Behçet's disease presented with obscure gastrointestinal bleeding: A Palestinian case report
Abstract
Key Clinical Message
It is important to recognize and manage gastrointestinal symptoms in patients with BD, as they are linked to high rates of mortality and morbidity. BD can affect any part of the gastrointestinal tract, and prompt diagnosis and appropriate treatment are essential to prevent complications. Additionally, the diagnosis of BD is primarily based on clinical factors due to the lack of pathognomonic laboratory tests.
Behçet's disease (BD) is an idiopathic, chronic, and relapsing multi-systemic vasculitis characterized by recurrent skin lesions and eye disease. There is no pathognomonic laboratory testing; the diagnosis is made mainly on clinical factors. BD symptoms affecting the gastrointestinal (GI) system are particularly important as they are linked to high rates of mortality and morbidity. Although ileocecal involvement is most frequently mentioned, BD can affect any part of the GI tract. There are techniques for keeping track of disease activity during treatment, but they are not ideal. We present a case of a 38-year-old male patient admitted to the ICU with a history of black tarry stools of 1-month duration, fresh blood per rectum 5 to 7 times a day associated with fever, chills, and back and nonspecific joint pain for five days. The patient also experienced left eye episcleritis while being hospitalized, which was later confirmed to be BD.
1 INTRODUCTION
Behçet disease (BD) is an uncommon kind of recurrent systemic inflammatory vasculitis that is believed to happen after an autoimmune reaction to an infectious or environmental trigger in genetically predisposed individuals. Human leukocyte antigen (HLA)-B51 is considered the primary genetic risk factor in many patients.1 The disease can be found at any age but is most commonly found in adults between 20 and 40 years old. Both genders can be affected equally, with variable gender predominance in different countries.1 It's most prevalent in Eastern Asia and the Eastern Mediterranean, with the highest prevalence in Turkey (420: 100,000).1, 2
BD is a heterogeneous disease that can involve multiple systems. The recurrent mucocutaneous (oral and genital), ocular, and musculoskeletal manifestations are the most common manifestations to be seen. GI findings can only be found in less than 5% of cases.3 Behçet's disease symptoms affecting the GI system are particularly important since they are linked to high rates of mortality and morbidity due to various etiologies including GI bleeding. Even though ileocecal involvement is most frequently mentioned, BD can affect any part of the GI tract.3 Since BD is a clinically diagnosed disease, there are no specific laboratory, genetic, or imaging studies for it, and the inflammatory markers can be only mildly elevated. However, antisaccharomyces cerevisiae was higher in BD with GI involvement than in BD patients without GI manifestations.3, 4 The pathergy skin test is the only diagnostic test that can be used to diagnose the disease with high specificity and fair sensitivity.3, 5
The diagnosis of BD is based on clinical criteria. Since the 1990s, the International Study Group (ISG) criteria have been used as the main criteria for BD diagnosis.6 In 2004, Revised Japanese diagnostic criteria for BD were created.7 The International Criteria for BD (ICBD) was established in 2014 and included neurological and vascular manifestations.8 Our patient diagnosis was based on ISG criteria.6 In this case report, we present a patient with Behcet's disease with a rare manifestation of GI bleeding.
2 CASE REPORT
We present a case of a 38-year-old Palestinian male patient admitted to the intensive care unit (ICU) with a history of black tarry stools for one-month duration. Fresh blood per rectum 5–7 times a day along with fever, chills, and back and nonspecific joint pain for 5 days. He was also diagnosed with left eye episcleritis during his hospital admission in April 2022. The patient's history was also positive for known recurrent oral and genital ulcerations. Upon physical examination, the patient displayed superficial nonspecific tenderness and was alert and oriented, with normal cardiovascular, respiratory, neurological, and psychiatric examinations. Aside from well-controlled hypertension managed with amlodipine 5 mg once daily, his past medical history was unremarkable.
3 METHODS
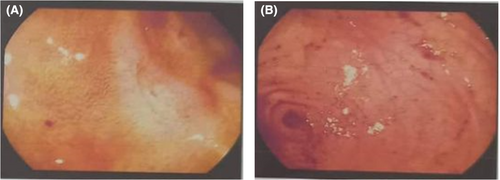
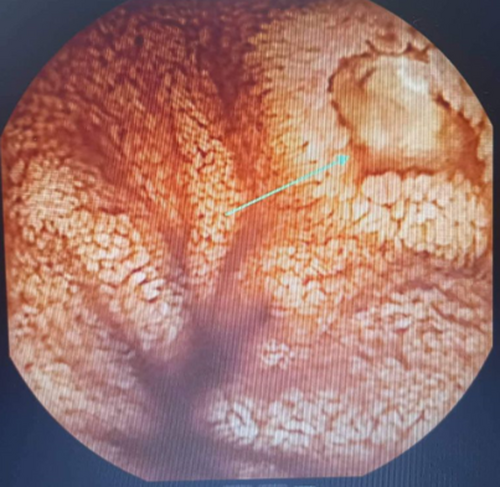
The patient underwent a CT scan with IV contrast of the abdomen and pelvis, as well as CT angiography, which yielded nonsignificant results. Upper endoscopy revealed a clean-based gastric ulcer measuring 12–15 mm (see Figure 1). A subsequent colonoscopy showed multiple clean-based ulcers in the terminal ileum and one in the cecum, with blood coming from the ileum (see Figure 2). Capsule endoscopy also revealed an ulcer in the terminal ileum (see Figure 3). Biopsy of the terminal ileum showed focal nonspecific inflammation with ulceration, without dysplasia, granuloma, or evidence of parasites, consistent with BD's typical pathological manifestations.

Upon admission, his hemoglobin was 6.96 g/dL (reference value for males: 13.5–17.5 g/dL), with a CRP level of 20.6 mg/dL (reference value for adults: 0.3–1.0 mg/dL). Other laboratory findings were normal, including MCV, white blood cell count, platelet count, serum electrolytes, blood urea nitrogen, creatinine, SGPT, SGOT, bilirubin, alkaline phosphatase, PT, PTT, and INR.
Following a rheumatology consultation, the patient was diagnosed with BD based on the ISG criteria. While in the hospital, he was started on 40 mg of prednisolone, azathioprine, and colchicine. He also received up to 5 units of packed red blood cells (PRBCs). Upon discharge, he was prescribed a tapering dose of prednisolone, azathioprine, colchicine, calcium 600 (one tablet twice a day), and vitamin D3 50,000 IU once weekly to manage his systemic, gastroenterological, and ocular symptoms.
4 RESULTS
In follow-up sessions at the end of 2022, he showed gradual improvement, with resolved GI bleeding and no tarry stool.
5 DISCUSSION
The GI manifestations of Behçet's disease are particularly significant because there is a high rate of morbidity and mortality associated with them. GI symptoms often appear between 4.5 and 6 years following the start of mouth ulcers.9 The most typical signs and symptoms include GI bleeding, diarrhea, nausea, vomiting, and abdominal pain.10 Although ileocecal involvement is most frequently mentioned, BD can affect any part of the GI tract or the different GI organs.9-11 There are two main types of intestinal Behçet's disease: mesenteric artery disease, which causes intestinal ischemia and infarction, and neutrophilic phlebitis, which causes mucosal inflammation and ulcer formation. GI involvement among BD sufferers is more common in some nations than others. Higher frequency has been reported in Japan (50%–60%) and the United Kingdom (38%–53%), while lower frequency has been reported in India (3.4%), Turkey (2.8%), and Saudi Arabia (4%), moderate frequency in Taiwan (32%) and China (10%) have reported higher frequency.12
Studies using video capsule endoscopy have revealed that BD can have an impact on the entire small bowel.13 The typical signs of intestinal BD are large (>1 cm), round or oval-shaped, deep ulcers in the ileocecal region. An important Korean study that demonstrated this found that 96% of the 94 patients with intestinal BD had damage to the terminal ileum, ileocecal valve, or cecum. Localized single ulcers made up 67% of the distribution patterns, and localized multiple ulcers made up 27%.14 Only 6% of the time did the colon show extensive and multisegmental involvement. Eighty-five percent of patients had one to six ulcers, with 67% having one and 18% having two to five. 76% of the ulcers were greater than 1 cm in diameter and had an average diameter of 2.9 cm. Round or oval shapes were the most prevalent (77%) shapes. Deep ulcers were more common, with a prevalence of 68% in deep ulcers compared to 38% in superficial ulcers. Rectal involvement occurs in less than 1% of BD patients, it should be noted.10 In our case, a terminal ileum ulcer was found during capsular endoscopy. A terminal ileum biopsy showed focal nonspecific inflammation with ulceration, without dysplasia, granuloma, or a parasite site, consistent with Behcet's illness.
Managing Behçet's syndrome can pose challenges due to the limited high-quality evidence available.15 Controlled studies have focused on managing ophthalmic disease, arthritis, and mucocutaneous disease, leaving a gap in knowledge regarding treatments for neurologic and vascular symptoms. Furthermore, there is a lack of widely recognized management guidelines for gastrointestinal BD. The Japanese Inflammatory Bowel Disease Research Group published several consensus statements in 2007 to standardize care. These statements were updated in 2014 to reflect growing low-level evidence in favor of anti-TNF-mAb therapy.16 Typically, intestinal BD has been treated using the same classes of medications as systemic BD, with a few exceptions. These medications include prednisolone, sulfasalazine, colchicine, immunomodulators, immunosuppressants, corticosteroids (CS), IFN, and anti-TNFa-antibodies treatment.15, 16 In one case, the patient experienced significant improvement in ocular, rheumatologic, and GI bleeding manifestations after using prednisolone, azathioprine, and colchicine.
AUTHOR CONTRIBUTIONS
Afnan W. M. Jobran: Writing – original draft; writing – review and editing. Abdelrhman Janem: Writing – original draft; writing – review and editing. Tareq Alhor: Supervision. Muhammad Idris: Data curation; resources. Mustafa Nabilsi: Data curation; resources. Salam Mughrabi: Data curation; resources. Aisha Alfakhry: Writing – review and editing. Hazem Ashhab: Supervision.
ACKNOWLEDGMENTS
None.
FUNDING INFORMATION
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST STATEMENT
None declared.
CONSENT
Complete written informed consent was obtained from the patient for the publication of this study and accompanying images.
Open Research
DATA AVAILABILITY STATEMENT
All the necessary data are available in the article itself.




