10 mg/kg every 12 h for 10 days and then valacyclovir 1 g BID for 2 weeks, until all lesions resolved.
Quesada et al. conducted a comprehensive literature review in 2014 focusing on verrucous HSV lesions. The main emphasis of the Quesada et al review, and most of the antecedent literature, is on patients with HIV, higher inclination for high-risk sexual activities as well and increased viral shedding in acquired immunodeficiency syndrome (AIDS) patients make HSV infection more common and therefore easier to suspect in these patients.13 Organ transplant recipients and other forms of immunosuppression can also have severe and atypical presentations of HSV infection, requiring different treatment strategies, such as adjusting immunosuppression, monitoring drug interactions, and preventing drug resistance.14 Notably, our review provides valuable insights into verrucous HSV presentations in non-HIV patients, broadening the understanding of this condition beyond its association with HIV/AIDS.
We reviewed the literature from 2014 to 2023 and included cases in non-HIV patients. To be included in this review, articles had to be available in the English language and only patients without HIV/AIDS comorbidity were included. The terms “verrucous HSV” and “Herpes Vegetans” were used in our search (Table 1). We reviewed eight articles and found nine cases of HSV infection with atypical presentations, most of the patients were immunocompromised because of immunosuppressive therapy, primary immunodeficiency, or leukemia. Lesion sites varied from anogenital and perioral to unconventional locations such as the shoulder.
| Authors | No. | Age | Sex | Localization | Pathology | Other medical conditions | Rx |
|---|---|---|---|---|---|---|---|
| Al-Zubaidi et al. (2023) | 1 | 39 | M | Perianal | Acanthosis, spongiosis keratinocytes, with viral nuclear inclusions, severe mixed inflammation in the superficial dermis, mild perivascular and peri adnexal infiltration with extensive RBC extravasation into the deep dermis | Renal transplantation | Acyclovir 10 mg/kg BID for 10 days, and then oral valacyclovir 1 g BID for 2 weeks |
| Ho, et al.15 | 2 | 65 | M | Right posterior shoulder | Epithelial hyperplasia, ulceration, eosinophilic intranuclear inclusions, focal multinucleated keratinocytes. Immunoperoxidase staining positive for both HSV-1 and HSV-2 | T2DM, CKD, Metastatic RCC, Medication-induced pneumonitis | IV acyclovir 10 mg/kg then oral valaciclovir 1 g TDS |
| Guimarães, et al.16 | 3 | 74 | M | Right zygomatic region | N/A | T2DM, obesity, coronavirus disease-19 pneumonia | Oral acyclovir 400 mg thrice daily for 10 days |
| Parsons, et al.17 | 4 | 18 | F | Perioral region, nose, right cheek | Spongiosis, mixed granulomatous dermal infiltration with fat necrosis | Common variable immunodeficiency | IV foscarnet, oral valaciclovir |
| Koushk-Jalali, et al.18 | 5 | 45 | F | Left labial angle | Cornified squamous epithelium with eosinophilic intranuclear inclusion bodies surrounded by a dense inflammatory infiltrate. IHC staining positive for HSV. | Primary myelofibrosis | Oral acyclovir 500 mg TDS for 3 weeks, topical fusidic acid cream |
| Boix-Vilanova, et al.19 | 6 | 40 | F | Vulva | N/A | SLE, renal transplantation | Valaciclovir 500 mg BID |
| Kaufman and Sivendran20 | 7 | 75 | F | Perianal region | N/A | CLL | IV acyclovir 5 mg/kg TDS for 7 days then oral acyclovir |
| Owen, et al.21 | 8 | 55 | M | Penoscrotal |
Center: Accumulation of acute and chronic inflammatory cells (with a preponderance of plasma cells), pseudoepitheliomatous hyperplasia. Periphery: Multinucleated giant cells with intranuclear eosinophilic inclusions, nuclear molding, and chromatin margination |
Unknown | Refused follow-up |
| Shim, et al.22 | 9 | 70 | M | Glans penis | Surface ulceration, dense chronic dermal inflammatory infiltrate (mainly plasma cells, fewer lymphocytes) | CLL | Initially acyclovir and ciprofloxacin then, upon relapse, famciclovir followed by long-term prophylactic famciclovir |
| 10 | 76 | M | Buttock | N/A | CLL | Oral acyclovir 400 mg five times daily for 2 weeks |
- Abbreviations: BID, twice a day; CKD, chronic kidney disease; CLL, chronic lymphocytic leukemia; F, female; HSV, Herpes Simplex Virus; IHC, immunohistochemistry; IV, intravenous; M, male; RCC, renal cell carcinoma; SLE, systemic lupus erythematosus; T2DM, type 2 diabetes mellitus; and TDS, three times a day.
The age distribution ranged from 18 to 76 years, with a mean age of 53.7 years. The gender distribution shows a slight male predominance (6 out of 10 males). The lesion had various localization and the anogenital lesion was the most reported site (6 out 10), followed by the perioral and facial region (3 out of 9), in one patient the lesion was on the shoulder, and one patient was on the buttock. Some patients had more than one lesion site, such as patient 4 who had perioral, nose, and right cheek lesions.
The most common histopathological features are epithelial hyperplasia, ulceration, eosinophilic intranuclear inclusions, and focal multinucleated keratinocytes.
The most common first-line treatment option was oral acyclovir 400 mg three times a day (TDS) up to five times a day. In more severe cases Intravenous Acyclovir 5 mg/kg to 10 mg/kg TDS was initiated.
Depending on the severity and therapeutic response the treatment duration ranged from 10 days to 3 weeks.
In general, the treatment outcome was favorable, with most cases showing complete or partial resolution of the lesions after antiviral therapy.
5 CONCLUSION
This case report and review of the literature underscores the formidable clinical challenges in accurately diagnosing cutaneous HSV infections, in immunosuppressed individuals. The atypical presentation mimicking condyloma acuminata in this renal transplant recipient patient highlights the need for a high suspicion rate and thorough diagnostic evaluation for rapid diagnosis and initiation of antiviral therapy, to reduce and prevent complications and achieve favorable patient outcomes. This narrative emphasizes the intricate interplay between immunosuppression and HSV infections, emphasizing the imperative for vigilant clinical management.
AUTHOR CONTRIBUTIONS
Nabaa Al-Zubaidi: Writing – original draft. Mohsin Al-Zubaidi: Writing – original draft. Nasim Gholizadeh: Investigation; writing – review and editing. Shirin Zaresharifi: Investigation; resources; writing – review and editing.
ACKNOWLEDGMENTS
The authors have nothing to report.
FUNDING INFORMATION
No funding was received for this study.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflicts of interest.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data are available from the corresponding author upon reasonable request.




