Spinal gout recovery with urate-lowering therapy: A case report
Kunfang Huo and Jialin Zhang contributed equally to this work.
Key Clinical Message
The occurrence of spinal gout resulting in erosion of the superior articular process in patients with low back pain is uncommon, potentially leading to misdiagnosis and inappropriate treatment. Urate-lowering therapy may be beneficial in improving joint destruction and bone erosion, as evidenced by our case.
1 INTRODUCTION
The prevalence of gout ranges from less than 1% to 6.8%, with an incidence of 0.58–2.89 per 1000 person-years.1 The most severe consequence of gout is the complete destruction of the joint. Currently, preventing joint damage is the primary focus of gout treatment. Advanced imaging techniques have increasingly allowed for the better detection of joint damage and tophi.2 There is growing evidence indicating a strong relationship between joint damage and the presence of tophi at affected sites.3 Urate-lowering therapy (ULT) is now essential in the long-term management of gout and may be good for the absorption of tophaceous gout. However, some studies have shown that ULT did not significantly change joint erosion.4 Interestingly, in our case, the joint damage to the superior articular process showed recovery with ULT after 18 months.
2 CASE HISTORY
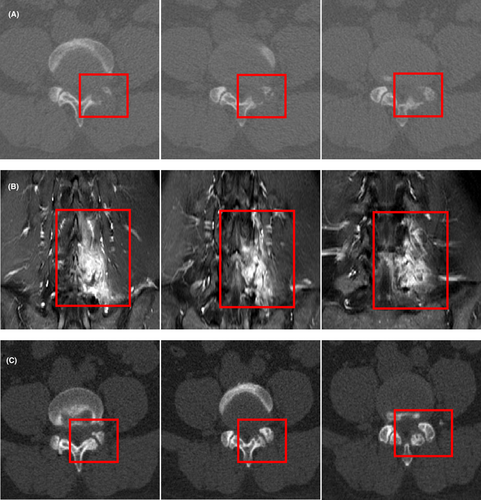
A 36-year-old man was admitted to the spinal surgery department of the hospital due to chronic low back pain lasting 3 months, characterized by prolonged pain while walking that was relieved with rest. He had not experienced any joint pain. The physical examination clearly showed no tophi. A computed tomography (CT) scan revealed bone destruction in the left inferior articular process of L4 and the superior articular process of L5 (Figure 1A, red box). Contrast-enhanced magnetic resonance imaging (MRI) of the lumbar spine showed bone destruction with surrounding soft tissue swelling (Figure 1B, red box), indicating local inflammation. There was no relevant family history, and none of his family members exhibited gout.
3 METHODS (DIFFERENTIAL DIAGNOSIS)
A biopsy performed by a spinal surgeon revealed pathological findings suggestive of tophus (Figure 2A, black arrows) and giant cell reaction (Figure 2A, yellow arrows). The patient's plasma uric acid level was significantly elevated at 601 μmol/L (10.1 mg/dL), leading to a suspicion of spinal gout. He was subsequently admitted to the rheumatology and immunology department for further diagnosis. Given the low prevalence of spinal gout, additional tests were conducted to exclude other causes of lumbar erosion, such as spondyloarthropathy and spinal tuberculosis.
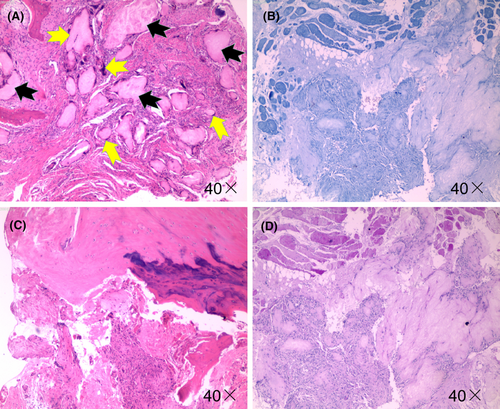
Human leukocyte antigen B27 was negative, and there were no other positive results to support a diagnosis of SpA. However, TB infection was confirmed with positive results from both the tuberculin test (PPD test) (2+) and interferon-γ release assays. To identify the presence of tuberculosis or other diseases contributing to bone erosion, additional tests were conducted on the punctured tissue, including acid-fast, periodic acid–Schiff, and periodic acid-silver methenamine staining (Figure 2B–D). All staining results were negative.
4 OUTCOME AND FOLLOW-UP
Consequently, it was concluded that the patient's lower back pain resulted from spinal gout at L4–L5 despite a latent tuberculosis infection, tumor, and spondyloarthropathy. The patient was treated consistently with urate-lowering therapy by febuxostat (40 mg given orally every day). However, after given uric acid-lowering treatment with febuxostat, the patient suffered from pain in the left knee, with obvious skin redness and swelling of left knee, increased local temperature, and limited left knee movement. We considered the acute attack of gouty arthritis, and we performed dual energy CT scan of the left knee and confirmed our diagnosis. The blood uric acid was maintained at about 360 μmol/L. A follow-up CT scan of the lumbar region, conducted 18 months after the ULT treatment, revealed that the joint damage in the superior articular process had recovered (Figure 1C, red box).
5 DISCUSSION
Low back pain in young adults could be a common symptom of many diseases, such as spondyloarthropathy, tuberculosis infection, neoplasm metastasis, lumbar muscle strain, and prolapse of the lumbar intervertebral disk. It is crucial to pay close attention to bone or joint damage, as it can have undesirable consequences. Therefore, a biopsy may sometimes be necessary. In our case, the young man had latent TB infection (LTBI), which could lead to misdiagnosis and inappropriate treatment, such as ankylosing spondylitis.5
Approximately a quarter of the global population is infected with tuberculosis,6 with the majority having latent TB infection (LTBI). LTBI is characterized by the body's sustained immune response to tuberculosis antigens without any clinical signs of active TB.7 Both the tuberculin skin test and interferon-gamma release assays can yield positive results for LTBI, leading to potential misdiagnoses as other diseases or conditions linked to tuberculosis infection. First-line anti-tuberculosis medications often cause side effects and organ damage. Therefore, diagnosing TB infection in patients without symptoms (such as fever, night sweats, or weight loss) requires careful consideration. Accurate diagnosis should rely on acid-fast staining, pathological examination, or PCR testing of tissues and body fluids. In our case, despite using CT and MRI, the surgeons could not definitively diagnose the patient. Consequently, a biopsy and pathological examination were performed. Without these pathological tests, the patient might have been misdiagnosed with spinal tuberculosis. Additionally, some anti-tuberculosis drugs can increase blood uric acid levels, potentially worsening bone erosion after treatment.
Research on the surgical treatment of gout indicates that urate can redeposit post-surgery without ULT,8 leading to bone and joint damage. ULT means that the target serum uric acid level is determined based on the patient's condition and comorbidities, but not higher than 360 μmol/L. The pathogenesis of bone erosion has revealed infiltration by various immune cells, including macrophages and lymphocytes. Monosodium urate crystals, which are composed of tophi, can stimulate immune cells to produce numerous proinflammatory cytokines, such as interleukin 1 and tumor necrosis factor, activating the RANK–RANKL pathway, which is crucial for bone remodeling.9-11 Therefore, ULT is the most essential treatment for gout. However, more evidence is required to determine whether ULT effectively improves joint destruction and bone erosion. A randomized study showed that treatment with febuxostat did not significantly restore joint erosion over a 2-year period.4 In the clinical trial, there were no improvement in bone erosion scores, and we considered several potential reasons for this outcome. Some clinical trials on urate-lowering therapy have not established differential treatment targets based on the presence of comorbidities in study participants. According to the most clinical guidelines for gout, the target of blood uric acid concentration of patients with diseases such as hypertension and diabetes should be lower (<5 mg/dL). In addition, the patient included in the study had low baseline bone erosion scores and very small radiographic damage, so the changes may not be obvious. However, the study showed that the ULT can significantly improve joint synovitis in patients with gout, which suggests that standardized ULT still may be beneficial to the recovery of gouty arthritis, which needs more clinical studies to confirm. And this case report demonstrated that low back pain and spinal bone erosion can be caused by gout and that bone destruction can be recovered with ULT. This case has also significantly increased our confidence in treating urate-induced spinal joint destruction.
AUTHOR CONTRIBUTIONS
Kunfang Huo: Data curation; formal analysis; investigation; writing – original draft; writing – review and editing. Jialin Zhang: Data curation; formal analysis; investigation; writing – original draft; writing – review and editing. Yanhua Lin: Data curation; formal analysis; investigation. Qianyun Chen: Data curation; formal analysis; investigation. Han Zhong: Data curation; formal analysis; investigation. Bin Yang: Conceptualization; data curation; formal analysis; investigation; writing – original draft; writing – review and editing.
FUNDING INFORMATION
Supported by the Medical Science and Technology Research Project of Foshan City.
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interest to declare.
ETHICAL APPROVAL
This study received ethical clearance from the Ethical Committee of Shunde Hospital, Southern Medical University (The First People's Hospital of Shunde).
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data may become available upon reasonable requests to the corresponding author.