Papaverine effect on superficial vein in thumb replantation procedure: A case study
Abstract
Key Clinical Message
Topical papaverine is an effective vasodilator that can be used for dilating small veins to accept venous couplers for thumb replantation. This technique corrects size mismatches for successful venous anastomosis and minimizes postoperative complications.
Thumb replantation is a complex microsurgical procedure used to restore function and appearance after amputation. A successful venous anastomosis is essential in replantations; however, venous couplers can mismatch the size of veins and lead to obstacles. A 26-year-old male presented with a left thumb amputation caused by an electric saw injury. The amputated thumb was preserved and replantation surgery was performed 9 h post-injury. The digital artery and veins were repaired but a size mismatch was found between the only salvageable superficial vein (0.7 mm) and the smallest available venous coupler (1 mm). The vein was dilated to accept the coupler by a series of applications of topical papaverine (1 mg/mL). This allowed venous anastomosis to be accomplished in 25 min. Postoperative follow-up showed good thumb function, sensation, and circulation. Venous anastomosis is vital in thumb replantation to avoid venous congestion hence survival of the replanted thumb. Venous couplers shorten operative time and decrease the risk of postoperative complications. Papaverine is a vasodilator and facilitates venous anastomosis when veins and couplers are mismatched. This case demonstrates how papaverine, a vasodilator, may be used to improve surgical outcome during thumb replantation when small veins prevent venous coupler use.
1 INTRODUCTION
Thumb replantation is a complicated microsurgical procedure with the aim of restoring the functionality and appearance of a severed appendage. The bones and surrounding soft tissue must all be intricately reattached. A major component in thumb replantation is establishing a suitable connection between the vessels that supply the replanted thumb.1 The size mismatch between the veins and the venous coupler used for anastomosis can be a point of conflict in the venous anastomosis stage.2 Vasodilators, such as papaverine, can be utilized when the diameter of veins is smaller than that of the coupler in order to achieve a successful anastomosis.3 Papaverine, an alkaloid vasodilator produced from the opium poppy plant, has been used in a variety of surgical operations to increase blood flow and improve anastomotic results.3
In this case study, we explain how papaverine was administered as a vasodilator to widen a superficial vein with a diameter of 0.7 mm during thumb replantation with the goal of accommodating a 1 mm coupler while still ensuring satisfactory anastomosis.
2 CASE HISTORY/EXAMINATION
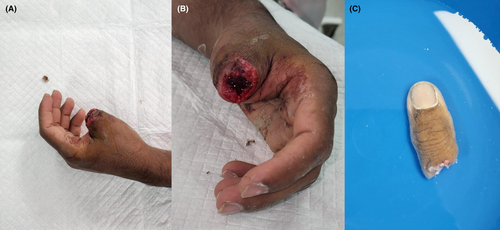
A 26 year old, previously healthy, male presented to the emergency department following an electric saw injury to the left thumb while cutting wood at work. His dominant hand is the right hand. No past medical or surgical history. Review of system was otherwise negative. He brought the amputated part with him and it was wrapped in wet gauze and placed in a container that was immersed in ice. On examination, he was vitally stable, primary and secondary survey were unremarkable except for the base of the left thumb amputation just distal to the metacarpophalangeal joint (Figure 1).
3 METHODS (DIFFERENTIAL DIAGNOSIS, INVESTIGATIONS AND TREATMENT)
X-ray of the hand showed amputated first proximal phalanx with residual bone fragment at the base (Figure 2). He was managed with IV amoxicillin/clavulanic acid (1000 mg q8hr) and IM tetanus toxoid; for the pain a digital block was done and he was given ketorolac and paracetamol. The patient was admitted under plastic surgery's service, and the surgery was performed 9 h after the amputation.

In the operating theater, the digital artery from the ulnar aspect was repaired with 9–0 nylon. The digital veins were badly crushed and only one small 0.7 mm vein was found on the dorsal aspect of the thumb, but since the smallest coupler size we had was 1 mm it was difficult to perform the anastomosis. A trial of topical papaverine, 1 mg/mL, was given to vasodilate the vein and after many cycles of papaverine in addition to mechanical dilation; the vein could accommodate the 1 mm coupler and anastomosis of the veins was possible within 25 min. One digital nerve was identified and repaired on the radial aspect. Flexor and extensor tendons were repaired with PDS thread, however the flexor tendon was shuttered badly. The bone was shortening by 0.5 cm from the proximal phalanx on the amputated side. Wound was closed with prolene and the coupler was covered with a small skin flap. The ischemia time was already 10 h before restoring circulation (Figures 3 and 4).


4 CONCLUSION AND RESULTS (OUTCOME AND FOLLOW-UP)
The patient was followed in the clinic for reassessment and wound care. Almost 2 months after the replantation, the patient was noted to have left thumb flexor pollicis longus (FPL) tendon rupture on examination. So secondary FPL tendon repair was done. Four months after the primary surgery the patient had good range of movement and function of the left thumb, his wounds were healed and he had good sensation and circulation (Figure 5). The patient was discharged from our care with full satisfaction.

5 DISCUSSION
Thumb replantation is an intricate procedure that necessitates venous anastomosis to prevent venous congestion in the attached appendage and eventual replantation failure.4 A meta-analysis published in 2018 evaluated the correlation between venous anastomosis and replant survival, they found that the higher the anastomosis number the higher the chance of survival. Zero versus one versus two anastomosis were evaluated, with two anastomosis showing a survival rate of 92.3% and 61.1% survival in zero anastomosis.5
Venous anastomosis can be achieved by either hand-sewn technique or the use of couplers. A meta-analysis published in 2020 looked at studies comparing coupler use versus hand-sewn technique in venous anastomosis; it reported anastomotic time and postoperative complications. Their results showed that the use of couplers when compared to hand-sewn venous anastomosis significantly decreased anastomotic time and postoperative failure risk, but it did not decrease postoperative venous thrombosis risk.2 In one study, time reduction from approximately 12 min with hand-sewn anastomosis to 3 min with a coupler was noted.6
One of the problems faced during the anastomosis phase of the replantation surgery is the post-traumatic vasospasm experienced by vessels in the zone of injury. Additionally, intraoperative vessels dissection and manipulation are also reasons for the narrowing of vessels. Vasospasm during microsurgery affects up 5%–10% of the procedures due to the aforementioned reasons. There are several ways to deal with this issue; some of which are: mechanical dilation, perivascular lidocaine injection, axillary block anesthesia, and systemic papaverine use.3
Papaverine was initially discovered in 1848 by Georg Merk.7 It is a phosphodiesterase (PDE) inhibitor commonly used in microsurgery. It antagonizes the PDE that breaks down cyclic guanosine monophosphate (cGMP) thus increasing the concentration of this second messenger within the vessel's smooth muscles, consequently inhibiting the effect of myosin light chain kinase and thus causing vasodilation.8 It is approved for the use in cerebral vasospasm, biliary duct spasms, and erectile dysfunction through its antispasmodic action on smooth muscles.9-11 One study looked at the time of action of papaverine in preventing vasoconstriction in response to phenylephrine and potassium (60 mmol/L); it showed that it reversed vasoconstriction for a maximum of only 1 h.12 Another study looked at the effect of preventing vasoconstriction on the radial artery during coronary artery bypass grafting (CABG) in vitro. The radial artery was pretreated with papaverine and prevention of vasoconstriction to norepinephrine was tested; results showed that the effect of papaverine was lost after 8 h.13
An article published in 2016 looked at the alternative drugs that can be given in the case of shortage of papaverine. Topical lidocaine and nicardipine (calcium channel blocker) were used as alternative antispasmodics and the rates of reexploration, complications, and flap salvage were compared when matched with papaverine controls. Results showed that there was no higher risk of flap loss or reoperation, making these drugs safe, and effective alternatives to papaverine.7 Other anti-spasmodic were studied in animal models; for example, PDE inhibitors (pentoxifylline, papaverine, and amrinone), calcium channel blockers (verapamil, nicardipine, nifedipine, and magnesium sulfate), local anesthetics (lidocaine), alpha antagonists (chlorpromazine and phentolamine), and direct vasodilators (prostaglandin E1, sodium nitroprusside, hydralazine, and nitroglycerin). However, to guide evidence-based management, well-controlled translational studies are required in order to reliably generalize the data.14
In our case, there was no salvageable vein for anastomosis except one superficial vein with a diameter of 0.7 mm and the smallest coupler size was 1 mm, so we gave the patient a trial of topical papaverine, 1 mg/mL, to vasodilate the vein. Several cycles were given in addition to mechanical dilation and finally the vein could accommodate the 1 mm coupler and anastomosis of the veins was possible in 25 min; 30% increment in the vein diameter was achieved. The coupler was covered with a small skin flap. Consequently, the thumb survived with no post-operative complications.
6 CONCLUSION
Thumb replantation is a difficult surgical technique that necessitates high precision and skills. Anastomosis of small diameter superficial veins can be difficult, and vasodilation may be required to allow the venous coupler to fit into it. The use of papaverine is safe and efficient to achieve sufficient vasodilation and allow for successful anastomosis. Nonetheless, as with any medication, the patient's existing comorbidities should be carefully evaluated before using papaverine. The effective application of papaverine in this example and the significant increment in the vein diameter demonstrates its potential value in microsurgery, particularly when vessels are small relative to that of the coupler.
AUTHOR CONTRIBUTIONS
Mahra AlSheryani: Writing – original draft. Ammar AlDhamin: Writing – review and editing.
ACKNOWLEDGMENTS
None.
FUNDING INFORMATION
No funding was received for conducting this study.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
ETHICS STATEMENT
This case report is not reviewed by the IRB as there are no identifying patient factors.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data supporting the findings in this case report is available within the article and its supplementary materials.




