Chronic painful swelling in the popliteal fossa—A diagnostic challenge
Key Clinical Message
The differential diagnoses of popliteal ganglion cysts include Baker's cysts, popliteal artery aneurysms, popliteal tendinitis, popliteal lymphadenopathy, lipomas, and synovial sarcoma.
1 INTRODUCTION
Different types of cystic masses can occur in the popliteal fossa, including meniscal cysts, synovial cysts, and ganglion cysts. Ganglion cysts are benign masses resulting from collagenous degeneration, causing swelling and pain with restricted knee movement. Diagnosis involves ultrasound and MRI, and surgical removal is often required to prevent recurrence.
2 CASE HISTORY
A 49-year-old male patient, with no significant medical history, presented with a progressively painful swelling in the left popliteal fossa over the past 18 months. The patient did not experience fever or deterioration in general health. Physical examination revealed a dry, cold, and non-swollen left knee with preserved mobility. However, there was moderate limitation in flexion due to posterior pain at the end of the range of motion.
3 METHODS
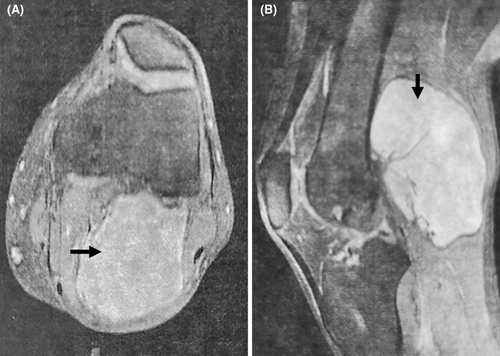
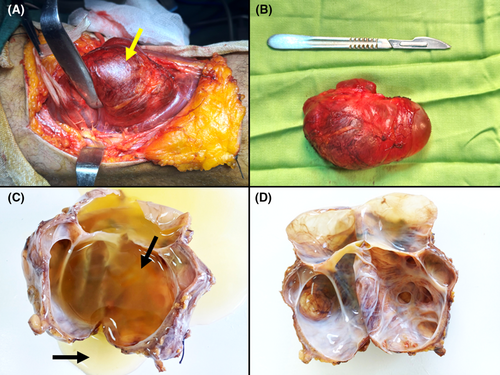
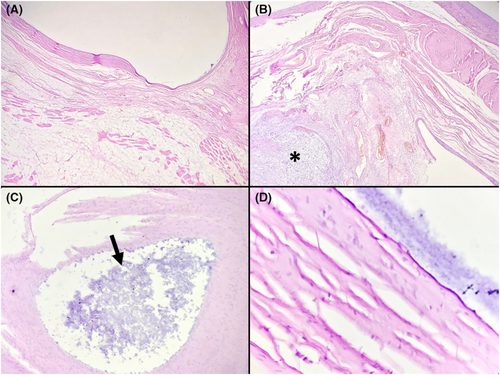
Laboratory tests yielded normal results without any indications of an inflammatory response. MRI of the left knee revealed a multilocular cystic formation with a thin wall, measuring 100 × 72 × 60 mm, containing liquid content (Figure 1). The cyst was found to communicate with the knee joint through a small opening. No joint effusion was observed. The patient underwent surgery in the prone position with a tourniquet, utilizing Trickey's posterior approach. Dissection of the popliteal neurovascular bundle was performed, followed by a complete resection of the well-defined cyst (Figure 2). The cyst was primarily located adjacent to the lateral femoral condyle and laterally relative to the tibial insertion of the posterior cruciate ligament. It was closely adherent to the posterior joint capsule without communication, infiltration, or displacement of the surrounding neurovascular and musculoaponeurotic structures. Vascular supply to the cyst was provided by collateral branches of the popliteal artery and vein. The excised cyst, weighing 160 g and measuring 10 × 7 × 3 cm, exhibited a multilocular configuration and contained a viscous gelatinous fluid (Figure 2). Histological examination confirmed the absence of an epithelial lining in the cyst wall, which predominantly consisted of dense fibrous stroma (Figure 3). The cyst lumen showed the presence of myxoid material (Figure 3). The diagnosis was therefore a popliteal ganglion cyst.
4 CONCLUSION AND RESULTS
The patient had a smooth recovery after the surgery without any complications and is currently being regularly monitored. There was no recurrence after a 3-month follow-up period.
5 DISCUSSION
Different types of cystic masses can be found in the popliteal fossa, necessitating precise differentiation for treatment selection. Distinguishing between meniscal cysts, synovial cysts (Baker's cysts), and ganglionic cysts is crucial.1 MRI is reliable in detecting ganglion cysts as hyperintense lesions on T2-weighted images, with confirmation based on unique imaging characteristics.2 While histologic examination is essential for a definitive diagnosis, the management of ganglion cysts varies. Spontaneous resolution is possible, but interventions like aspiration and steroid injections may lead to high recurrence rates. Surgery is considered for persistent or severe cases, aiming for complete excision to minimize recurrence, with an estimated postoperative recurrence rate of 10%–15%.3
AUTHOR CONTRIBUTIONS
Faten Limaiem: Conceptualization; data curation; formal analysis; investigation; methodology; resources; supervision; validation; visualization; writing – original draft; writing – review and editing. Mohamed Amine Gharbi: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; resources; software; supervision; validation; visualization. Ramzi Bouzidi: Investigation; methodology; project administration; resources; software; supervision; validation; visualization.
ACKNOWLEDGMENTS
None.
FUNDING INFORMATION
We did not receive funding for this article.
CONFLICT OF INTEREST STATEMENT
None declared.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




