Refractory CRPS pain treated with psilocybin: A case report
Key Clinical Message
Psilocybin shows promise as a treatment for CRPS, offering significant pain relief and functional improvement in a patient with refractory symptoms. This case highlights the need for further research into psilocybin's efficacy and optimal dosing for chronic pain management.
1 INTRODUCTION
Complex regional pain syndrome (CRPS) is a debilitating neuropathic disorder marked by persistent pain disproportionate to inciting injury.1, 2 Though CRPS is often seen in the setting of a traumatic event but may also occur spontaneously.3, 4 The pathophysiology of CRPS is likely multifactorial, with many proposed mechanisms present in the literature involving dysregulation in both the sympathetic and central nervous systems, as well as contributions from genetic, inflammatory, and psychological factors.2
CRPS pain is often accompanied by various other sensory, vasomotor, sudomotor, motor, or trophic symptoms.3 These symptoms significantly impact their quality of life and daily functioning.5 While reports of CRPS' incidence range from 0.82 to 5.46 per 100,000 person-years,6, 7 the severe nature of CRPS underscores the need for effective treatment options.
Treatment for CRPS is often challenging, with many cases proving refractory to standard therapies.8 Conservative treatments typically include physical therapy, occupational therapy, or psychotherapy, along with medications such as NSAIDs, antiepileptic drugs (AEDs), antidepressants, and opioids.8 However, these medications often carry significant side effects and may not provide adequate relief for all patients. Invasive options, such as sympathetic blocks and spinal cord or dorsal root ganglion (DRG) stimulation,8 are available but bear risks associated with interventional procedures. As a result, there is a growing need for alternative approaches, particularly for patients who wish to avoid or have not benefited from conventional medications or interventional procedures.
Recent interest in the role of psychedelics in pain management has prompted exploration into their potential use for CRPS.9 This case report describes the experience of a 54-year-old female with CRPS and her use of psilocybin as a treatment. To our knowledge, this is the second case suggesting the potential efficacy of psilocybin for managing CRPS symptoms, underscoring the importance of exploring novel therapeutic avenues in chronic pain management. This study contributes to the emerging literature on innovative treatments for CRPS, offering alternative options beyond conventional therapy.
2 CASE HISTORY
A 54-year-old female (BMI 24.0) with a history of migraines and depression presented with 4 months of burning pain and numbness in her right lateral thigh. She described how her 9 out of 10 pain began immediately following right subacromial decompression in 2003. Nerve conduction studies revealed absent sensory nerve action potential (SNAP) in the right lateral femoral cutaneous nerve compared to the left. Her surgeon attributed the lateral femoral cutaneous nerve mononeuropathy secondary to intraoperative seat belt tightness. She was initially diagnosed with meralgia paresthetica and treated with gabapentin. Despite treatment, her symptoms persisted and were accompanied by allodynia, temperature fluctuations, skin discoloration, asymmetrical sweating, weakness, and trophic changes. This constellation of symptoms ultimately led to a diagnosis of CRPS in 2010.
Of note, the patient began experiencing glossodynia in 2009, with attacks occurring about four times per week and lasting from 2 h to 3 days. The pain was rated at 8 to 10 out of 10 and was not responsive to medical management.
3 METHODS
Complete blood count, basic metabolic panel, coagulation values, and inflammatory biomarkers were within normal limits during this period (Appendix S1). She began to fall 4–8 times per month as her symptoms progressed. Combinations of antidepressants, antiepileptics, muscle relaxants, opioids, and topical ketamine failed to provide adequate relief. She continued to take Oxcarbazepine which reduced the pain to 4 out of 10 but was discontinued in 2013 due to significant hyponatremia, after which symptoms re-flared.
The patient underwent a spinal cord stimulator (SCS) trial in 2015 with leads at bilateral T7 and T8 levels which brought pain level to 0 to 1 out of 10. Revision was required due to lead migration, but it was ultimately removed in 2018, prompting a return to 9 out of 10 pain.
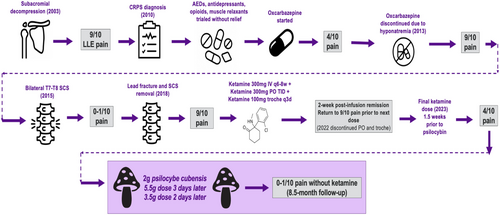
In 2016, the patient was prescribed ketamine, 300 mg of which was administered intravenously every 6–8 weeks and titrated up to 1200 mg, resulting in 2 weeks of transient postinfusion remission. Her pain would return to a baseline of 9 out of 10 before the next dose. In addition, she took 300 mg capsules three times daily and 100 mg troches every 3 days during that time. The oral ketamine and ketamine troche were discontinued in 2022. Given the past success of psychedelic treatments, she decided to try guided sessions of psilocybin cubensis dried mushrooms in a rural indoor setting with one-on-one emotional support from a certified psilocybin facilitator. A visual representation of the case timeline can be found in Figure 1.
4 RESULTS
In 2023, one and a half weeks after her final dose of intravenous ketamine 1200 mg, her pain remained 4 out of 10. The patient consumed 2 g, 5.5 g, and then 3.5 g of Psilocybe cubensis mushrooms. The second dose was 3 days after the first, and the third was 2 days later. Alongside dosing sessions, the patient partook in adjunctive neuromechanics, neurovisual modulation, and tactile reprocessing programming. Leading up to the psilocybin dosing, she had tried these adjunctive techniques alone without concurrent psilocybin use, but did not achieve significant relief.
At 1-month follow-up, the pain decreased to 0 to 1 out of 10 as recorded by the Brief Pain Inventory (BPI). She also endorsed a decrease in mood symptoms at follow-up, supported by Montgomery-Asberg Depression Rating Scale (MADRS), Hamilton Depression Rating Scale (HAM-D), and Clinician-Administered PTSD Scale (CAPS) scores, as reflected in Table 1.
| Initial | One-month follow-up | Nine-month follow-up | |
|---|---|---|---|
| BPI (pain now) | 4 | 0–1 | 0–1 |
| MADRS | 41 | 0 | |
| HAM-D | 22 | 2 | |
| CAPS | 54 | 3 |
Her CRPS pain remained at 0 to 1 out of 10 without ketamine for 9 months. The frequency of her falls decreased by 75%, with only two falls in the 9-month period since starting psilocybin, a significant improvement from before. Additionally, the frequency, intensity, and duration of glossodynia attacks have reduced by 75% each. She reports that the attack intensity no longer rises above 2 out of 10. No long-term adverse events after psilocybin were noted.
5 DISCUSSION
CRPS is notoriously challenging to manage, with a substantial need for alternative long-term management strategies, particularly for cases unresponsive to conservative management. It is estimated that 10%–20% of patients with CRPS, specifically those with pain confined to the distal extremities, can have pain refractory to both spinal cord stimulation (SCS) and conservative management.10 The urgency for new treatments is underscored by the limitations of existing therapies.
A recent case series from 2023 reported one successful instance of CRPS treated with psilocybin, where a patient with 5 years of CRPS pain, averaging a baseline pain score of 5 out of 10, experienced significant relief using 500 mg microdoses of psilocybin-containing mushrooms daily for 7–10 days, followed by a rest period of 2–3 days to avoid gastrointestinal side effects and rebound pain or withdrawal.11 Each dose provided approximately 80% pain relief for 3–4 h, which gradually returned to baseline over 12 h. This regimen yielded sustained pain relief, which was maintained at the 1-year follow-up, emphasizing the potential role of psilocybin in CRPS management. Notably, no other reports in the literature were identified.
The present case reinforces the need to better understand psilocybin's role in managing CRPS. The mechanisms by which psychedelics could improve CRPS symptoms are not fully understood. Psilocybin's serotonergic effects, particularly through cortical serotonin 2a receptor (5-HT2A) agonism, are believed to contribute to its anti-nociceptive properties.9 Central sensitization in CRPS may drive neuroplastic cortical changes that disrupt sensory processing,12 which psilocybin may help to modulate centrally. This proposed mechanism is distinct from other novel CRPS treatments currently under investigation, such as ketamine, which is thought to reverse long-term potentiation through NMDA antagonism.13 However, more research is needed to elucidate these mechanisms and determine the most effective dosing strategies.
In comparing dosing regimens, the patient in the previously published Lyes et al.11 case utilized microdoses, while the current case involved full doses spanning 2 g–5.5 g. The decision between microdosing and taking full doses should consider the balance between transient side effects and the frequency of administration. Lyes et al.11 reported that the patient initially consumed 2 g of dried psilocybin mushrooms, resulting in 18 h of pain remission but also significant psychotropic, audiovisual, and cognitive changes. This experience prompted the patient to switch to a microdosing regimen that eliminated psychotropic effects but provided only 80% pain relief.
Microdosing may minimize side effects but may require more frequent dosing, while full doses could potentially offer longer-lasting relief with less frequent administration but may cause more pronounced side effects. As research on psilocybin for CRPS expands, special attention should be given to creating population-specific dosing guidelines. Interestingly, many of the higher-quality studies on psilocybin utilize a dose of 0.14 mg/kg.14, 15 However, it is important to consider that these studies focus on headache and migraine populations, not CRPS.
Psilocybin is not FDA-approved and is classified as a Schedule I drug under the Controlled Substances Act, indicating their lack of acceptance for medical use and high abuse potentials.16 Nonetheless, the FDA and several local and state governments are moving toward allowing the use of psilocybin under controlled conditions. This regulatory landscape underscores the importance of continued research into the safety and efficacy of psilocybin for medical purposes. Recent evidence increasingly supports the use of psychedelics including psilocybin for the treatment of chronic pain syndromes.9, 17 As research in this field continues to expand, there is a need for more robust studies with larger sample sizes and protocols designed to reduce bias.
Adjunctive therapies are crucial in managing CRPS, especially since patients often exhibit decreased tactile-spatial processing.18 Functional restoration training activates presensorimotor cortices, progresses to gentle active movements, and culminates in weight-bearing activities.8 Gradual desensitization to sensory stimuli is linked to increased function.19 In this case, neuromechanical techniques, neurovisual modulation, and tactile reprocessing were used alongside psilocybin treatment. These therapies target different aspects of CRPS's complex pathophysiology and are included in the CRPS Treatment Guidelines. This is the third known case demonstrating the synergistic effects of psilocybin and adjunctive therapies in treating various chronic pain conditions.11, 20 More research is warranted to explore the effect of psilocybin with and without adjunctive reprocessing therapies.
Despite the promising outcomes observed in this case, several limitations must be acknowledged. The generalizability of the findings is limited due to the case report's single-patient nature. Additionally, the lack of blinding and randomization introduces bias and poses a challenge to establishing causality and determining the full extent of psilocybin's therapeutic potential for CRPS. Large-scale studies with proper blinding, randomization, and control groups are needed to provide a balanced perspective on psilocybin's effects on CRPS.
6 CONCLUSION
This case report highlights the potential of psilocybin as a treatment for CRPS. The promising results observed in this case and the 2023 case series suggest that psilocybin could represent a valuable addition to the existing treatment options for CRPS, particularly for patients who have not responded to conventional therapies. Further research is essential to comprehensively assess its efficacy, safety, and mechanisms of action. Future studies should prioritize the investigation of optimal dosing strategies, long-term effects, and its potential application in other chronic pain conditions. As the regulatory landscape evolves, conducting well-designed clinical trials will be critical to fully understand psilocybin's therapeutic potential for CRPS and other chronic pain conditions.
AUTHOR CONTRIBUTIONS
David S. Jevotovsky: Writing – original draft; writing – review and editing. Harman Chopra: Writing – review and editing. Court Wing: Conceptualization; project administration. Carlton J. Spotswood: Data curation; investigation. Joel Castellanos: Supervision; writing – review and editing.
FUNDING INFORMATION
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST STATEMENT
The author declares no conflicts of interest.
ETHICS STATEMENT
Given psilocybin's Schedule I status, it is important to note that the patient sought psilocybin treatment independently, without a physician's recommendation. She engaged with a psilocybin facilitator who educated on best practices for harm reduction during the 8 weeks leading up to dosing. The facilitator monitored for adverse events during and after dosing, which were absent. The authors were informed of the patient's case and now present the data.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




